Research Article
Challenges in Differential Diagnostic and Treatment of Cervical Root Resorption vs Root Caries
1Department of Cariology and Comprehensive Care, NYU College of Dentistry, New York, USA.
2Clinic 3AB-A, NYU College of Dentistry, New York, USA.
*Corresponding Author: Natalia Elson, Department of Cariology and Comprehensive Care, NYU College of Dentistry, New York, USA.
Citation: Elson N, Spielman R, Ameh G, Brandes I, Berkowitz L. (2023). Challenges in Differential Diagnostic and Treatment of Cervical Root Resorption vs Root Caries, International Clinical Case Reports and Reviews, BRS Publishers. 1(1); DOI: 10.59657/2993-0855.brs.23.001
Copyright: © 2023 Natalia Elson, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 13, 2023 | Accepted: June 27, 2023 | Published: July 01, 2023
Abstract
External cervical root resorption is often mistaken for root caries and vice versa. Radiological and clinical differential diagnosis of cervical root resorption and root caries is essential for both correct treatment planning as well as for the education and training of dental students. The aim of this article is to conduct a literature review and to summarize the prevailing professional consensus pertaining to external root resorption and to establish a proper clinical diagnostic and treatment protocol which help students distinguish cervical root resorption from root caries, and thereby manage it appropriately. This is critical because unlike external root resorption, the etiology of caries is predominantly bacterial and thus requires radically different treatment modalities. Early and correct diagnosis of cervical root resorption would prevent unnecessary removal of tooth structure to access what would otherwise be treated as a carious lesion. Following an overview of etiology, classification and diagnostic methods, we will propose a treatment approach a dental school clinical setting to improve education for students and provide better care for patients by means of a minimally invasive approach.
Keywords: bio dentine; cervical root resorption; MTA; root caries; trichloroacetic acid
Definition
Non-infectious loss of hard and soft tissue (root cementum and/or dentin) due to osteoclastic activity. The cause varies (see classification); the condition is usually asymptomatic; the outcome is mostly loss of tissue or tooth; the treatment is palliative and always reactive, never predictive. Currently there is no standardly accepted management. According to the Glossary of the American Association of Endodontists, resorption is defined as a condition associated with either a physiologic or a pathologic process resulting in loss of dentin, cementum or bone [1, 2].
Introduction
Root resorption is a condition that is frequently misdiagnosed or only incidentally found in a clinical setting. Cervical tooth resorption is often mistaken for caries. Some resorptions are self-limiting or require monitoring only, others require more extensive management, even including endodontic treatment. Currently, there are is a substantial body of publications describing etiology, classification and treatment approaches [3].
However, it is the goal of the authors to create a clinical approach that will assist clinicians and dental students in correct diagnosis of this condition and thus prevent unnecessary removal of tooth structure. Cervical tooth resorption seems to be somehow related to anatomical variations in the cementoenamel junction (CEJ) [4,5]. Due to such physiological diversity (see Table 1), care must be taken when performing any interventions in the cervical region of the tooth because this may inadvertently alter the morphology of this region and induce pathological processes and/or hypersensitivity. Usually located in the supracrestal area and generally covered by soft tissue, the CEJ produces hard scraping sound when examined by explorer.
Table 1: Types of CEJ Morphologies and their relative frequencies.
| Type of cementoenamel junction | Frequency (%) | |
| Type I | Cementum Overlapping Enamel | 33.30% |
| Type II | Enamel Overlapping Cementum | 13.30% |
| Type III | Cementum and Enamel Abut Without Overlap | 36.70% |
| Type IV | Gap Between Cementum and Enamel | 16.70% |
Etiology of Resorption
The etiology of any resorption will ultimately determine the treatment and management protocol. Although the cause of resorption is not fully understood, there is general agreement among researchers that different types of traumas may trigger the start of the resorption process. In particular, damage to the periodontal ligament can induce an immune response, resulting in the osteoclastogenesis [6,7].
