Case Report
Chagas Disease in Children-Case Report
- Alicia Santa Cortes Gonzalez 1*
- Veronica Garcia Torres 1
- Maria Patricia Ramos Gonzalez 1
- Rodolfo Ramirez Robles 2
- Mariana Guerra Estevez 2
- Diana Cristina Mancisidor Carreras 2
- Alberto Hernandez Mota 3
1Pediatrician, Mexican Institute of Social Security, University Veracruzana, Xalapa Veracruz, Mexico.
2Doctor Pediatrics First-Year Resident, Institute Mexican Social Security University, Veracruzana, Xalapa Veracruz, Mexico.
3Family Physician, Mexican Institute of Social Security, Universidad Veracruz, Xalapa Veracruz, Mexico.
*Corresponding Author: Alicia Santa Cortes González, Pediatrician, Mexican Institute of Social Security, University Veracruzana, Xalapa Veracruz, Mexico.
Citation: A.S.C. Gonzalez, Veronica G Torres, M.P.R. Gonzalez, Rodolfo R Robles, Mariana G Estevez, et al. (2023). Chagas Disease in Children-Case Report. International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(2); DOI: 10.59657/2837-8172.brs.23.015
Copyright: © 2023 Alicia Santa Cortes Gonzalez, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 05, 2023 | Accepted: May 25, 2023 | Published: June 10, 2023
Abstract
Chagas disease, caused by Trypanosoma cruzi, is considered the most serious parasitosis in America. It is mainly transmitted by triatomics (bugs). The infection causes cardiomyopathies and mega organs of the digestive tract. The diagnosis in the acute phase is by parasitological approach and in the chronic phase, by laboratory screening studies. In Mexico, children under 10 years of age are the most affected. The case of a 12-year-old girl with data suggestive of a bacterial infectious process is reported. with persistent fever, multi-treated with antimicrobials with suspicion of Chagas disease through the route of entry of the parasite with the Romana-Mazza sign.
Keywords: trypanosome cruzi; chagas disease; sign of romana-mazza; parasitemia
Introduction
Trypanosomiasis or Chagas disease is considered the most serious parasitosis in America and is one of the 14 lagging diseases on the World Health Organization list [1]. Mexico is an endemic country for Chagas disease, where two thirds of the territory can be considered at risk of vector transmission, that is, 1,100,000 individuals could be infected with Trypanosoma cruzi and 29,500,000 at risk of contracting the infection [2,3], the states with the highest incidence were Veracruz, Morelos, Oaxaca, Yucatán, Chiapas, Guerrero and Jalisco [4,5] Children under 10 years of age are the most Affected, approximately 75% present signs and symptoms related to the route of entry of the parasite with non-specific systemic manifestations, mainly fever; in 50% of cases, when the entry route is close to the ocular mucosa, the ophthalmoganglionic complex or Romaña-Mazza sign is presented, which consists of unilateral bipalpebral edema of a slightly pruritic violaceous color accompanied by regional adenopathies [5,10]. The demonstration of the presence of the parasite constitutes the diagnosis of certainty; however, it is only possible to detect the blood form during the acute phase of the infection by visualizing the parasite by different methods. In Mexico it is considered a public health problem since an estimated 1.1 million people are infected. The mortality rate in 2016 was 0.02 for men and 0.01 for women.
Clinical Case
A 12-year-old female with no significant history of her current condition, began her condition seven days after she was admitted to the emergency department, presenting a sensation of a foreign body in her right eye and conjunctival hyperemia. She went to a private doctor prescribing ophthalmic antibiotics and oral analgesics without improvement, two days later she went to an ophthalmologist for presenting an increase in the size of the right eyelid, pain and whitish ocular discharge, changing the intramuscular antibiotic scheme, ceftriaxone plus oral clindamycin without improvement, she was sent to the emergency department to continue her treatment, upon admission she presented blepharoedema +++ in the right eye, painful on palpation, prevented eye opening, yellowish eye discharge +++, agglutination of eyelashes, forced eyelid opening of 2 mm painful Left eye: adequate lid closure, Bell's reflex present. No fever (Fig 1), physical examination found no lesions at any level, cardiopulmonary compromise, soft abdomen, no visceromegaly, normal extremities.
