Research Article
Cardiovascular Risk Factors
1Riggs Pharmaceuticals Karachi Department of Pharmacy, University of Karachi-Pakistan.
2Head of the Department of Pharmacology, Fazaia Ruth Pfau Medical College, Shahrahe Faisal Karachi.
3Assistant Professor, Department of Microbiology, University of Karachi, Pakistan.
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals Karachi Department of Pharmacy, University of Karachi-Pakistan.
Citation: R. Haider, A.Mehdi, A.Zehra. (2024). Cardiovascular Risk factors, Journal of BioMed Research and Reports, Biores Scientia Publishers. 4(3):1-16. DOI: 10.59657/2837-4681.brs.24.060
Copyright: © 2024 Rehan Haider, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 12, 2023 | Accepted: January 23, 2024 | Published: January 26, 2024
Abstract
Cardiovascular disease (CVD) is the main cause of morbidity and mortality worldwide. Various risk factors contribute to the improvement and development of CVDs, encompassing both modifiable and non-modifiable elements. This abstract highlight the important cardiovascular risk factors and their impact on coronary heart fitness. Age and sex: Advancing age and being male are non-modifiable risk factors associated with increased CVD risk. Guy women are usually at a better chance than premenopausal women; however, this difference decreases menopause. High blood pressure: Extended blood strain is a sizable, modifiable risk factor for CVDs. Controlling hypertension damages blood vessels, causes atherosclerosis, and increases the risk of heart attack, stroke, and coronary heart failure.
Dyslipidemia: High levels of LDL cholesterol and triglycerides, coupled with low levels of HDL cholesterol, contribute to atherosclerosis and plaque formation, leading to coronary artery disease and other cardiovascular complications.
Smoking: Cigarette smoking is the main modifiable risk factor for CVDs. It damages blood vessels, accelerates atherosclerosis, and decreases oxygen delivery to tissues, thereby increasing the risk of heart disease and stroke.
Diabetes Mellitus: Type 1 and type 2 diabetes drastically increase the risk of CVDs because of insulin resistance, inflammation, and metabolic abnormalities that adversely affect blood vessels and the heart.
Obesity: Extra body weight, specifically abdominal adiposity, increases the likelihood of CVDs by contributing to insulin resistance, hypertension, dyslipidemia, and inflammation.
Body state of being inactive: A sedentary lifestyle and a shortage of regular bodily pastimes are connected to weight problems and numerous metabolic disturbances that lead to CVD improvement.
Circle of relative’s records: A high-quality family record of premature CVD increases an individual's chance, suggesting a genetic predisposition to heart disease.
Weight reduction plan: consuming an excessive diet of saturated and trans-fat, salt, and introduced sugars, even as missing fruits, vegetables, and whole grains, can contribute to the CVD threat. Strain and intellectual health: Chronic pressure, depression, and anxiety can affect CVD risk via numerous mechanisms, including unhealthy coping behaviors and hormonal imbalances.
Alcohol consumption: While mild alcohol consumption may also have some cardiovascular blessings, immoderate ingestion can boost blood strain and contribute to coronary heart muscle damage. Efforts to mitigate cardiovascular hazard factors should include recognition of lifestyle adjustments, including ordinary workouts, a heart-wholesome diet, smoking cessation, stress management, and blood pressure and cholesterol control. The early identification of chance factors and their effective control can play an important role in decreasing the burden of cardiovascular illnesses and improving typical coronary heart health.
Keywords: cardiovascular health; risk factors for heart disease; identifying cardiovascular risks heart disease risk factors; modifiable cardiovascular risk factors; non-modifiable cardiovascular risk factors and managing cardiovascular risk
Introduction
Hypertension is often accompanied by both type 1 (T1DM) and type 2 (T2DM) diabetes mellitus. The association between these two conditions has been recognized for a long time. In 1923, the Swedish physician Eskil Kylin described a syndrome of diabetes, hypertension, and hyperuricemia [1], which are now regarded as aspects of the broader “metabolic syndrome” linked to insulin resistance (IR) [2, 3]. The association between diabetes and hypertension is complex. Both are standard and likely to be associated by chance, but in some instances, they may have a common cause. Moreover, hypertension can develop as a consequence of diabetic nephropathy, whereas some drugs used to treat hypertension can induce diabetes in susceptible subjects. Hypertension is important because, like diabetes, it is a major cardiovascular risk factor that synergizes with the deleterious effects of diabetes. It is also a risk factor for microvascular complications such as nephropathy and retinopathy. The management of hypertension in diabetes has been widely debated, and there is still a need for consensus on treatment targets and strategies. During the last decade, several well-constructed trials have added considerably to the evidence base [4 – 8], demonstrating the benefits of lowering blood pressure (BP) but also highlighting the difficulty of achieving this in practice.
Size of the problem
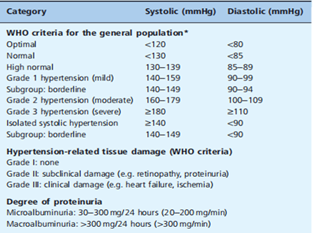
Hypertension was widely defined according to the World Health Organization/International Society of Hypertension (WHO/ISH) criteria (Table 40.1). People with diabetes are still at risk for macro vascular and microvascular complications at BP levels below these thresholds, and the treatment target range is, therefore, lower (130 – 140/80 – 85 mmHg). Overall, hypertension (according to the WHO criteria) is up to twice as common in people with diabetes as in the general population [9]. In white Europeans, 10 – 30% of subjects with T1DM and 60 – 80% of those with newly diagnosed T2DM have hypertension [10]. There are racial and ethnic differences in the prevalence of hypertension, which presumably are at least partly genetically determined: for example, hypertension (and macro vascular disease) is less frequent among the Pima Indians and Mexican Americans [11]. Impaired glucose tolerance (IGT) is also associated with hypertension (20 – 40% of cases), perhaps reflecting the common origins of these aspects of the metabolic syndromes [12]. There is evidence that the true prevalence of hypertension is increasing in the diabetic population (especially T2DM) after allowing for a greater number of cases identified through improved screening and lowering of thresholds for BP [13]. The causes probably include the rising prevalence of obesity and the longer survival of older people with diabetes.
Causes Of Hypertension in Diabetes
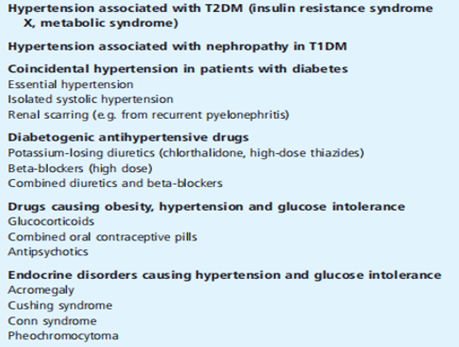
The association between high blood pressure and diabetes is shown in Table 40.2. Vital and remote systolic hypertension is common in the non-diabetic population (particularly in the elderly). It is anticipated that important high blood pressure is due to approximately 10% of cases in people with diabetes. Other crucial reasons are hypertension that coexists with IR, obesity, and IGT in metabolic syndrome, and high blood pressure secondary to diabetic nephropathy, as discussed in detail below.
