Case Report
Case Report: Painless Compartment Syndrome
- Arsen Shpigelman M.D
- David Maman M.D *
- Fadi Khalil Hanna M.D
- Jeries Hakim M.D
- Dimitri Vodovozov M.D
- Benjamin Bernfeld M.D
Carmel medical center, Haifa, Israel.
*Corresponding Author: David Maman, Carmel medical center, Haifa, Israel.
Citation: Arsen, S., David, M., Fadi, K. H., Jeries, H., Dimitri, V., Benjamin, B. (2023). Case Report: Painless Compartment Syndrome. Clinical Case Reports and Studies, BRS Publishers. 2(2); DOI: 10.59657/2837-2565.brs.23.018
Copyright: © 2023 David Maman, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 28, 2022 | Accepted: February 06, 2023 | Published: February 13, 2023
Abstract
Introduction: Acute compartment syndrome (ACS) is a surgical emergency that requires urgent intervention in order to prevent permanent structural damage and irreversible functional disability. The diagnosis of ACS depends on a high index of suspicion, relying on the following diagnostic criteria commonly known as the 5 Ps; Pain, Paresthesia, Paralysis, Pallor, and Pulse-lessness. When the diagnosis is uncertain, intracompartmental pressure greater than 30 mmHg is suggestive of ACS.
Case Presentation: We report a case of an underdiagnosed ACS, with a lack of classical presentation in a thirty-seven-years-old male patient with a history of myopathy. The patient was admitted to the emergency room due to direct trauma to his right hip, without a significant Visual Analogue Score. On his hip radiograph a subtrochanteric fracture of the right femur was demonstrated. An additional masked ipsilateral subcapital fracture was detected during the operation. The diagnosis of ACS was made during the operation while relying on the clinical appearance of the thigh and the clinical findings during surgery. Fasciotomies were performed, and open reduction with internal fixation via Proximal Femoral Nail was done. The diagnosis of ACS was confirmed later on, by the biopsy results.
Conclusion: This case suggests that myopathy can mask the classical presentation of ACS. Furthermore, the extent of pain complaints and accompanying paresthesia cannot be relied on in this regard and other clinical features should be considered in order to diagnose ACS.
Keywords: compartment syndrome, painless, myopathy, fasciotomy, subtrochanteric fracture
Introduction
Acute Compartment Syndrome is caused by increased pressure in a sealed myofascial compartment, resulting in muscular and neurovascular damage [1-3]. Increased pressure comprises perfusion, and necrosis occurs [1-3]. Early diagnosis and emergent fasciotomy are vital for the relief of intracompartmental pressure and to avoid irreversible damage. Delayed diagnosis can lead to complications ranging from residual disability to amputation [4].
All limb injuries, whether open or closed, can be complicated by compartment syndrome [1-4]. Compartment syndrome of the thigh is an uncommon condition, due to better dilative capacity of the thigh fascia, unlike the common ACS in the lower leg and forearm [5,6]. Diagnosis of ACS relies on proper assessment and evaluation of the patient in addition to a high index of suspicion relaying on the 5 Ps; Pain, Paresthesia, Paralysis, Pallor, and Pulse-lessness. Trauma with or without fracture has been well reported as a cause of ACS [1,2,4,6]. In addition, there are diverse alternative etiologies for ACS such as anticoagulation use, exercise, snake bites, and vascular injury [2-5].
Regardless of the etiology, the presentation may be similar; ACS usually presents with pain out of proportion to the injury, pain on a passive stretch of the muscle within the affected compartment, palpably tense compartment, paresthesia, and paralysis, and pulse-lessness which is typically a late sign of ACS [2]. The development of pain that is out of proportion to the injury and that is not relieved by analgesia is traditionally considered to be the earliest, most sensitive, and reliable indicator of the development of an underlying compartment syndrome [7].
In the literature, “silent” compartment syndrome has been reported in a few cases [5,7-10]. Silent compartment syndrome is compartment syndrome without significant pain or absence of marked pain on passive motion [7,8].
We report a unique case of ACS, in a thirty-seven-years-old male with a history of myopathy who presented with painless ACS. Myopathies are a heterogeneous collection of disorders characterized by the abnormal structure or functioning of skeletal muscle. These abnormalities of muscle cell structure and metabolism lead to various patterns of weakness and dysfunction. Myopathies are characterized by motor symptoms in the absence of any sensory involvement [11].