Physical Trauma
- Occlusal trauma
- Scaling and root planing
- Orthodontic treatment
- Bruxism
- Intracoronal restorations
Chemical Trauma
Internal bleaching (30% hydrogen peroxide can pass through the dentinal tubules and provoke an immunologic response). Sodium perborate might be a safer alternative as a "walking bleach" agent. Other co-factors play an important role in the resorptive process:
- Endodontic microbes and their toxins can pass through the dentinal tubules to periodontal tissue
- Developmental factors: cementum hypoplasia, dentinal hypoplasia, dentin hypocalcification
- Neoplasia (benign or malignant)
- Hormonal (hyperparathyroidism, Gaucher’s disease)
- Hyperoxaluria and oxalosis
- Genetic predisposition
- Systemic sclerosis
- Feline herpes virus type 1
- Varicella Zoster virus
- Hepatitis B virus
- Bisphosphonates
Special attention should be paid to multiple idiopathic cervical resorption which first was reported by Mueller and Rony in 1930. This type of resorption occurs spontaneously without common initiating factors, affects more than one tooth, and is primarily seen in young females. Though it is debated, some researchers have proposed some predisposing factors such as tooth transplantation, guided tissue regeneration, use of tetracycline for root surface conditioning, and orthognathic surgery [8,9].
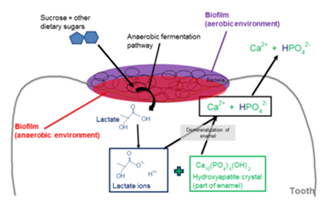
Mechanism of Dental Caries
Dental caries is a bacterial disease process that starts when certain types of bacteria commonly found in the oral cavity produce acidic by products from the metabolism of fermentable carbohydrates. These acids then leach the mineral content out of the enamel and dentin, causing them to dissolve. The caries process is a continuum resulting from many cycles of demineralization and remineralization. Demineralization begins at the atomic level on the crystal lattice structure inside the enamel or dentin and continues unless halted, eventually culminating in a tissue cavitation.
Figure 1: Mechanism of resorption.
A group of researchers from University of Pennsylvania School of Dental Medicine recently published their findings regarding caries
"A cross-kingdom partnership between bacteria and fungi can result in the two joining to form a ‘superorganism’ with unusual strength and resilience. It may sound like the stuff of science fiction, but these microbial groupings are very much part of the here and now.” This synergism between Streptococcus mutans and Candida albicans causes more extensive tooth decay [10].
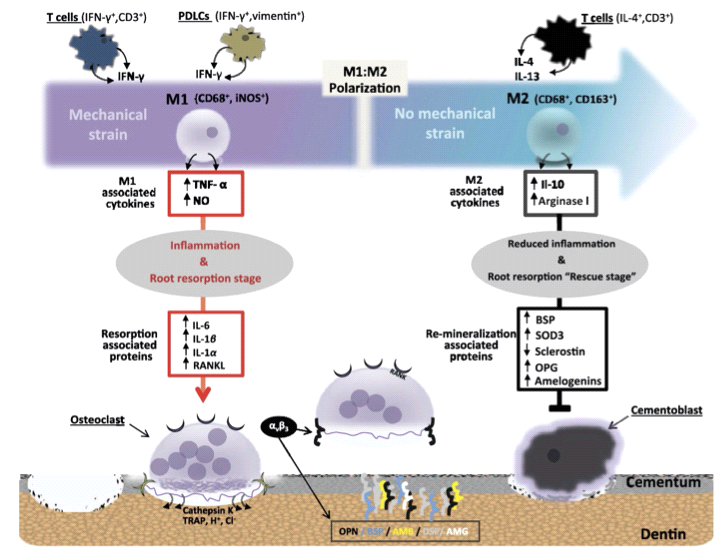
Figure 2: Cellular and molecular pathways leading to external root resorption (J. Dent. Res. 2017).
Mechanism of Resorption
"Clastic" cells (J. Andersen) are derived from hematopoietic stem cell precursors, namely monocytes. They are stimulated by prostaglandins and cytokines to migrate toward resorption sites where they form into the mature multinucleated osteoclasts. Mineral and organic components are degraded both extra- and intracellularly through exocytosis and phagocytosis. Hydrogen ion release produces pH levels of around 4.75. In the most advanced cases after mechanical or chemical trauma at the cementoenamel junction, mostly seen in Type IV, external cervical resorption (ECR) can progress inwards with or without pulpal involvement. Cementum gets replaced by granulation tissue followed by inflammation of the periodontium caused by lymphocytes, polymorphonuclear leukocytes and plasma cells. In contrast, root caries is identified as a decayed soft lesion associated with gingival recession. Radiographically it appears an ill-defined, radiolucent patch [11,12].