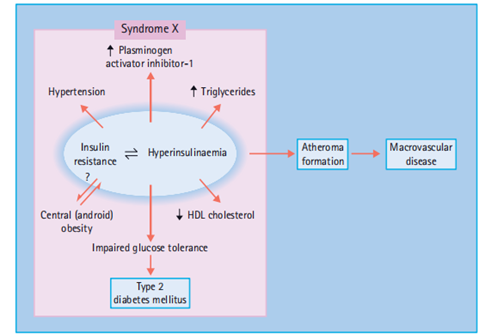
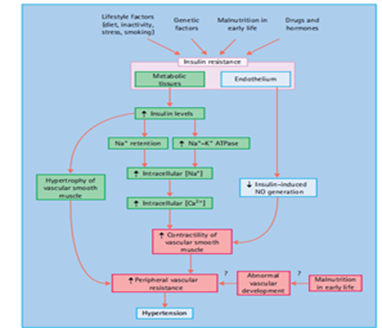
Hypertension in the metabolic syndrome. This syndrome includes IR, IGT (which includes T2DM), characteristic dyslipidemia. hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, and raised low-density. lipoprotein (LDL), with an extra of small dense LDL debris – truncal obesity, pro coagulant. modifications (raised plasminogen activator inhibitor 1 and fi fibrinogen stages) and Hyperuricemia [2,14,15]. As those abnormalities are all chance factors for atherogenesis, the syndrome is characterized by a marked tendency toward vascular aging mainly due to macro vascular ailments, particularly coronary heart disorder (CHD) and stroke (Figure1).
Table 1: criteria for hypertension and related tissue damage, defined by the world Health Organization (WHO) and the international Society for Hypertension. 1999 (33).
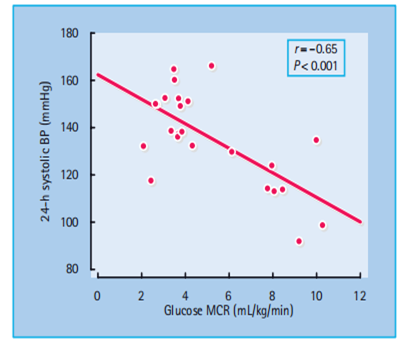
IR has been proposed via Reaven [2], DeFronzo and Ferrannini [14] and others [15] to be an essential reason for high blood pressure and cardiovascular sickness (CVD) as well as T2DM. IR is partially Genetically determined factors, including obesity, physical inactivity, and perhaps malnutrition in utero and during early infancy, may also contribute [16]. In support of the latter, family studies have revealed a correlation between the BP of the mother and her offspring that appears to be non - hereditary in origin; early growth retardation is suggested to program abnormal development of the vasculature as well as the tissues that regulate glucose homeostasis IR is closely associated with a high BP in both humans and animals. Experimental induction of IR (e.g., feeding rats fructose) is accompanied by an increase in BP. An inverse relationship has been demonstrated in humans between BP and insulin sensitivity [17] (Figure 40.2).
Figure 1: The metabolic syndrome. HDL, high density lipoprotein.
Table 2: Associations between hypertension and diabetes
Figure 2: Hypertension is associated with insulin resistance.
Insulin sensitivity, measured as the metabolic clearance rate (MCR) of glucose during an insulin clamp study, is inversely related to the mean 24 - hour systolic and ambulatory blood pressure. Reproduced from Pinkney et al. [17], with permission from the Editor. Various mechanisms have been proposed to explain how IR and/or hyperinsulinemia could increase BP (Figure 40.3). First, there is some evidence that insulin is an endothelium-dependent vasodilator, releasing nitric oxide (NO) from the endothelium, which relaxes vascular smooth muscle [18,19]; blunting of this aftereffect, caused by insensitivity to the action of insulin on the endothelium as well as on metabolically important tissues, could contribute to increased peripheral resistance, which is a hallmark of hypertension in obesity and T2DM. Impaired endothelium-mediated vasodilation is associated with IR states and may plays a key role in the initiation and progression of atherosclerosis [20]. In contrast, insulin also has several actions that tend to raise BP, and there is some evidence that these are accentuated in IR states, presumably because sensitivity is preserved to the effects of raised insulin levels. Insulin acts on the distal renal tubule to retain Na + ions and water [20,21], an effect that still operates in IR subjects [22], and thus could contribute to the increase in total body Na + content that occurs in obesity and T2DM [23]. Insulin also stimulates the cell membrane Na + – K + ATPase, which raises intracellular Na + concentrations in vascular smooth muscle, and increasing systolic Ca 2+ levels enhance contractility and increases peripheral resistance [22,23]. Insulin may stimulate sympathetic outflow through its effects on the CNS. Theoretically, this could also increase BP, although direct evidence in humans is lacking [22,24]. Finally, insulin may stimulate the proliferation of muscle cells, which can lead to medial hypertrophy and increased peripheral resistance [22,25].
Hypertension and diabetic nephropathy
This association is most obvious in young patients with T1DM, in whom the presence of hypertension is strikingly related to renal damage and even to minor degrees of proteinuria. BP begins to rise when the urinary albumin excretion (UAE) enters the Microalbuminuria range (> 30 mg/24 hours) and is usually over the WHO threshold when UAE reaches the Microalbuminuria (> 300 mg/24 hours) [26]. The association may be partly genetically determined: subjects with diabetes and Microalbuminuria commonly have parents with hypertension and may also inherit over activity of the cell - membrane Na + – H + pump (indicated by increased Na + – Li + counter-transport in red blood cells), which would tend to raise intracellular Na + concentrations, thus increasing vascular smooth muscle tone [27].
The basic mechanisms of hypertension include decreased Na +excretion with Na + and water retention. Peripheral resistance is increased, which raised intracellular Na + will contribute. The role of the renin-angiotensin-aldosterone system (RAS) is uncertain, as both increased and decreased activity have been reported [28,29]. These discrepancies may be explained by differences in diet, treatment, metabolic control, and the type and duration of diabetes. Na + retention and hypertension would be predicted to suppress the RAS, while renin levels may be influenced by other complications of diabetes: renal tubular acidosis type 4 causes Hyporeninemic hypo aldosteronism and neuropathy can also lower plasma renin levels, while renin may be elevated in retinopathy and advanced nephropathy. Patients with Microalbuminuria who are insulin-resistant appear to be particularly susceptible to hypertension [30].
Figure 3: Possible mechanisms of hypertension in conditions of insulin resistance. NO, nitric oxide.
Impact of hypertension on diabetes
A large proportion of hypertensive people with diabetes show signs of cardiovascular aging and target-organ damage [10]. Hypertension, as an independent risk factor for atherogenesis, synergizes with the effects of diabetes and significantly increases the development and progression of CHD, and cerebrovascular and peripheral vascular diseases. Overall, the effects of hypertension on deaths from CHD increased by 2 – 5 times in people with diabetes, with the greatest increase occurring at the lowest BP levels. The deleterious effects of hypertension on left ventricular function have also been attributed to the presence of diabetes. These include impaired left ventricular relaxation [31] and increased. left ventricular mass [32], with the latter being an independent predictor of premature death from CHD. Hypertension also predisposes to the development of certain microvascular complications, particularly nephropathy and end-stage renal failure (ESRF), for which the risk is increased by 2 – 3 times Hypertension is also a risk factor for retinopathy, as has been confirmed by the beneficial effects of improved BP control in patients with T2DM, reported by the UK Prospective Diabetes Study (UKPDS) [4].
