Case Report
Case Report: Visual Field Loss Following Lateral Rectus Muscle Botulinum Toxin Injection
- Aaron Goldberg *
- Edward Botcherby
- Sarah Maling
Department of Ophthalmology, Stoke Mandeville Hospital, UK.
*Corresponding Author: Aaron Goldberg, Department of Ophthalmology, Stoke Mandeville Hospital, UK.
Citation: Goldberg A., Botcherby E., Maling S. (2024). Case Report: Visual Field Loss Following Lateral Rectus Muscle Botulinum Toxin Injection. Clinical Case Reports and Studies, BioRes Scientia Publishers. 5(1):1-4. DOI: 10.59657/2837-2565.brs.24.097
Copyright: © 2024 Aaron Goldberg, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 20, 2023 | Accepted: January 08, 2024 | Published: January 15, 2024
Abstract
Purpose: Raise awareness of a rare vision-threatening complication of botulinum toxin injections for strabismus.
Report: A 22-year-old woman underwent bilateral lateral rectus muscle botulinum toxin injections for exotropia. She then developed complete vision loss in the left eye over a few hours, which partially resolved by the following day, leaving a temporal field defect. Steroids were administered at day five, which precipitated further improvement. However, a temporal field defect still remains.
Conclusion: The underlying mechanism for this presentation is unclear, with trauma, compression, ischaemia or direct toxicity to the optic nerve and retina being possible. Ultimately, it is important to be aware of this complication so that patients can be consented adequately before receiving Botox treatment.
Keywords: strabismus; botulinum toxin; visual field loss
Introduction
Botulinum toxin A (Botox) has been used extensively in the treatment of strabismus both as a standalone treatment and as an adjunct to surgery since 1980 [1]. It is considered a low-risk intervention as complications such as overcorrection and ptosis are largely transient, with effects generally wearing off within six weeks [2]. A recent Cochrane review did not highlight any serious adverse events [3] and only a handful of case-reports have ever described severe ophthalmic complications [4-8]. In this case report we discuss an instance of Botox injection into the left lateral rectus (LR) muscle causing a permanent visual field deficit (VFD).
Case Report
A 22-year-old woman presented with residual alternating exotropia following four operations over a 15-year period, including maximal horizontal recti muscles surgery (8mm LR recessions and 6mm medial rectus (MR) resections bilaterally) and bilateral inferior oblique disinsertions. Visual acuity was 6/6 bilaterally. Her ocular deviations on alternating cover test were 20 and 30 prism dioptres at near and distance respectively. Half-dose Botox (2.5 units of DysportÒ) was injected into both LR muscles with electromyography (EMG) readings of 75% and 50% in the right and left eyes respectively. Two weeks later, there was significant improvement with minimal exophoria of two prism dioptres at near and three prism dioptres at distance. Over the next four months the effect of the Botox wore off and she reverted back to an alternating exotropia with the same measurements as before. A second pair of half-dose Botox injections were given into the LR muscles with respective right and left eye EMG readings of 100% and 75%. During the left eye injection, the patient experienced a lot of pain so was monitored for an hour for signs of retrobulbar haemorrhage then discharged with advice to take oral analgesia.
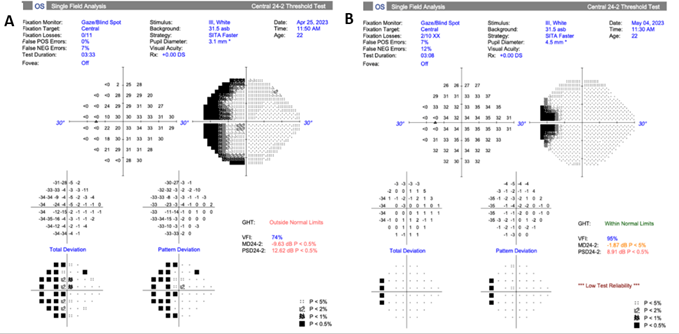
Figure 1: Humphrey visual field testing: A shows left eye temporal VFD on presentation post-Botox injection. B shows improving VFD after oral prednisolone.