Table 2: Pulp is involved in advanced cases.
| Differential Diagnosis of Crr & Root Caries | ||||
| Lesion | Etiology | Radiology | Clinical Evaluation | Treatment |
| Caries | Bacterial Metabolism | Ill-defined radiolucency, detected via conventional radiographs | Sticky on probing Pulp tests normal | Removal of decay & restoration Extraction if tooth is unrestorable |
| Resorption | Trauma Bacteria Idiopathic | Asymmetric radioluncency with irregular margins in cervical region, mottled appearance, possible intrabony defect, detected via conventional radiographs or, ideally, CBCT. | Hard mineralized with sharp edges Pulp test normal* "Pink Tooth" | Periosteal flap and curettage & restoration Extraction if tooth is unrestorable |
Diagnosing pulpal condition is quite important to establishing future treatment plan. The best diagnostic pulp vitality test is laser Doppler flowmetry (LDF) which is not practical in a dental school clinical setting.
Classifications
Root resorption in permanent teeth (Kanas and Kanas, 2011) is classified:
Internal-originating in the pulp (relatively rare) due to trauma or inflammation of the pulp.
External-originating in the periodontal ligament due to:
- infection/inflammation
- traumatic injuries
- pressure/mechanical insult
- neoplastic conditions
- systemic disorders
- idiopathic.
Picture 2: Tooth 10 (year 2018).
Picture 3: Tooth 10 (year 2022) Patient was diagnosed with Gaucher disease.
Internal Root Resorption (IRR): this is relatively uncommon and most studies are based on case reports. Histologically, we observe destruction of intraradicular dentin and dentinal tubules, sometimes accompanied by repair with bone and/or cementum-like tissue close to the site of resorption. Neither imaging nor histological evaluation of such cases can shed light on the cause or the aftermath of the root resorption. Case descriptions in the literature do not provide any means to predict future cases or definitive treatment options for existing cases (Patel et al., 2010, Patel et al., 2022). [13,14].
External Root Resorption (ERR): this pathology can be classified in at least 16 ways (reviewed in Aidos et al., 2018 and Abbott and Lin, 2022). The simplest and most widely used is the classification described by Andreasen in 1970. Andreasen’s classification divides root resorption into:
- internal resorption of two types: replacement and inflammatory;
- external resorption of three types: surface, replacement, and/or inflammatory [15,16].
The Andreasen classification appears to have gained wide acceptance for its simplicity and is quoted by various recent authors. However, the Kanas classification is the most complete and is based on localization, etiology, and type (Kanas & Kanas, 2011). Other authors have suggested a classification system based on location, physiology, and pathology (Abbott and Lin, 2022).
This latter classification is more thorough and logical:
Internal
- Internal surface resorption.
- Internal inflammatory resorption.
- Internal replacement resorption.
External
- External surface resorption.
- External inflammatory resorption (apical or lateral).
- External replacement resorption (transient or progressive).
- External invasive resorption.
- External pressure resorption.
- Orthodontic resorption.
- Physiological resorption.
- Idiopathic resorption.
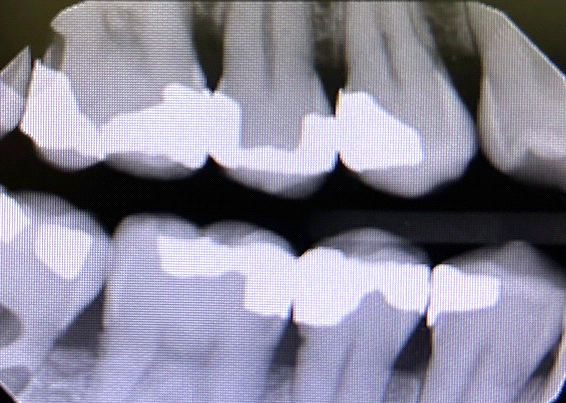
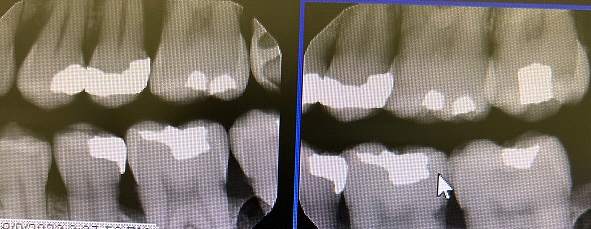
Picture 4: External Cervical Resorption Teeth 23 and 25.