Screening for hypertension in diabetes
If the two conditions are commonly associated, people with diabetes must be regularly screened for hypertension and vice versa. Hypertensive patients, especially those who are obese or are receiving treatment with potentially diabetogenic drugs, should be screened for diabetes at diagnosis and during follow-up. a hyperglycemic camera is detected, diabetogenic antihypertensive drugs should be reduced or changed to others or used in combinations that do not impair glucose tolerance, and normoglycemia can often be restored. All individuals with diabetes should have their BP checked at diagnosis and at least annually thereafter. This is especially important in patients with other cardiovascular risk factors such as nephropathy (which is associated with a substantial increase in the cardiovascular mortality rate), obesity, dyslipidemia, smoking, or poor glycemic control.
Measurement of blood pressure BP should be measured with the patient in the supine or sitting position with an accurate sphygmomanometer and a cuff of appropriate size (i.e., wider for obese subjects with an arm circumference of > 32 cm). Systolic and diastolic BP should be recorded to the nearest 2 mmHg if using a manual sphygmomanometer from phases I and V (i.e., appearance and final disappearance of the sounds of Korotkoff). Precautions should be taken to ensure reliability and avoid “white coat” stress effects that can acutely raise BP. Conditions should be quiet and relaxed, and at least two readings should be taken initially and then repeated at intervals of weeks or months to determine the subject’s typical values and any trend to change. Office BP measurements can be complemented by repeated home BP recordings. BP should also be checked with the patient in the upright position (1 min after standing) because there may be a significant postural fall (> 20 mmHg systolic) in patients with diabetic autonomic neuropathy, the elderly, or those treated with vasodilators or diuretics. Marked postural hypotension, which can coexist with supine hypertension, may indicate the need to change or reduce antihypertensive medications, especially if symptoms are provoked. Ambulatory BP monitoring over 24 hours may be useful in some cases to exclude “white coat” effects, and in patients with early nephropathy who have nearly normal BP during the day, but who may be at risk of hypertensive tissue damage because they fail to show the physiologic BP dip during sleep [33].
Diagnosis of hypertension in diabetes
The criteria issued in 1999 by WHO and ISH [34] define hypertension as an office BP exceeding 140/90 mmHg (Korotkoff I – V), and borderline hypertension as being below these limits but > 130 mmHg systolic and/or 85 mmHg diastolic [34]. Established hypertension is diagnosed when readings consistently exceed 140/90 mmHg over several weeks, when the BP is very high (diastolic BP > 110 mmHg), or when there are clinical signs of tissue organ damage from long-standing hypertension. It is clear from numerous epidemiologic studies that the WHO/ISH threshold is too high in people with diabetes because of the additional risk of both macro vascular and microvascular diseases and that there are definite benefits to treating Microalbuminuria subjects whose diastolic BP is < 90>
Management of hypertension in diabetes
Strict BP control is the primary treatment goal. In recent years, target treatment levels have declined progressively to the current recommendation of a mean office BP lesousedf than 130 – 140/80 – 85 mmHg for all patients who can tolerate this condition without side effects, such as orthostatic reactions or compromising arterial circulation in critical vascular beds. Recent observations indicate that subgroups of susceptible patients who will not tolerate a dramatic BP reduction below 130 mmHg systolic BP might exist; therefore, caution should be exercised. Management begins with lifestyle modification, but few patients respond to this alone, and most will require more than one antihypertensive drug to control BP adequately [4,5].
Non - pharmacologic Treatment
The treatment of high blood pressure in patients with diabetes needs to be primarily based on dependent lifestyle interventions. This includes weight discount or weight stabilization inside the overweight, sodium limit, weight-reduction plan modification, and ordinary bodily exercise (moderate intensity, 40 – 60 min, 2 – three times weekly). Nutritional consumption of saturated fats has been related to impaired insulin sensitivity, and must therefore be reduced [37]. Alcohol needs to be constrained to 2–3 units/day in guys and 2 units/day in girls but left out Altogether, high blood pressure is difficult to manipulate. Smoking causes an acute boom in blood pressure and greater average variability [38]. Smoking cessation is especially critical, as smoking now not simplest speeds up the development of atherosclerosis and vascular growing old, but also impairs insulin sensitivity [39] and worsens albuminuria [40]. treatment with nicotine supplementation for 4 – 6 weeks (chewing gum or patches), bupropion, or Varenicline may be useful. When followed completely by using the patient, the way of life modification can be extraordinarily powerful. The above measures can decrease systolic and diastolic BP by using 11 and 8 mmHg, respectively [41] – as much as many antihypertensive drugs – and often enough to obviate the need for drug therapy. Weight reduction in overweight patients can similarly reduce BP.
Antihypertensive drug therapy
Numerous drugs are available to lower BP, but some are better suited to the particular needs of patients with diabetes because of their favorable or neutral effects on glucose metabolism and other factors. Most patients (at least two-thirds) will require combinations of antihypertensive drugs to control BP, with an average of approximately three different drugs in two large studies [4,5]. Accordingly, the clinician must be able to use a wide variety of antihypertensive pills and choose combinations that achieve maximum pharmacological synergy. usually aggregate therapy the way lower doses of character pills can often be used, Accordingly, the risk of harmful effects is reduced.
Diuretics
Diuretics are often powerful antihypertensives for human beings with diabetes, in which the total body sodium burden is increased and increased extracellular fluid volume [42]; but diuretics that increase urinary losses of potassium and magnesium can worsen hyperglycemia because insulin secretion is impaired by potassium depletion and insulin sensitivity in peripheral tissues may additionally also, reduce [43]. taking excessive doses of thiazide diuretics -equivalent to ≥ 5 mg/day bedroll Ume thiazide (bendrofluazide) It is said to increase the likelihood of developing diabetes in hypertensive patients up to threefold; this does not happen at low doses (up to 2.5 mg/day of Bendroflumethiazide) [44].Potassium depletion is particularly excessive with an overdose of chlorthalidone (chlorthalidone), less so with furosemide (Frusemide) and bedroll Ume-thiazide, and reportedly negligible with indapamide. This mechanism is irrelevant for C - peptide-negative subjects with T1DM who are dependent on exogenous insulin. In addition, thiazides may worsen dyslipidemia [45], even when it is low doses may pose little risk. Thiazides were extra associated with gout and impotence and usually avoided middle-aged men with diabetes and hyperuricemia or erectile disorder However, some evidence suggests that the risk of erectile dysfunction may have been overestimated. Diuretics can induce hyperosmolar hyperglycemia syndrome and must be prevented by being used at the lowest effective dose in patients with a record of this type of hardship. Diuretics are effective in preventing CVD in elderly subjects with T2DM and systolic high blood pressure [46 and the butane observational view suggested that the use of diuretics increased cardiovascular mortality in hypertensive patients with T2DM who were still hyperglycemic, regardless of treatment [47]. By default, these pills are strong and safe for use in patients with diabetes. Diuretics suitable for use in diabetic high blood pressure include furosemide, Bendroflumethiazide (≤ 2.5 mg/day), hydrochlorothiazide, spironolactone, and indapamide. Low doses must be used, sometimes mixed with potassium supplements or potassium-sparing tablets including amiloride. If diuretics are ineffective, they should be mixed with other first-line drugs (e.g., angiotensin II receptor inhibitors or antagonists [ARB]). and then administered an extended dose. Spironolactone is exceptional when not combined with an ACE inhibitor, as it increases the risk of hyperkalemia. Furosemide is useful in patients with impaired renal function (serum creatinine level > 150 μmol/L) or edema. During this period, serum urea, creatinine, and potassium levels should be checked for initiation of diuretic therapy and every 6 – one year thereafter, as risk disorders of plasma potassium levels may develop, specifically in patients with diabetes and impaired renal function.