Overnight she developed complete visual loss and complete ptosis in her left eye that came on progressively over a period of hours post-injection. She was reviewed in Eye Casualty the following morning. At this point she still had a mild ptosis that completely resolved when dilated with phenylephrine drops. Her vision had also improved (6/6 acuity) but she was noted to have a monocular temporal VFD on Humphrey visual field testing of the left eye (Figure .1A). There was neither relative afferent pupillary defect nor red desaturation, and colour vision testing was unremarkable. Eye examination was also unremarkable with no evidence of infection or globe perforation and the intraocular pressure was 17mmHg. After monitoring for five days and reviewing the limited literature on visual field loss [4,5], we made a speculative diagnosis of optic neuropathy and gave a course of oral prednisolone 40mg OD for two weeks with concomitant gastroprotection cover. The patient reported a significant recovery of visual field after starting the steroids, which was confirmed on visual field testing (Figure .1B). Electrodiagnostic tests performed at day 14 post-injection demonstrated symmetric Visual Evoked Potential responses consistent with normal optic nerve function, and there was no convincing evidence of ganglion cells dysfunction on Pattern Electroretinogram. Full field Electroretinogram recordings were similarly unremarkable. Optical Coherence Tomography (OCT) showed borderline retinal nerve fibre layer thinning temporally in the left eye compared to the right. The temporal VFD has stabilised and persists to date.
Discussion
Botox has a very good safety profile when used to treat strabismus, which is why there are so few reports highlighting complications. The transient complete monocular vision loss and ongoing temporal VFD is undoubtedly related to Botox administration in this case. As there were a few cases of presumed optic neuropathy post-Botox injection [4,5] that responded to steroids, we went ahead and gave this treatment once infection had been ruled out. In this case however, subsequent investigations, including electro diagnostics, seem to refute the diagnosis of optic neuropathy. Subjectively the patient felt that steroids accelerated improvement, but it is not clear if this was simply a placebo effect upon the natural course of the disease process. The underlying mechanism for her presentation still remains unclear. The Botox medication was unlikely to be contaminated because she received a dose from the same aliquot in the right eye without complication. Although retinal detachment following scleral perforation during a Botox injection has been reported [8], there was no evidence of this in our case. Equally the optic nerve or retina may have been damaged directly by the needle. However, her symptoms did not arise instantly and there was no evidence of trauma on fundal examination. She previously received a Botox injection into that same LR muscle without complication and the EMG recordings indicate the treatment was correctly delivered into the muscle.
The patient’s pain during injection suggests the needle may have taken an atypical trajectory, which could have been compounded by her altered orbital anatomy due to previous LR resection surgery. This could have led to Botox leakage within the orbit. In-vitro studies have illustrated neuronal degeneration and mitochondrial-mediated apoptosis induced by botulinum neurotoxin [9,10], thus such extravasation may have caused toxicity to retinal or optic nerve cells that would correlate with the timescale of her presenting symptoms post-injection. Additionally, there could have been leakage into a vascular structure such as the posterior ciliary artery. Local thrombotic effects, vascular wall injury or retinal hypoperfusion may have then been responsible as has been purported in other cases of post-Botox VFD [6,7]. Furthermore, vascular leakage of Botox may explain the ptosis in our case. It only lasted a few days, whereas direct Botox action on the levator neuromuscular junction would be expected to last much longer. The ptosis’ resolution with phenylephrine points more towards dysfunctional sympathetic drive of Muller’s muscle as in Horner’s syndrome. Systemic anticholinergic effects of Botox spread by blood vessels has been reported [11], and therefore the ptosis may have resulted from Botox reaching the preganglionic sympathetic nerve terminal in the superior cervical ganglion in this way.