Picture 5: Cervical resorption Teeth 29, 30 and 4.
Picture 6: Cervical resorption. Teeth 4, 5, 12, 13, 18, 19 and 20.
Picture 7: Root caries Tooth 12.
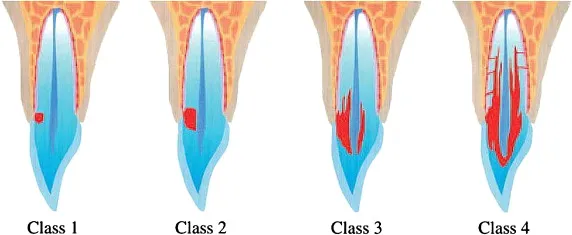
Clinical classification (Heithersay)
Class 1: Small invasive resorptive lesion with shallow penetration into dentin.
Class 2: Well-defined invasive resorptive lesion, can penetrate close to the pulp chamber and shows little or no extension into radicular dentin.
Class 3: Deeper invasion into dentin, extending to the coronal third of root.
Class 4: Large invasive lesion extending beyond the coronal third of the root canal.
(Class 1 and Class 2 tissue are fibrovascular in nature whereas Class 3 and Class 4 tissue are fibro-osseous) [17,18,19].
Figure 3
Role of microorganisms in Cervical Resorption
Inflammatory cervical root resorption occurs when bacteria from an infected root canal pass through the dentinal tubules to the cementum and trigger external root resorption [20,21]. In a chronic case, the tooth is asymptomatic. However, if the infection is acute, the patient typically experiences pain on percussion and swelling. Radiographically, the lesion presents as a bowl-shaped resorptive lesion on the root surface with attendant pathological changes in the surrounding bone tissue. One of the key challenges in managing this condition is to establish the proper treatment approach and protocol. In more recent publications, Ledermix™ paste and calcium hydroxide are suggested to stop clastic activity by transporting corticosteroids and antibiotics from the pulp to external root surfaces. Microbiotas of periodontal and endodontic infections in patients with active disease are quite similar. Due to multiple reports about the role of yeast species (Candida) and hypoxic environments created by enzymes and interleukins, research efforts should be particularly focused toward creating new medications to address this issue [22,23].
Table 3
| Microflora | Root caries | External Cervical Resorption |
| Aggregatibacter actinomycetemcomitans | Yes | No |
| Prevotella intermedia | Yes | Yes |
| Tannerella forsythia | Yes | Yes |
| Porphyromonas gingivalis | Yes | Yes |
| Candida albicans | Yes | Yes |
| Treponema denticola | Yes | Yes |
| Epstein-Barr Virus | No | Yes |
| Human Cytomegalovirus | No | Yes |
| Herpes Virus spp. | No | Yes |
| Archaea | No | Yes |
Management of External Cervical Root Resorption
Management of External root resorption can be based on the type of resorption and the etiology, whether it is caused by trauma or by infection. The treatment management protocol, therefore, depends on the severity, access, and location of the resorption. The objectives of treatment are broadly categorized into preventive care and therapeutic management [24].
The clinician can apply one of the following:
- Monitoring, no treatment
- Treatment external root surface
- Endodontic approach
- Combination: external and internal treatment [25].
According to the authors of this paper, the management of ECR is dependent on accessibility. Successful management of external cervical resorption will require correct and accurate diagnosis of the lesion, with current diagnostic accuracy favoring the use of Cone Beam CT. The authors have stated that when ECR is present in a vital pulp and limited to the coronal third of the root, a mucoperiosteal flap will be needed to gain access to the lesion where adequate curettage of the granulomatous tissue can be done for both the root and periodontal tissue [26,27]. Topical application of trichloroacetic acid (TCA) may also be done on the surface of the lesion to permeate tissues and arrest the resorptive process especially in channels that are not accessible to mechanical debridement. However, TCA may cause irritation to the skin and oral mucosa.
In order to counteract this, topical glycerol can be applied to the areas adjacent to the lesion. Restoration should be done using glass ionomer cement or composite material. The use of Bio dentine and other bioactive restorative materials such as MTA have also been proposed. This latter choice offers excellent aesthetics and promotes adhesion to the PDL. Endodontic therapy was also suggested for lesions that have perforated the root canal system and/or exhibit symptoms of irreversible pulpitis. The root canal should be obturated to prevent communication with the PDL space. This must be accompanied by corresponding use of mechanical debridement for the external cervical lesion. Patel et al. have also suggested intentional reimplantation as a possible treatment of the lesion [28]. This paper suggests the use of preventive therapy for the management of trauma induced inflammatory resorption. To that end, it proposes various pharmaceutical interventions such as antibiotics, corticosteroids, calcium hydroxide and Ledermix.