β - Adrenergic blocking agents
Beta-blockers may significantly lower BP levels in patients with diabetes and hypertension, even though renin release (a major target of these drugs) is commonly reduced in diabetes because of Na + and fluid retention. These drugs are often ineffective in Afro-Caribbean patients commonly have low renin levels. Other mechanisms of action that reduce BP include reductions in heart rate and cardiac output via interaction with β1 - and β2 - receptors in the myocardium and the vessel wall. Similar to diuretics, beta-receptor blockers may aggravate both hyperglycemia and dyslipidemia [48]. These effects depend on both the dosage and the degree of selectivity of the individual drug. The hyperglycemic effect is attributed to the inhibition of β2 - adrenergic-mediated insulin release and decreased insulin action in peripheral tissues; the long-term risks of a person without Diabetes developing disease may be increased by six-fold [49] and even more, if given together with thiazides. Some studies have suggested that the hazards of both hyperglycemia and hyperlipidemia have been exaggerated and maybe both dose-dependent and secondary to weight gain [50]. The metabolic side effects of beta-blockers can be reduced by using low dosages combined with other agents, particularly dihydropyridine calcium channel antagonists (CCAs), or by intensifying non-pharmacological efforts to decrease weight and improve physical activity. Beta-blockers have other side effects relevant to diabetes. They may interfere with the counter-regulatory effects of catecholamines released during hypoglycemia, thereby blunting manifestations such as tachycardia, tremors, and delayed recovery from hypoglycemia [51]. However, in clinical practice, this rarely presents a serious problem, especially when cardio-selective β1 - blockers are used. Beta-blockers may also aggravate impotence and are generally contraindicated for second or third-degree atrioventricular (AV) heart block, severe peripheral vascular disease, asthma, and chronic airway obstruction. Recent studies have shown that certain beta-blockers such as metoprolol and carvedilol [52,53] can be used favorably in cardiac failure in patients with diabetes, as shown in the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT - H F) study, in which 25% of the patients had diabetes [52]. Atenolol is a commonly used drug because it is cardio-selective and water-soluble, which reduces CNS side effects and renders its metabolism and dosage more predictable. It is most effective as a single daily dose, which probably encourages compliance. In the UKPDS, its effect was comparable to that of the ACE inhibitor captopril [54]; however, it should be kept in mind that the stroke preventive effect of atenolol is 16% less than that of other antihypertensive drugs, based on data from meta-analyses. Metoprolol is an alternative treatment at moderate doses. Both non-selective and selective beta-blockers are effective in the secondary prevention of myocardial infarction (MI) after an initial event in patients with diabetes [55]. Metoprolol or carvedilol may be indicated in patients who also have heart failure [52,53], and beta-blockers in general, are useful for patients with angina or tachyarrhythmia.
Calcium-channel antagonists
These vasodilator agents do not generally worsen metabolic control when used at conventional dosages, although sporadic cases of hyperglycemia have been reported after starting a calcium channel antagonist (CCA) of the dihydropyridine class [56]. This may be caused by the inhibition of insulin secretion (a calcium-dependent process) in susceptible patients or a compensatory sympathetic nervous activation, which antagonizes both Insulin secretion and action following vasodilation. CCAs have a slight negative inotropic effect and are contraindicated in significant cardiac failure; they often cause mild ankle However; this is caused by the relaxation of the peripheral pre capillary sphincters and increased capillary pressure rather than right ventricular failure. Owing to their potent vasodilator properties, these drugs can cause postural hypotension and can be aggravated by autonomic neuropathy. Non-dihydropyridine CCAs (e.g., verapamil) reduce proteinuria in diabetic nephropathy, but this effect is not observed with dihydroxy-riding derivatives such as nifedipine, amlodipine, felodipine, and isradipine [57]. Because of their other cardiac actions, these drugs are particularly indicated in hypertensive patients who also have angina (e.g., sustained-release nifedipine and diltiazem) or supra ventricular tachycardia (e.g., verapamil). Their vasodilator properties may also be beneficial in peripheral vascular diseases. CCAs are ideally combined with selective β1 - blockers, but the specific combination of verapamil and beta-blockers (especially together with digoxin) must be avoided because of the risk of conduction blocks and asystole’s. Overall, CCAs appear less or similarly cardioprotective but better at preventing stroke than either beta-blockers or Thiazide diuretics [58,59]. Amlodipine administered once daily is an evidence-based and convenient preparation for general use, and felodipine, nicardipine, and sustained-release nifedipine are suitable alternatives.
Angiotensin-converting enzyme inhibitors
ACE inhibitors may be used in diabetic hypertension, even in cases where the general RAS is not activated, and as the drug interferes with the local angiotensin action in specific target tissues. However, when used alone, these agents have limited hypotensive action in many black patients who tend to have suppressed RAS activity. ACE inhibitors have no adverse metabolic effects and may even improve insulin sensitivity [60]; hypoglycemia has rarely been reported [61]. These drugs are particularly beneficial in diabetic nephropathy by reducing albuminuria and possibly delaying the progression of renal damage [62]. Their antiproteinuric effect may be caused specifically by the relaxation of the efferent arterioles in the glomeruli, which are highly sensitive to vasoconstriction by angiotensin II, thus reducing intra-glomerular hypertension that is postulated to favor albumin filtration; however, the importance of this mechanism remains controversial [63]. ACE inhibitors are also indicated for cardiac failure in combination with relatively low dosages of diuretics. Dry cough is reported in 10 – 15% of patients treated with ACE inhibitors because these drugs also interfere with the breakdown of kinins in the bronchial epithelium. Changing to another ACE inhibitors and ARB may prevent this problem. ACE inhibitors occasionally precipitate acute renal failure, particularly in the elderly and in subjects taking non-steroidal anti-inflammatory
drugs (NSAIDs), or those with bilateral renal artery stenosis. Other side effects (rashes, neutropenia, taste disturbance) are unusual with the low dosages currently recommended but becomes more prominent in patients with renal failure. Because ACE inhibitors cause potassium retention, they should not generally be taken concurrently with potassium-sparing diuretics (spironolactone and amiloride), or potassium supplements. Serum creatinine and potassium levels should be monitored regularly, especially in patients with renal failure or type 4 renal tubular acidosis, in Hyperkalemia can rapidly reach dangerous levels. Ramipril, enalapril, captopril, lisinopril, and perindopril are all established ACE inhibitors that are suitable for use in people with diabetes; enalapril, lisinopril, perindopril, and ramipril are given once a day for hypertension. The first dose of an ACE inhibitor should be small and taken just before bedtime to minimize postural hypotension, which may be marked in subjects receiving diuretics or a strict sodium-restricted diet. A similar problem may arise in patients with autonomic neuropathy. ACE inhibitors are now recommended for patients with left ventricular dysfunction following MI. Ramipril has been shown to prevent cardiovascular morbidity and mortality in high-risk patients with diabetes, with or without pre-existing ischemic heart disease [64].