Case Presentation
A thirty-seven-year-old male patient presented at the Accident and Emergency Department of our institution after direct trauma to his right hip due to a fall in the bathroom. His past medical history included myopathy and hypothyroidism, functional history included mobility to close destinations using a walker and wheelchair for far destinations.
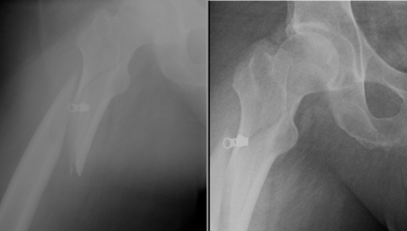
The patient presented in a good condition, and hemodynamically stable. The initial emergency room assessment revealed a slight tenderness over the proximal thigh, mild shortening, and externally rotated right lower extremity. Neurovascular examination revealed bilateral muscle weakness 3/5 in the lower extremities without vascular deficit. No additional injuries were noted. Plain X-ray images of anterior-posterior (AP) and Axial radiographs of the pelvis and right hip demonstrated displaced subtrochanteric femoral fracture (Fig. 1).
Figure 1: Right Hip radiograph demonstrating subtrochanteric fracture of the right femur.
Follow-up prior to operation included vital signs reported to be within normal limits, Visual Analogue Score assessment was not significant despite limited analgesia (VAS of 3-4/10), laboratory tests were normal, and close neurovascular examination did not change prior to the surgery.
Physical assessment shortly before surgery was notable for severely and diffusely distended and swollen thigh, hard to palpation, and bluish discoloration under toenails of the involved extremity.
Under general anesthesia, the patient was transferred to the operation table and mild traction was applied. After sterilization and draping of the involved extremity, a longitudinal surgical skin incision was made on the lateral aspect on the proximal to middle third of the thigh, separation of the subcutaneous tissue, exposure and incision of the fascia lata. Surprisingly, incision borders of the fascia were spontaneously retracted, and huge bulge of the vastus lateralis part of quadriceps muscle protruded out of the skin incision. The muscle appeared whitish, with only mild muscular bleeding noticed. A muscle biopsy was performed, and the specimen was sent to the pathology laboratory. The combination of the bulging of the vastus lateralis and his whitish color raised a high suspicion of masked compartment syndrome, hence a fasciectomy was performed. After muscle retraction, and exposure of the fracture ends, open reduction of the subtrochanteric femur fracture was done under fluoroscopic guidance. During this action, an ipsilateral subtle sub capital fracture was discovered.
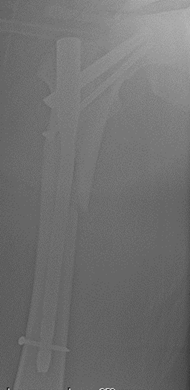
Internal fixation using Proximal Femoral Nail (PFN) and an additional anti-rotational hip screw were inserted as shown in Fig. 2. As part of the gold standard care of ACS at the end of the surgery, the fascia and skin were not sutured, and the surgical wound was draped with sterile gauzes.
Figure 2: Radiograph of the right hip after reduction and internal fixation.
After the surgery, the patient was admitted to the Orthopedic Department in order to monitor his vital signs, for laboratory tests (blood electrolytes, kidney function test, and hemoglobin levels), and in order to assess his clinical condition. He received extensive hydration with 0.9% normal saline and antibiotics. A notable significant clinical improvement of the thigh and the right lower limb were recorded.
One week later, he was scheduled for secondary wound closure. Then he was finally discharged to a rehabilitation institution. After 6 weeks the biopsy results were obtained and confirmed our diagnosis of ACS. About 6 months later, the patient was examined at our clinic, and he demonstrated a full recovery to his baseline status.
Discussion
Acute compartment syndrome (ACS) is a surgical emergency that requires urgent intervention to prevent permanent and irreversible functional and structural damages. The diagnosis of ACS depends on a high index of suspicion, relying on clinical features (Pain, Paresthesia, Paralysis, Pallor, and Pulseless-ness) [1-3]. The development of pain that is out of proportion to the injury and that is not relieved by analgesia is traditionally considered to be the earliest, most sensitive, and reliable indicator [2,3,4-6].
Our patient presented with mild pain in relation to the injury he suffered, which reduced the initial suspicion of compartment syndrome. Moreover, the patient was injured in a location that is less typical of ACS and with an injury mechanism that is less suitable for ACS [8]. Although pain is commonly the leading symptom in ACS, the absence of severe pain does not necessarily exclude ACS as shown in our case and in previous studies [4,5,7,8].