- Antibiotics: Intracanal medicament and systemic tetracycline. This approach is bacteriostatic, and inhibits both osteoclastic resorption as well as collagenases.
- Corticosteroids: In a randomized clinical trial where the roots of extracted teeth were covered with dexamethasone, it was found to result in over 70% less resorption.
- Calcium Hydroxide: This approach is less desirable because it can cause resorption on its own.
- Ledermix™: This is a prescription paste featuring demeclocycline (antibiotic) and triamcinolone (corticosteroid) for intracanal medication [29].
This was a case report in which the authors suggest the use of platelet rich fibrin in the canal following endodontic therapy and the use of MTA Plug. They also used a low intensity antimicrobial photodynamic therapy which basically irradiates all surfaces of the tooth with a fibreoptic tip at a wavelength of 670nm. This is accompanied with the application of photosensitizer within the periodontic ligament space [30].
Characteristics of Materials and Methods Used for Treatment of Cervical Resorption
MTA (Mineral Trioxide Aggregate)
MTA was developed by Torabinejad in 1993.The beneficial features are biocompatibility, bioactivity, hydrophilicity, sealing ability, and low solubility. It is typically used for perforation repairs, apexification, root-end filling, obturation, tooth fracture repair, regenerative procedures, apexogenesis, pulpotomies, and as a pulp-capping material [31].
Bio dentine®
The powder component of this material consists of tricalcium silicate, dicalcium silicate, calcium carbonate and oxide filler, iron oxide shade, and zirconium oxide. Tricalcium silicate and dicalcium silicate are indicated as the primary and second core materials, respectively, whereas zirconium oxide serves as a radio pacifier. The liquid contains calcium chloride as an accelerator and a water-soluble polymer that serves as a water reducing agent. The material is characterized by the release of calcium when in solution Tricalcium silicate-based materials are also defined as a source of hydroxyapatite when they are in contact with synthetic tissue fluid.
Calcium Hydroxide
Calcium hydroxide was originally introduced to the field of endodontics by Herman in 1930 as a pulp-capping agent, but its use today has spread beyond merely endodontic therapy. It is the most commonly used dressing for treatment of a vital pulp. It also plays a major role as an interim dressing in the disinfection of the root canal system. It has been shown that the dissociation coefficient of calcium hydroxide of 0.17 permits a slow, controlled release of both calcium and hydroxyl ions which can diffuse through the dentinal tubules. Tronstad et al. demonstrated that untreated teeth with pulpal necrosis had a pH of 6.0~7.4 in the pulpal dentin and periodontal ligament, whereas, after calcium hydroxide had been placed in the canals, the teeth showed a pH range in the peripheral dentin of 7.4~9.6.
Trichloroacetic acid
90% aqueous trichloroacetic acid (TCA) may be applied to the resorptive cavity to promote coagulation necrosis of this tissue as it penetrates the smaller, more inaccessible recesses and resorptive channels which may not be identified and debrided by mechanical instrumentation alone." (Heithersay 1999, Schwartz et al. 2010). Care must be taken when using TCA due to the potential irritation it may inadvertently cause following contact with the oral mucosa and/or skin. A small cotton pledget or microbrush should be dipped into TCA and then gently pressed to remove excess liquid before carefully applying it to the resorptive site until coagulation necrosis occurs (usually within 3~4 minutes). The areas immediately adjacent to the ECR defect may be protected by application of glycerol and single tooth isolation or split dam technique to prevent inadvertent contact by the TCA with the adjacent tissues (Heithersay & Wilson 1988, Heithersay 1999). Alternatively, 3~5% sodium hypochlorite may be used in a fashion similar to TCA. Undermined dentin and enamel should be removed with a bur in a high-speed surgical handpiece [32].