Angiotensin II type 1 receptor blockers
This promising new class includes losartan, irbesartan, valsartan, candesartan, and telmisartan, which act on the AT1 receptor to reduce BP. They are metabolically neutral [65] and unlike ACE inhibitors, they do not cause cough. They are effective antihypertensive agents in people with diabetes [66] and have been demonstrated to slow the progression of nephropathy in patients with diabetes and different degrees of albuminuria (at RENAAL, IDN, T, and PRIME - 2 studies) [67 – 69]. Losartan has also been shown (in a subgroup of the LIFE study) to be superior to atenolol in reducing both cardiovascular endpoints (by 25%) and overall mortality (by 40%) in high-risk T2DM patients with hypertension and left ventricular hypertrophy [70]. Interestingly, the combination An ACE inhibitor (lisinopril) with an AT1 antagonist (candesartan) was more effective in lowering BP than either agent alone and SAE in patients with T2DM [71]; but lately In the ONTARGET study, no extra benefits on cardiovascular endpoints were noted for the combination of telmisartan and ramipril compared to monotherapy [72].
α1 - Adrenoceptor antagonists
α1 - blockers can effectively lower BP and improve dyslipidemia and insulin sensitivity. Doxazosin is normally well tolerated, especially in combination therapy; side effects include nasal congestion and postural hypotension. Doxazosin has been reported to be inferior to the diuretic chlortalidone in the prevention of stroke and heart failure [73].
Treatment strategies in general, lifestyle modification should be attempted initially for 3 months or more. If moderate hypertension (diastolic BP > 100 mmHg, or systolic BP > 160 mmHg) or signs of hypertensive tissue damages present, drug therapy should be initiated at the outset. Initially, monotherapy with one of the first-line drugs suggested above should be used; the choice is influenced by other factors, such as the coexistence of angina, heart failure, or nephropathy. All drug treatments should be evidence-based and cost-effective for individual patients.
Hypertension in T1DM
ACE inhibitors are especially suitable for patients with albuminuria or more advanced stages of diabetic nephropathy. Diuretics, β1 selective blockers commonly and CCAs are Alternative’ ‘Complementary about BP reduction. If renal function is moderately impaired (serum creatinine values > 150 mole/L), thiazide diuretics become less effective, and furosemide or other loop diuretics should be used instead. However, in established ESRF (serum creatinine > 500 mole/L), furosemide may be toxic, and dialysis must be started. In some patients, hypoglycemia attacks may be masked by the use of beta-blockers.
Hypertension in T2DM
BP control is generally more important than the choice of drug. First-line agents, according to evidence from clinical studies, are ACE inhibitors, ARBs, beta-blockers, low-dose thiazide diuretics (in the elderly), furosemide and CCAs [4 – 8]. Ramipril has evidence-based support for its use in patients with T2DM because of its high cardiovascular risk [64]. Beta-blockers (in combination with low-dose aspirin) are indicated for secondary prevention in patients who have had an MI, as long as no serious contraindications are present. Low doses of thiazide diuretics are useful in elderly patients with diabetes, as this class of drugs has proven efficacy in preventing stroke and all-cause mortality in elderly hypertensive patients [8]. α1 - blockers may be used as part of combination therapy, especially in patients with dyslipidemia (high triglycerides and low HDL cholesterol levels) and prostatic hyperplasia. Indapamide was well tolerated and had no metabolic side effects. Spironolactone may also be of value [74], especially for elderly obese female patients with hypertension and hypovolemia with a low renin profile.
Combination therapy
Combination therapy is needed in most people with diabetes (especially in those with T2DM) to achieve satisfactory BP control [4,5]. It is often better to use low-dose combinations than to increase dosages of single agents, a side effects are commonly dose-dependent. As already mentioned, potassium-sparing agents (spironolactone and amiloride) should not be combined with ACE inhibitors because of the increased risk of hyperkalemia. Certain combinations of antihypertensive drugs have proved very safe and effective at low to moderate doses, for example, ACE inhibitor plus a diuretic, for example in the ADVANCE study [75]; CCA plus ACE inhibitor, for example in the ACCOMPLISH study [76]; selective β1 - blocker plus CCA; or β1 - blocker plus α1 - blocker. In some high-risk patients, combination treatment can also be considered as an initial therapy.
Special considerations in ethnic groups
Hypertension in diabetes represents a serious medical problem in many ethnic groups, including African Americans. Annon-white European patients, beta-blockers, and ACE inhibitors are often less effective at lowering BP because the RAS is already under active. Diuretics and CCAs are often preferred, particularly in African-Americans [78]. The outcome of treating hypertension in diabetes It has long been recognized that effective treatment of hypertension can slow the progression of diabetic nephropathy, lower UAE, and decrease the rate of fall of the GFR [79]. The assumption that improved BP control would improve cardiovascular and other prognoses in T2DM has been confirmed by the UKPDS [4]. In this study, tighter BP control (averaging 144/82 mmHg) for over 8 years led to significant improvements in several outcomes compared with less strict control that averaged 154/87 mmHg (Table 40.4). Interestingly, the most powerful effects were related to microvascular complications (retinopathy and nephropathy), although significant. Reductions were observed in the risk of stroke (44%) and heart failure (56%). MI and peripheral vascular disease showed non-significant reductions. Overall, tight BP control has been proven to provide substantial benefits for patients with hypertension and diabetes. Moreover, this treatment strategy seems to be cost-effective, at least according to the health economics analyses in the UKPDS [80]; however, it must be kept in mind that these benefits will not Lastly, if a continuous BP reduction cannot be achieved long-term, as shown by the 10-year follow-up of the UKPDS [81]
Research method
Research on cardiovascular threat factors has in all likelihood involved a combination of observational research, medical trials, and record evaluation. The intention of the studies changed to picking out and examining various factors that contribute to the development and improvement of cardiovascular ailments.
Results
Studies may also screen several key cardiovascular risk factors that may be associated with an extended probability of developing coronary heart sickness or the prevalence of unfavorable cardiovascular events. These danger factors may also encompass the following.
Excessive blood stress (excessive blood strain): Improved blood pressure levels are a massive danger for cardiovascular sickness, heart assault, and stroke.
Excessive LDL cholesterol: Multiplied stages of LDL cholesterol ("terrible" LDL cholesterol) and reduced degrees of HDL LDL cholesterol ("correct" LDL cholesterol) can contribute to the improvement of atherosclerosis and coronary artery disease.
Smoking: Tobacco smoking is strongly related to an improved threat of cardiovascular ailments due to its risky outcomes on blood vessels and the coronary heart.
Diabetes: Type 1 and type 2 diabetes are related to an improved risk of cardiovascular complications.
Weight problems: More frame weight, particularly inside the belly area, can cause high blood stress, insulin resistance, and exceptional metabolic problems that increase cardiovascular risk.
Sedentary lifestyle: Loss of normal bodily interest can contribute to weight gain, excessive blood pressure, and different threat elements for coronary heart illness.
Circle of relative’s statistics: A circle of relatives’ facts of cardiovascular sickness can also indicate a genetic predisposition to such conditions.
Dangerous diet plan: A healthy eating plan that is excessive in saturated fats, trans fats, salt, and sugars can contribute to various threats to cardiovascular disorders.
Pressure: Chronic stress can lead to dangerous coping mechanisms (e.g., overeating and smoking) and advanced blood pressure, all of which may impact cardiovascular fitness.