The temporal VFD in this case corresponds to the nasal retina, which is on the opposite side of the globe to the LR Botox injection site. This discrepancy could be explained by compressive effects post-injection. In patients receiving Botox injections for thyroid-related orbitopathy, CT scans have shown hypertrophied injected recti muscles, suggesting they displace the optic nerve onto contralateral non-injected muscles at the orbital apex, causing optic neuropathy three weeks after injection [5]. Similarly, in our case the increased pressure from the volume of injected Botox may have compressed the left optic nerve fibres against the MR and given rise to her VFD. Compressive effects do not explain the VFDs reported in other cases, such as para-central scotomas and temporal VFD after MR injection [4].
Conclusion
Vision loss post-Botox injection is clearly a very rare complication of what is otherwise a safe intervention [2]. Further research is needed to delineate the underlying mechanism and possibly identify risk factors that may predispose patients to this side-effect. Overall, the variability of symptom onset time in the current case compared with other reports may signify a different aetiology. Ultimately, consideration needs to be given to this complication when consenting patients and we would also advocate for the early administration of steroids once infection has been ruled out.
Conflicts of Interest
Nil
References
- Dutton JJ, Fowler AM. (2007). Botulinum toxin in ophthalmology. Surv Ophthalmol., 52(1):13-31.
Publisher | Google Scholor - Rowe F, Noonan C. Complications of botulinum toxin a and their adverse effects. Strabismus. 2009 Oct-Dec;17(4):139-142.
Publisher | Google Scholor - Bort-Martí AR, Rowe FJ, Ruiz Sifre L, Ng SM, Bort-Martí S, Ruiz Garcia V. (2003). Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev., 3(3):CD006499.
Publisher | Google Scholor - Khalili MR, Hosseini S, Shirvani M, Sadati MS. (2022). Optic Neuropathy following Botulinum Toxin Injection into the Medial Rectus Muscle for Diplopia. J Ophthalmic Vis Res. 2022 Apr 29;17(2):296-302.
Publisher | Google Scholor - Korn BS, Seo SW, Levi L, Granet DB, Kikkawa DO. (2007). Optic neuropathy associated with botulinum A toxin in thyroid-related orbitopathy. Ophthalmic Plast Reconstr Surg., 23(2):109-114.
Publisher | Google Scholor - Chun BY, Kim SY. (2018). Acute visual loss after botulinum toxin A injection in the masseter muscle. Int Ophthalmol, 38:1339-1342.
Publisher | Google Scholor - Chen, Yi-Hsing M.D.; Tsai, Yueh-Ju M.D.; Chao, An-Ning M.D.; Huang, Yih-Shiou M.D.; Kao, Ling Yuh M.D. (2010). Visual Field Defect after Facial Rejuvenation with Botulinum Toxin Type A and Polyacrylamide Hydrogel Injection. Plastic and Reconstructive Surgery, 126(5):249e-250e.
Publisher | Google Scholor - Lee DH, Han J, Han SH, Lee SC, Kim M. Vitreous hemorrhage and Rhegmatogenous retinal detachment that developed after botulinum toxin injection to the extraocular muscle: case report. BMC Ophthalmol, 17(1):249.
Publisher | Google Scholor - Berliocchi L, Fava E, Leist M, Horvat V, Dinsdale D, Read D, Nicotera P. (2005). Botulinum neurotoxin C initiates two different programs for neurite degeneration and neuronal apoptosis. J Cell Biol., 168(4):607-618.
Publisher | Google Scholor - Akpınar O, Özşimşek A, Güzel M, Nazıroğlu M. Clostridium botulinum neurotoxin A induces apoptosis and mitochondrial oxidative stress via activation of TRPM2 channel signaling pathway in neuroblastoma and glioblastoma tumor cells. J Recept Signal Transduct Res., 40(6):620-632.
Publisher | Google Scholor - Witmanowski H, Błochowiak K. The whole truth about botulinum toxin - a review. Postepy Dermatol Alergol., 2020 Dec;37(6):853-861.
Publisher | Google Scholor