Ledermix™ paste
Ledermix™ paste is a non-setting, water-soluble paste material for use as a root canal medicament or as a direct or indirect pulp capping agent. The release and subsequent dentinal diffusion characteristics of triamcinolone from Ledermix™ paste when used as a root canal medicament have been investigated under different conditions. Several such studies show that triamcinolone is released from the Ledermix™ paste in the root canal and can reach the systemic circulation via diffusion through the dentinal tubules, lateral canals, and the apical foramen. After the first 24 hours, 30% of the triamcinolone was released. By the end of 14 weeks, the remaining 70% had been released. Immediate intracanal placement of Ledermix has been studied for reimplanted teeth because it has been shown to inhibit root resorption after an extended drying time. In a recent study done in dogs, the groups treated with Ledermix, triamcinolone and demeclocycline had significantly more favorable healing and more remaining root structure than the group filled with gutta-percha and sealer only.
Calcitonin
Calcitonin is a known inhibitor of osteoclastic bone resorption that also regulates human odontoclastic activity, particularly during the physiological process of root resorption. It is a naturally occurring polypeptide hormone which can be used as an intracanal medication with the ability to diffuse through the dentinal tubules to inhibit clastic cells. Despite some promising research results, it is not yet available for commercial use in Dentistry [33].
Hydraulic calcium silicate-based materials
BioRoot™ RCS (Septodont, Saint-Maur-des-Fossés, France), MTA Fillapex® (Angelus, Londrina, Brazil), EndoSequence® BC Sealer™, (Brasseler USA, Savannah, GA, USA). Various ions are known to have different effects in the context of the oral cavity. For example, Si4+ and Ca2+ promote biomineralization, while OH- ions increase the pH in the environment and possess antimicrobial properties.
Proposal for a Diagnostic and Treatment Protocol in Dental School Clinics
A series of integrated lectures explaining the etiology, differential diagnoses and treatment protocols should be implemented in the curriculum of D2 and D3 students.
Diagnosis of external root resorption
1. Medical and dental history including questions about:
- dental trauma
- orthodontic treatment
- TMJ problems
2. Radiographs: vertical BWs and any necessary PAs
3. Percussion, palpation and vitality testing of teeth with both carious/non-carious lesions
4. Microbiological assay salivary test
5. Periodontal charting of all teeth in both arches
6. Intraoral clinical evaluation of tooth lesion using a periodontal probe (dull end)
Treatment of external cervical tooth resorption
Dependent on any findings:
1. Occlusion equilibration (if necessary)
2. Orthodontic treatment (if necessary)
3. Monitoring (6 months recall)
4. Flap surgery (cooperation with periodontal faculty), debridement of lesion if indicated, filling the lesion using biocompatible material (MTA, Biodentine®, GIC, composite, etc.)
5. Endodontic treatment depending on extent of lesion
6. Periodontal therapy and maintenance
7. Patient education including oral hygiene instruction.
8. Implementation of laser treatment (different laser wavelengths are capable of removing soft tissue, killing bacteria, achieving hemostasis, promoting healing and reducing post-operative pain and swelling) [35].
Conclusion
Tooth resorption is frequently misdiagnosed and improperly treated. To avoid misdiagnosis and mismanagement of resorptive dental tissue, clinicians should be educated and aware of these conditions. Careful attention to the location of resorbing tissue, their clinical and radiographic appearance, and the presence of any etiologic agents can assist with accurate detection, diagnosis and management. Multiple studies and histological results have shown that microorganisms are identified only at the outer layers of lesions. However, microbes can trigger or promote resorptive processes. Cervical resorption is found only accidently in most cases. For this reason, recall exams play a critical role in diagnosis, monitoring and treatment of this condition. In the early stages, the tooth is asymptomatic and the lesion can easily be mistaken for root caries. If diagnosed in time, the prognosis is generally favourable and the tooth can usually be saved. In the case of pulpal involvement, restoration of the tooth requires access followed by root canal therapy [36]. Treatment of periodontal disease, traumatic occlusion management and patient education are crucial to achieving good results and optimistic prognoses. In the case of idiopathic tooth resorption, or generalized tooth resorption, consultation with a primary care doctor is a must. Correct differential diagnosis between root resorption and root caries can help avoid unnecessary removal of tooth structure by establishing the appropriate treatment approach ab initio. Using new diagnostic methods and equipment, we can achieve better results. Our recommendation to dental schools is to include additional resources in their respective curricula, calibrate faculty, collaborate with dental and medical specialists, educate students, and provide the best treatment options for patients by using minimally invasive dentistry.