Discussion
The discussion of the research results involves interpreting the findings and placing them in the context of existing knowledge in the field. Researchers are likely to discuss the strength of the associations between each risk factor and cardiovascular diseases, as well as the potential mechanisms through which these risk factors exert their effects. Additionally, research might explore how multiple risk factors can interact and compound their effects on cardiovascular health. For example, obesity may worsen the effect of hypertension or diabetes on the heart. Understanding these interactions is crucial for developing effective prevention and treatment strategies. Furthermore, researchers may discuss the public health implications of their findings. Identifying modifiable risk factors can guide policymakers and healthcare professionals in designing interventions to reduce the burden of cardiovascular diseases in the population. These interventions could include lifestyle modifications, smoking cessation programs, promotion of physical activity, and healthier eating habits. It is important to note that the research findings may have limitations such as potential confounding factors, sample size issues, or the specific population studied. Researchers are likely to acknowledge these limitations and suggest avenues for further investigation to strengthen the evidence. Overall, research on cardiovascular risk factors is vital for enhancing our understanding of the pathophysiology of the disease and for guiding preventive measures and treatments to reduce the global burden of cardiovascular diseases.
Conclusion
The diagnosis and treatment of hypertension are of great importance for individuals with diabetes [34,36,82 – 84]. The treatment targets are demanding and require considerable effort from both patients and physicians. However, the benefits are now undisputed. New antihypertensive drugs are constantly being introduced, but their efficacy and tolerability have to be proven. Although some antidiabetic drugs appear to lower BP and blood glucose [85], safety concerns are important. In the future, the application of cardiovascular genomics may substantially change the approach to treating hypertension in diabetes [86], aiming at tailoring treatment according to the Genotype of an individual patient. In addition, further large-scale studies with a large number of hypertensive patients with T2DM are awaited [87]. In the recent ACCORD - Blood pressure study [88] there was no significant. The difference in the primary composite outcome of cardiovascular events between patients randomized to achieve a systolic blood pressure goal below 120 mmHg versus below 140 mmHg, even if a reduction in stroke was noticed (secondary endpoint) in the intensive arm. This means that the optimal blood pressure goal for patients with hypertension and T2DM has not yet been established [89]. Finally, it takes a multifactorial approach to address and treat all major cardiovascular risk factors, not only BP, to achieve lasting cardiovascular protection, as evidenced by the Steno - 2 trial [90].
Declarations
Acknowledgment
The completion of this research project would not have been possible without the contributions and support of many individuals and organizations. We are deeply grateful to all those who played a role in the success of this project We also thank My Mentor [. Naweed Imam Syed Prof. Department of Cell Biology at the University of Calgary and Dr. Sadaf Ahmed Psychophysiology Lab University of Karachi for their invaluable input and support throughout this research. Their insights and expertise were instrumental in shaping the direction of this project.
Declaration of Interest
I at this moment declare that, I have no pecuniary or other personal interest, direct or indirect, in any matter that raises or may raise a conflict with my duties as a manager of my office Management.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Financial support and sponsorship
No Funding was received to assist with the preparation of this manuscript
References
- Kylin E. (1923). Studien ü ber das Hypertone - Hyperglyk ä mie -Hyperurik ä syndrome. Zeitschrift Motel Med, 7:100-112.
Publisher | Google Scholor - Reaven GM. (1988). position of insulin resistance in human sickness Diabetes, 37:1595–1607.
Publisher | Google Scholor - Meigs JB, DAgostino RB Sr, Wilson P, Cupples L.A., Nathan DM, Singer DE. (1997). Hazard variable clustering within the insulin resistance syndrome. The Framingham Offspring have a look at Diabetes, 46:1594-1601.
Publisher | Google Scholor - UK Ability Diabetes. (1998). Take a look at the organization. Tight blood strain management and risk of macro vascular and microvascular headaches in kind 2 diabetes. UKPDS 38 Br Med J, 317:703-713.
Publisher | Google Scholor - Hansson L, Zanchetti A, Carruthers S, Dahl ö f B, Elmfeldt D, Julius S, et al. (1998). Consequences of vast blood-stress decreasing and coffee-dose aspirin in sufferers with high blood stress: maximum crucial effects of the high blood pressure top-rated treatment (warm) randomized trial. Lancet, 351:1755-1762.
Publisher | Google Scholor - Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. (1998). The impact of nisoldipine compared with enalapril on aerobic vascular outcomes in sufferers with non-insulin-structured diabetes and excessive blood stress. N Engl J Med, 338:645-652.
Publisher | Google Scholor - Tuomilehto J, Rastenyte D, Birkenh ä ger WH, Thijs L, Antikainen R, Bulpitt CJ, et al. (1999). Consequences of calcium-channel blockade in older sufferers with diabetes and systolic high blood pressure. N Engl J Med, 340:677-684.
Publisher | Google Scholor - Lindholm LH, Hansson L, Ekbom T, Dahl ö f B, Lanke J, Linjer E, et al. (2000). Evaluation of antihypertensive treatments in stopping automobile cardiovascular activities in elderly diabetic sufferers: effects from the Swedish Trial in vintage sufferers with high blood pressure - 2 have a study enterprise. J Hypertens, 18: 1671-1675.
Publisher | Google Scholor - Wiseman MJ, Viberti GC, waterproof coat D, Jarrett RJ, eager H. Glycemia. (1984). arterial stress, and Microalbuminuria in kind 1 (insulin-structured) diabetes mellitus. Diabetologia, 26:401-405
Publisher | Google Scholor - high blood pressure patients with diabetes should take a look at the organization. hypertension in Diabetes Take a look at HDS II, the expanded threat of cardiovascular complications in hypertensive type 2 diabetic patients. J Hypertens, 11:319-325
Publisher | Google Scholor - Haffner S, Mitchell B, Stern M, Hazuda HP, Patterson JK. (1990). decreased incidence of high blood pressure in Mexican-Americans, 16:225-232.
Publisher | Google Scholor - Salomaa VV, Strandberg TE, Vanhanen H, Naukkarinen V, Sarna S, Miettinen TA. (1991). Glucose tolerance and blood pressure follow-up in middle elderly guys. Br Med J, 302: 493-496.
Publisher | Google Scholor - Cooper R, Cutler J, Designee - Nickens P, Fortmann SP, Friedman L, Havlik R, et al. (2000). Trends and disparities in coronary heart disorder, stroke, and different cardiovascular sicknesses inside the us: findings of the countrywide conference on cardiovascular sickness prevention. Circulation, 102:3137-3147.
Publisher | Google Scholor - DeFronzo R, Ferrandine E. (1991). Insulin resistance: a multifaceted syndrome accountable for NIDDM, weight problems, hypertension, dyslipidemia, and atherosclerotic disorder. Diabetes Care, 14:173-194.
Publisher | Google Scholor - Py ö r ä l ä M, Miettinen H, Halonen P, Laakso M, Py ö r ä l ä okay. (Insulin resistance syndrome predicts the risk of coronary coronary heart disease and stroke in the healthy center - elderly men: the 22 - year compliance with - up outcomes of the Helsinki Policemen have a look at. Arterioscler Thromb Vasc Biol, 20:538-544.
Publisher | Google Scholor - Barker DJP, ed. (1992). Fetal and infant Origins of person ailment. London: British Clinical Journal.
Publisher | Google Scholor - Pinkney JH, Mohamed - Ali V, Denver AE, Foster C, Sampson MJ, Yudkin JS. (1994). Insulin resistance, proinsulin, and ambulatory blood stress in type II diabetes. Hypertension, 24:362-367.
Publisher | Google Scholor - Sch, Randi, Vollenweide, Vollenweide, Nicod P. (1994). Nitric oxide launches accounts for insulin s vascular outcomes in human beings. J Clin invests, 2511-2515.