Figure 1: Blefaroedema +++ impide apertura ocular.
Tables: Laboratory report upon admission
| Blood Biometry | |
| Erythrocytes | 4.56 millones/UI |
| Hemoglobin | 11.70 g/dl |
| Hematocrit | 36.3 % |
| Vcm | 89.6 fl |
| Hcm | 25.7 pg |
| Platelets | 93 miles/UI |
| Leukocytes | 3.29 miles/UI |
| Neutrophils | 2.11 miles/UI |
| Lymphocytes | 0.95 miles/UI |
| Monocytes | 0.18 miles/UI |
| eosinophils | 0.00 thousand/UI |
| basophils | 0.03 thousand/UI |
| Serum Electrolytes | |
| Sodium (Na) | 136 mmol/l |
| Potassium (K) | 3.8 mml/l |
| Chlorine (Cl) | 101 mmol/l |
| General Urine Examination | |
| Density | 1.010 S/U |
| pH | 6 mmol |
| leukocytes | Negetive |
| nitrites | Negetive |
| proteins | Negetive |
| Glucose | Normal |
| Ketones | 15 |
| urobilinogen | Normal |
| Billirubin | Negetive |
| Hemoglobin | Negetive |
| Color | Yellow |
| Aspect | Clear |
| leukocytes | 0-1 × C |
| Epithelial cells | +++ |
| bacteria | ++ |
| Clinical Chemistry | |
| Glucose | 85 mg/DI |
| Urea | 22 mg/DI |
| Urea nitrogen | 10.09 mg/DI |
| C-reactive protein | 27.12 mg/L |
| Uric acid | 5.6 mg/DL |
| Total cholesterol | 125 mg/DI |
| Liver Function Tests | |
| Total bilirubin | 0.20 mg/DI |
| Indirect bilirubin | 0.10 mg/DI |
| Direct bilirubin | 0.10 mg/DI |
| Alanine amino transferase | 19 U/I |
| Aspartate aminotransferase | 25 U/I |
| lactic dehydrogenase | 269 U/I |
| Alkaline phosphatase | 105 U/I |
| Gamma giutamyltransferase | 38 U/I |
During her hospital stay, she presented feverish peaks of up to 39 degrees for 24 days. Complementary abdominal x-ray studies were requested where coprostasis was observed with colon dilation without visceromegaly (fig 2). chest x-ray no growth of cardiac cavities is observed, normal pulmonary flow (fig 3) multiple antibiotic treatments were prescribed. Ceftriaxone 32 mg/kg/day for 7 days, Vancomycin 16 mg/kg/day for 14 days, Meropenem 14 days, Ciprofloxacin Ophthalmic Sol 21 days Tobramycin /dexamethasone ophthalmic ointment 21 days, Paracetamol 15 mg/kg/dose, Ketorolac 0.5 mg/kg/dose, Prednisolone sol. Ophthalmic 10 days.
Figure 2: Abdominal X-ray shows coprostasis, colon dilation, no visceromegaly.
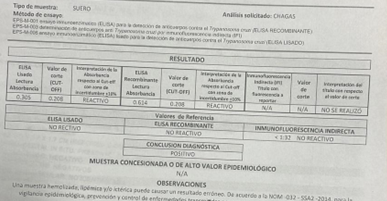
Figure 3: Chest X-ray without enlargement of heart chambers, normal pulmonary Flow with good evolution and clinical improvement in the right eye, a positive serological test was performed due to suspicion of Chagas disease, which was positive (fig 4).
Figure 4: Positive serological test for Chagas disease.
Treatment was started once the diagnosis was confirmed with nifurtimox at a dose of 12.5 mkg/day for 60 days with clinical improvement, being discharged home to continue with epidemiological and cardiology surveillance to avoid cardiac complications.