References
- S. PateL, A. M. Mavridou, P. Lambrechts, & N. Saberi. (2018). External cervical resorption-part 1: histopathology, distribution and presentation, International Endodontic Journal, 51(11):1205-1223.
Publisher | Google Scholor - Brooke Blitcher. (2021). Differentiating Resorption, American Association of Endodontists.
Publisher | Google Scholor - V.Yu. Bakhareva, E.G. Margaryan, E.I. Selifanova, I. M. Makeeva. (2021). Research on Microflora and The Qualitative Composition of Periodontal Pathogens by PCR method in Patients with Root Caries and External Cervical Resorption, Journal of Stomalogiia, 100(6):19-23.
Publisher | Google Scholor - H. Aidos, P. Diogo, J.M. Santos. (2018). Root Resorption Classifications: A narrative Review and a Clinical Aid proposal for Routine Assessment, Eur Endod Journal, 3:134-145.
Publisher | Google Scholor - Lilian Neuvald, Alberto Consolaro. (2000). Cementoenamel Junction: Microscopic Analysis and External Cervical Resorption, Journal of Endodontics, 26(9):503-508.
Publisher | Google Scholor - PV. Abbot. (2016). Prevention and Management of External Inflammatory Resorption following trauma to teeth, Australian Dental Journal, 61:(S1):82-94.
Publisher | Google Scholor - Marina Fernandes, Ida de Ataide, Rahul Wagle. (2013). Tooth Resorption part II- External Resorption: Case series, Joural Concerative Dentistry, 16(2):180-185.
Publisher | Google Scholor - Emily Y. Chu, Brian L. Foster, Evlambia Hajishengallis, Martha J. Somerman, Vivek Thumbigere-Math. Multiple Idiopatic Cervical Root Resorption: A Challenge for a Trandisciplinary Medical-Dental Team.
Publisher | Google Scholor - Katarina Mikuskova, Peter Vanuga, Katarina Adamicova, Dagmar Statelova, Maria Janickova, Igor Malachovsky, Tomas Siebert. (2022). Multiple Idiopathic external cervical root resorption in patients treated continuously with denosumab; case report, BMC Oral Health, 22:129.
Publisher | Google Scholor - Xiuqin Chen, Eric Banan-Mwine Daliri, Namhyeon Kim, Jong-Rae Kim, Daesang Yoo, Deog-Hwan Oh. (2020). Microbial Etiology and Prevention of Dental Caries: Exploiting Natural Products to Inhibit. Cariogenic Biofilms, Pathogens, 9(7):569.
Publisher | Google Scholor - Henrique Aidos, Patrícia Diogo, and João Miguel Santos. (2018). Root Resorption Classifications: A Narrative Review and a Clinical Aid Proposal for Routine Assessment, Eur Endod J. 3(3):134-145.
Publisher | Google Scholor - Ashraf F. Fouad. (2019). Microbiological Aspects of Traumatic Injuries, Dental Traumatology, Wiley, 45(12):S39-S48.
Publisher | Google Scholor - Stacey L. Gividen. (2016). Endodontics reference guide: Distinguishing differences between internal and external resorption.
Publisher | Google Scholor - Mario Dioguardi, Vito Crincoli, Luigi laino, Mario Alovisi, Diego Sovereto, Lorenzo Lo Muzio, Giuseppe Troiano. (2020). Prevalence of Bacteria of Genus Actinomyces in Persistent Extraradicular Lesions-Systematic Review, Journal of Clinical medicine, 9(2):457.
Publisher | Google Scholor - Marina Polonsky. (2022). Invasive Cervical Resorption: A Dental Pandemic or an Auto-immune Disease of the Mouth?, Journal of Oral Health.
Publisher | Google Scholor - Robert J. Kanas, Scott J. Kanas. Dental Root Resorption: A review of the Literature and a Proposed New Classification, Compendium, 32(3).
Publisher | Google Scholor - GS Heithersay. (2007). Management of Tooth Resorption, Australian Dental journal, 52:(S1):S105-S121.
Publisher | Google Scholor - Artak Heboyan, Anna Avetisyan, Mohmed Isaqali Karobari, Anand Marya, Zohaib Khutshid, Dinesh Rokaya, Muhammad S. Zafar. (2022). Gustavo Vicentis de Oliveira Fernandes Tooth Resorptio: A review, Science Progress, 105(3):1-29.