Publisher | Google Scholor - Rongen GA, Tack CJ. I92001). Triglycerides and endothelial function in the kind 2 diabetes. Eur J Clin Invest, 31:560-562.
Publisher | Google Scholor - DeFronzo RA, Goldberg M, Agus ZS. (1976). The consequences of glucose and insulin on renal electrolyte transport. J CLIN Invests, 8:83-90.
Publisher | Google Scholor - Natali A, Qui ñ ones Galvan A, Santora D, Pecori N, Taddei S, Salvetti A. et, al. (1993). dating among insulin launch, anti-natriuresis, and hypokalemia after glucose ingestion in a regular and hypertensive guy. Clin Sci, 85:327-335.
Publisher | Google Scholor - corridor JE, Summers RL, Brands MW, eager H, and Alonso-Galicia M. (1994). Resistance to metabolic actions of insulin and its position in hypertension. Am J Hypertens, 7:772-788.
Publisher | Google Scholor - Morris ad, Petrie JR, Connell JMC. (1994). Insulin and hypertension. J Hypertens, 12:633-642.
Publisher | Google Scholor - Anderson EA, Balon TW, Hoffman RP, Sinkey CA, Mark AL. (1992). Insulin increases sympathetic interest but now not blood pressure in borderline hypertensive humans. Hypertension, 19:621-627.
Publisher | Google Scholor - Capron L, Jarnet J, Kazandjian S, Housset E. (1986). Growth - selling outcomes of diabetes and insulin on arteries: an in vivo have a look at of rat aorta. Diabetes, 35:973-978.
Publisher | Google Scholor - Mathiesen ER, R ø B, Jensen T, hurricane B, Deckert T.
Publisher | Google Scholor - Walker JD, Tariq T, Viberti GC. (1990). Sodium lithium counter-shipping activity in the crimson cells of sufferers with insulin-based diabetes and nephropathy and their mother and father. Br Med J, 301:635--638.
Publisher | Google Scholor - Drury PL Bodansky HJ, Oddie CJ, Edwards CRW. (1984). elements inside the control of plasma renin activity and awareness in type 1 diabetics. Clin Endocrinol, 20:607- 618.
Publisher | Google Scholor - Zatz R, Brenner BM. (1986). Pathogenesis of diabetic micro angiopathy: the Hemodynamics view. Am J Med, 80:443-453.
Publisher | Google Scholor - Groop L, Ekstrand A, Forsblom C, Widen E, Groop PH. (1993). Insulin resistance, hypertension, and Microalbuminuria in sufferers with type II (non-insulin-based) diabetes mellitus. Diabetologia, 36:642-647.
Publisher | Google Scholor - Liu JE, Palmieri V, Roman NJ, Bella JN, Fabsitz, Hoard BV, et al. (2001). The impact of diabetes in left ventricular filling pattern in normotensive and hypertensive adults: the robust heart study. J Am Coll Cardiol, 37:1943-1949.
Publisher | Google Scholor - Kuperstein R, Hanly P, Niroamand M, Fasson Z. (2001). The importance of age and weight problems at the relation between diabetes and left ventricular mass. J Am Coll Cardiol, 37:1957-1962.
Publisher | Google Scholor - Schernt, Philli, Bretzel R. (1999). This significance off24-hour blood pressure tracking in patients with diabetes mellitus. Dtsch Med Wochenschrift, 124:393-395.
Publisher | Google Scholor - international health corporation – worldwide Society of hypertension pointers for the control of high blood pressure. (1999). recommendations Subcommittee. J Hypertens, 17:151-183.
Publisher | Google Scholor - Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other danger elements, and 12 - yr cardiovascular mortality for men screened inside the multiple threat component Intervention Trial. Diabete Scare, 16:434- 444.
Publisher | Google Scholor - Prevention of coronary heart ailment in medical exercise. guidelines of the second one Joint venture pressure of EU and other Societies on coronary prevention. (1998). summary of recommendations. Eur coronary heart J, 19:1434-1503.
Publisher | Google Scholor - Vessby B, Tengblad S, Lithell H. (1994). Insulin sensitivity is associated with serum lipids' fatty acid composition and skeletal muscle phospholipids in 70–12-month-old vintage men. Diabetologia, 37:1044-1050.
Publisher | Google Scholor - Stewart MJ, Jyothinagaram S, McGinley IM. (1994). Padfield Pl Cardiovascular outcomes of cigarette smoking: ambulatory blood pressure and BP variability. J Hum Hypertens, 8:19-22.
Publisher | Google Scholor - Facchini F, Hollenbeck C, Jeppesen J, Chen YD and Reaven GM. (1992). Insulin resistance and cigarette smoking. Lancet, 39:1128-1130.
Publisher | Google Scholor - Chase PH, Garg SK, Marshall G, Berg CL, Harris S, Jackson WE, et al. (1991). Cigarette smoking increases the risk of albuminuria amongst topics with type 1 diabetes. JAMA, 265:614-617.
Publisher | Google Scholor - treatment of moderate hypertension studies group. (1991). The treatment of moderate high blood pressure examines a randomized, placebo-controlled trial of a nutritional-hygienic routine together with various drug mono therapies. Arch Intern Med, 151:1413-1423.
Publisher | Google Scholor - Weidman P, Beretta - Piccoli C, Keusch G, Gl ü ck Z, Mujagic M, Grimm M., et al. (1979(. Sodium: extent aspect, cardiovascular reactivity, and hypotensive mechanism of diuretic therapy in slight high blood pressure related to diabetes mellitus. Am J Med, 67:779-784.
Publisher | Google Scholor - Pollare T, Lithell H., and Berne C. (1989). A contrast of the consequences of hydrochlorothiazide and captopril on glucose and lipid metabolism in sufferers with excessive blood pressure. N Engl J Med, 321:868-873.
Publisher | Google Scholor - Berglund G, Andersson O, and Widgren B. (1986). Low-dose antihypertensive remedy with a thiazide diuretic is not diabetogenic: a ten-year controlled trial with Bendroflumethiazide, Acta Med Scand, 220:419-424.
Publisher | Google Scholor - MacMahon SW, Macdonald GJ. (1987). Antihypertensive remedy and plasma lipoprotein variety: the establishments in data from a population examine. Am J Med, eighty (Suppl. 2A): 40-47.
Publisher | Google Scholor - lessen JD, Pressel SL, Cutler JA, Savage PJ, Applegate WB, Black H, et al. (1996). Systolic high blood pressure in the aged application Cooperative research the impact of diuretic-based, totally antihypertensive remedy on cardiovascular contamination risk in older diabetic sufferers with remote systolic immoderate blood stress. JAMA, 276:1886-1892.
Publisher | Google Scholor - Alderman MH, Cohen H, Madhavan S. (1999). Diabetes and cardiovascular Sports in diabetes sufferers: excessive blood strain, 33:1130-1134.
Publisher | Google Scholor - Pollare T, Lithell H, Selinus I, and Berne C. (1989). Insulin sensitivity ultimately treatment with atenolol and metoprolol: a randomized, double-blind examine of results on carbohydrate and lipoprotein metabolism in hypertensive sufferers. Br Med J, 198:115-1157.
Publisher | Google Scholor - Gress TW, Nieto FJ, Shahar E, Wofford MR, and Brancati FL. (2000). high blood pressure and antihypertensive treatments as danger elements for type 2 diabetes mellitus. Atherosclerosis has a risk within the community; take a look at it. N Engl J Med, 342:905-912.