Previous literature reported cases of ACS with missed or delayed diagnosis due to atypical presentation or atypical etiology. There are 12 cases of silent compartment syndrome reported in the literature, including the present cases, with the majority occurring secondary to traumatic tibial fracture [9,10]. Review of the literature concerning silent compartment syndrome case reports showed that most patients had minimal to mild pain, and tense swollen limb [10]. In our case, the presence of myopathy masked a compartment syndrome with an atypical presentation in a patient who had a subtrochanteric and sub capital femur fracture. The main presenting symptom in our patient was noticeably swollen limb. Our case demonstrates that even in an Acute setting, when a patient is admitted with a fracture that needs emergent surgical reconstruction, obtaining a proper history from the patient and evaluating his functional history before the injury is necessary in order to perform better medical decisions. Furthermore, even when the clinical presentation is not typical for ACS, this condition should always be considered in the differential diagnosis of an Orthopedic Surgent especially in a patient with a swollen limb.
Conclusion
We must always maintain a high index of suspicion for Acute Compartment Syndrome even if the documented criteria on which diagnosis is made, are not fully met, thus preventing long-term disability. Although ACS is considered a clinical diagnosis, the absence of pain does not exclude the diagnosis of ACS. Moreover, we must always bear in mind that myopathies and neuropathies might mask the typical diagnostic criteria of ACS.
Clinical Message
Diagnosing painless compartment syndrome can be challenging. Although ACS is considered a clinical diagnosis, the absence of pain does not exclude the diagnosis of ACS. Our case demonstrates that even in an Acute setting, when a patient is admitted with a fracture that needs emergent surgical reconstruction, obtaining a proper history from the patient and evaluating his functional history before the injury is necessary in order to perform better medical decisions.
Learning Point of the Article: In rare cases Acute compartment syndrome can present without acute severe pain.
Funding: This research received no external funding.
Informed Consent Statement: Informed consent was obtained from the patient.
Conflicts of Interest: The authors declare no conflict of interest.
References
- Lemberg, R. M., Dougherty, C., & Mallon, W. K. (2011). Enoxaparin-induced bleeding resulting in compartment syndrome of the thigh: A case report. Journal of Emergency Medicine, 41(1):1-4
Publisher | Google Scholor - Glutens, G. (1994). Spontaneous compartment syndrome in a patient with diabetes insipidus. International Orthopedics, 18(1):53–54.
Publisher | Google Scholor - Hope, M. J., & McQueen, M. M. (2004). Acute compartment syndrome in the absence of fracture. Journal of Orthopedic Trauma, 18(4):220-224.
Publisher | Google Scholor - Frei, Benjamin; Sommer-Joergensen, Vivienne; Holland-Cunz, Stefan; Mayr, Johannes. (2020). Acute compartment syndrome in children; beware of “silent” compartment syndrome. Medicine: Volume 99 - Issue 23 – p e20504.
Publisher | Google Scholor - Smith, R. D. J., Rust-March, H., & Kluske, S. (2015). Acute compartment syndrome of the thigh in a rugby player. BMJ Case Reports, 1-4.
Publisher | Google Scholor - Foster, R. D., & Albright, J. A. (1990). Acute compartment syndrome of the thigh: Case report. Journal of Trauma - Injury, Infection and Critical Care, 30(1):108-110.
Publisher | Google Scholor - S. Badhe, D. Baijiu, R. Elliot, J. Rowles, D. Calthorpe. (2008). The ‘silent’ compartment syndrome. Injury, Int. J. Care Injured 40 220-222.
Publisher | Google Scholor - Eyre's, K. S., Hill, G., & Maids, A. (1996). Compartment syndrome in tibial shaft fracture missed because of a local nerve block. The Journal of Bone and Joint Surgery. British Volume, 78(6):996-997.
Publisher | Google Scholor - Wright, J., Griffiths, D. E., & Nwaboku, H. C. (2011). Acute compartment syndrome with an atypical presentation: a useful clinical lesson. JRSM Short Reports, 2(4):1-3.
Publisher | Google Scholor - Hasan Alesia, Ghadeer Alsager, Abdulrahman Pasha, Hussain AL Yousif, Hani Valsartan & Saad Surer. (2021). Is It Compartment Syndrome? Two Case Reports and Literature Review. Cures, 13(10):e19083.
Publisher | Google Scholor - Rose M. Domingo-Horne, Mohammad Kian Sleighed. (2017). An Approach to Myopathy for the Primary Care Clinician. The American journal of medicine, 131(3):237-243.
Publisher | Google Scholor