Publisher | Google Scholor - Luiz Chavez De Paz. (2004). Gram-positive organisms in Endodontic infections. Endodontic Topics. 9(1):79-96.
Publisher | Google Scholor - Marina Fernandes, Ida de Ataide, Rahul Wagle. (2013). Tooth Resorption part II- External Resorption: Case series, Joural Concerative Dentistry, 16(2):180-185.
Publisher | Google Scholor - Shanon Patel, Navid Saberi, Tiago Pimental, Peng-Hui Teng. (2022). Present Status and Future Directions: Root Resorption. International Endodontic Journal, Wiley, 55(S4):892-921.
Publisher | Google Scholor - A.Iglesias-Linares, J.K.Hartsfield Jr. (2017). Cellular amd Molecular Pathways Leading to External Root Resorption. Journal of Dental Research, 96(2):145-152.
Publisher | Google Scholor - Ozlem Malkondu, Meriç Karapinar Kazandag, Ender Kazazoglu. (2014). A Review on Biodentine, a Contemporary Dentine Replacement and Repair Material, BioMed Research International.
Publisher | Google Scholor - Olivia Rotondi, PhiAnhWaldon, Sahng G. Kim. (2020). The Disease process, Diagnosis and Treatment of Invasive Cervical Resorption: A Review, Dentistry Journal, 8(3):64.
Publisher | Google Scholor - Nizar Ahned, Bejoy Mony, Harinath Parthasarthy. (2014). External cervical resorption case report and a brief review of literature, J Nat Sci Biol Med, 5(1):210-214.
Publisher | Google Scholor - G.S. Heithersay. (1996). External Root Resorption Part I, Australian Endodontic Newsletter, External Root resorption Part II, 22(3):33-37.
Publisher | Google Scholor - Kivanc Kamburoglu, Sebmem Kursun, Selcen Yuksel, Bengi Oztas. (2011). Observer Ability to Detect Ex Vivo Simulated Internal or External Cervical Root Resorption, Americal Association of Endodontists, 37(2):168-175.
Publisher | Google Scholor - T.M.T. Waltimo, B.H. Sen, J.H. Meurman, D. Osstavik, M.P.P Haapasalo. (2003). Yeasts in Apical Periodontitis, Crit Rev Oral Biol Med, 14(2):128-137.
Publisher | Google Scholor - Paul V. Abbott, Shaul Lin. (2022). Tooth Resorption-Part 2: A Clinical Classification, Dental Traumatology, Wiley, 38(4):267-285.
Publisher | Google Scholor - Farah Y. Eid, Walid A. El-Kenany, Mohamed I. Mowafy, Ahmed R. El-Kalza. (2022). The Influence of two photobiomodulation protocols on orthodontically induced inflammatory root resorption (a randomized control clinical trial), BMC Oral Health, 22:221.
Publisher | Google Scholor - Masoud Parirokh, Mabmoud Torabinejad. (2010). Mineral Trioxide Aggregate: A Comprehensive Literature Review- Part III: Clinical Applications, Drawbacks, and Mechanism of Action, Elsevier Inc, 36(3):400-413.
Publisher | Google Scholor - S. Patel, F. Foschi, F. Mannoci& K. Patel. (2018). External cervical resorption: a three-dimensional classification, International Endododntic Journal, 51(2):206-214.
Publisher | Google Scholor - Athina M. Mavridou, Esther Hauben, Martine Wevers, Evert Schepers, Lars Bergmans, Paul Lambrechts. (2018). Understanding External Cervical Resorption in Vital Teeth, Journal of Endodontics, 42(12):1737-1751.
Publisher | Google Scholor - Marina Fernandes, Lilian Menezes, Ida De Ataide. (2017). Management of invasive cervical resorption using a surgical approach followed by an internal approach after 2 months due to pulpal involvement, J Conserv Dent, 20(3):214-218.
Publisher | Google Scholor - Zvi Fuss, Igor Tsesis, Shaul Lin. (2003). Root resorption-diagnosis, classification and treatment choises based on stimulation factors, Dental Traumatology, 19(4):175-182.
Publisher | Google Scholor - Asgeir Sigurdsson, Noah Chivian. (2011). The Role of Endodontics After Dental Traumatic Injuries, Book Chapter, Cohen’s Pathways of the Pulp (Tenth Edition).
Publisher | Google Scholor