Discussion
In Chagas disease, the initial manifestations of the disease go unnoticed in most acute cases, 5% present apparent signs and symptoms and 30% of these, without visible symptoms or signs, will evolve to the asymptomatic chronic phase; Of these asymptomatic cases, 30% will develop a chronic clinical picture with cardiomyopathy or digestive problems.(6) The acute picture, which lasts from two to eight weeks, is characterized by parasitemia ; fever without special characteristics is also identified. Other common clinical signs and symptoms are lymphadenopathy , subcutaneous edema, hepatomegaly, splenomegaly, and heart rhythm disturbances. (7,8) In our case, the patient began with ocular symptoms without presenting initial fever, being among the 5% of patients who show signs that allow the identification of the inoculation site, the Romaña-Mazza sign presenting with a duration of more than one week. Among the mega digestive manifestations, the mega esophagus is more frequent, which can be diagnosed by radiological imaging; Not finding in this patient only growth of the colon due to constipation, multi-treated with antibiotics for presenting evidence of infection with paraclinical tests, as soon as Chagas disease is suspected, a serological study is requested confirming the disease, starting the appropriate treatment with good evolution and remission of symptoms , being discharged to her home for follow-up by epidemiology giving the necessary sanitary measures and surveillance of cardiac complications externally.
Conclusion
Chagas disease is very common in Mexico. Timely detection and early etiological treatment, along with expanded coverage, will enable successful medical care for patients with this disease.
Conflict of Interest
There are no conflicts of interest in this work.
References
- Organización Panamericana de la Salud. (2018).Guía para el diagnóstico y el tratamiento de la enfermedad de Chagas. Washington, D.C.: OPS.
Publisher | Google Scholor - González-Tomé MI, et al. (2013). Recomendaciones para el diagnóstico, seguimiento y tratamiento de la embarazada y del niño con enfermedad de Chagas. Enferm Infecc Microbiol Clin.
Publisher | Google Scholor - Martinez SJ, Romano PS and Engman DM. (2020). Precision Health for Chagas Disease: Integrating Parasite and Host Factors to Predict Outcome of Infection and Response to Therapy. Front. Cell. Infect. Microbiol. 10:210
Publisher | Google Scholor - Bravo-Gallego LY, Francisco-González L, Vázquez-Pérez Á, García-López Hortelano M, López Vélez R, González-Granado LI, et al. (2022) Pediatric Chagas disease in the non-endemic area of Madrid: A fifteen-year review. PLoS Negl Trop Dis 16(2).
Publisher | Google Scholor - Moscatelli G, Moroni S. (2022). Enfermedad de Chagas en Pediatría. Rev Hosp Niños (B Aires). 64(286):135–44.
Publisher | Google Scholor - Pino-Marín, A. Medina-Rincón, G.J. Gallo-Bernal, S. Duran-Crane, A. Duque, Á.I.A. Rodríguez, M.J. Medina-Mur, R. Manrique, F.T. Forero, J.F. Medina, H.M. (2021). Chagas Cardiomyopathy: From Romaña Sign to Heart Failure and Sudden Cardiac Death. Pathogens. 10:505
Publisher | Google Scholor - Edwards MS, Stimpert KK, Bialek SR, Montgomery SP. (2019). Evaluation and Management of Congenital Chagas Disease in the United States. Journal of the Pediatric Infectious Diseases Society. 8(5):461-469.
Publisher | Google Scholor - Wagner N, Jackson Y, Chappuis F, Posfay-Barbe KM. (2016). Screening and Management of Children at Risk for Chagas Disease in Nonendemic Areas. Pediatric Infectious Disease Journal. 35(3):335–337.
Publisher | Google Scholor - Carter YL, Juliano JJ, Montgomery SP, Qvarnstrom Y. (2012). Acute Chagas Disease in a Returning Traveler. The American Journal of Tropical Medicine and Hygiene [Internet].87(6):1038–40.
Publisher | Google Scholor - Rojo-Medina J, Ruiz-Matus C, Salazar-Schettino PM, González-Roldán JF. (2018). Enfermedad de Chagas en México. Gaceta de México [Internet]. 3:154(5).
Publisher | Google Scholor