Publisher | Google Scholor - Sawicki PT, Siebenhofer A. (2001). Beta-blocker remedy in diabetes mellitus. J Intern Med, 250:11-17.
Publisher | Google Scholor - Blohme G, and Smith’s. (1979). impact off cardioselectivity and non-selective beta-blockbuster hypotriglyceridemic in insulin-immunoreactive diabetics. Lancet, 458-462.
Publisher | Google Scholor - Hjalma, Goldstein, Faberge, Wede, Waagst, Kjekshu, et al. (2000). gain: HF takes look att the company; effects of managed release metoprolol on widespread mortality, hospitalizations, and well, being in patients with coronary heart failure: the Metoprolol CR/XL Randomized Intervention Trial in Congestive Coronary coronary heart Failure (gain HF) JAMA, 283:1295-1302.
Publisher | Google Scholor - Krum H, Ninio D., and MacDonald P. (2000). Baseline predictors of tolerability to carvedilol in patients with chronic coronary heart failure. coronary coronary coronary heart, 84:615-619.
Publisher | Google Scholor - There are 54 potential Diabetes examination institutions in the United Kingdom. (1998). effectiveness of atenolol and Captopril in decreasing the risk of macro vascular and microvascular complications in kind 2 diabetes: UKPDS 39. Br Med J, 317:713-720.
Publisher | Google Scholor - Kjekshus J., Gilpin E., Cali G., Blackey AR., Henning H., and Ross J. (1990). Prediabetics patients and beta-blockers after acute myocardial infarction. Eur Heart J, 11:43-50.
Publisher | Google Scholor - Chellingsworth MC Kendall MJ, Wright ad Singh BM and Pasi J. (1989). results of verapamil, diltiazem, nifedipine, and propranolol on metabolic manipulation in hypertensives with non-insulin-dependent diabetes mellitus. J Hum Hypertens, 3:35-39.
Publisher | Google Scholor - Bakris GL, Weir MR, DeQuattro V, and McMahon FG. (1998). consequences of an ACE inhibitor/calcium antagonist aggregate on proteinuria in diabetic nephropathy. Kidney Int, 54:1283-1289.
Publisher | Google Scholor - Pah, Psat, Alderma, Applegate, Williamson J, Cavazzini C., et al. (2000). health results associated with calcium antagonists compared with different first-line antihypertensive healing procedures: a meta-analysis of randomized managed trials. Lancet, 356:1949-1954.
Publisher | Google Scholor - Nea, MacMahon S., and Chapman N. (2000). Blood pressure lowering Treatment Trialists’ Collaboration outcomes of ACE inhibitors, calcium antagonists and other blood-strain-lowering tablets: results of prospectively designed overviews of randomized trials. Lancet, 356: 1955-1964.
Publisher | Google Scholor - Lithell H. (1991). Effects Effects of antihypertensive pills on insulin, glucose,e, and lipid metabolism. Diabetes Care, 14:203-209.
Publisher | Google Scholor - Herings RM, de Boer A, Stricker BH, Leufkens HG, Porsius A. (1995). Hypoglycemia is associated with the use of inhibitors of the angiotensin-converting enzyme. Lancet, 345:1195-1198.
Publisher | Google Scholor - Lewis EJ, Hunsickler LG, Bain RP, and Rohde RD. (1993). The impact of angiotensin-changing enzyme inhibition on diabetic nephropathy. N Engl J Med, 329:1456-1462.
Publisher | Google Scholor - bank N, Klose R, Aynedjan HS, Nguyen D, Sablay LB. (1987). proof against accelerated glomerular pressure, initiating diabetic nephropathy. Kidney Int, 31:898-905.
Publisher | Google Scholor - coronary heart result ins Prevention evaluation. (2000). take a look native. effects of ramipril on cardiovascular and microvascular effects in humans with diabetes mellitus: results of the desire take a look at and MICRO - wish sub-study. Lancet, 355:253-259.
Publisher | Google Scholor - Good friends TL, Elliott ME, and Catt KJ. (1996). Angiotensin receptors and their antagonists. N Engl J Med, 334:1649-1654.
Publisher | Google Scholor - Ruilope L. (2000). RAS blockade: new possibilities in the treatment of complications of diabetes Coronary Heart, 84:32-34.
Publisher | Google Scholor - Brenner B, Cooper ME, de Zeeuw D, de Zeeuw D, Keane WF, MitchWE et al. (2001). 's results of losartan on renal and cardiovascular effects in sufferers with type 2 diabetes and nephropathy. N Engl J Med, 345:861-869.
Publisher | Google Scholor - Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al. (2001). Reno protective effect of the angiotensin-receptor antagonist irbesartan in sufferers with nephropathy due to type 2 diabetes, N Engl J Med, 345:851-859.
Publisher | Google Scholor - Parving HH, Lehnert H, Bröckner- Mortensen J, Gomis R, and AndersenS. (2001). Arner P; Irbesartan in sufferers with type 2 Diabetes and Microalbuminuria Study Group The impact of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med, 345:870-878.
Publisher | Google Scholor - Lindholm LH, Ibsen H, Dahl ö f B, Devereux RB, Beevers G, de Faire U et al. (2002). Cardiovascular morbidity and mortality in patients with diabetes inside the Losartan Intervention For Endpoint reduction in high blood pressure examination (life): a randomized trial against atenolol. Lancet, 359:1004-1008.
Publisher | Google Scholor - Mogensen CE, Neldam S, Tikkanen I, Oren S, Viskoper R, Watts RW, et al. (2000). Randomized managed trial of dual blockade of renin-angiotensin and non - insulin-structured diabetes: the Candesartan and Lisinopril Microalbuminuria (CALM): have a look at Br Med J, 321:1440-1444.
Publisher | Google Scholor - ONTARGET. (2008). investigators in patients with telmisartan, ramipril, or both There is an excessive risk of vascular events. N Engl J Med, 358:1547-1559.
Publisher | Google Scholor - Major Cardiovascular Events ALLHAT Collaborative Center Hypertensive patients randomized to doxazosin and chlorthalidone. (2008). Antihypertensive and lipid-lowering treatment to preserve the coronary heart Attack Test (ALLHAT). JAMA, 283:1967-1975.
Publisher | Google Scholor - Ramsay LE, Yeo WW and Jackson PR. (1992). Diabetes mellitus, impaired glucose tolerance, and insulin resistance when taking diuretics. European Heart J, 13:68-71.
Publisher | Google Scholor - Patel A; Combined group effect of perindopril and indapamide combination sets on macro-vascular and microvascular effects in patients with type 2 diabetes (so-called. Boost test: Lancet 2007 randomized controlled trial, 370:829-840.
Publisher | Google Scholor - Jamerson OK, Weber MA, Bakris GL, Dahl of B., Pitt B., Shea W. (2008). and others. benazepril + amlodipine or Hydrochlorothiazide N Engl J for Hypertension in Intermediate-Risk Patients Honey, 359:2417-2428.
Publisher | Google Scholor - Jamerson, in Penalty, de Quatro V. (1996). The Effect of Race on Responses antihypertensive drugs. Hundred Days: 22C-32C, American Journal of Medicine.
Publisher | Google Scholor - Flack JM, Hamati M. R. (1999). efractory Hypertensive Population: It has a good reputation among Africans and people with type 2 diabetes. J. Hypertens, 17: S19-SS24.
Publisher | Google Scholor - Parving H.H., Andersen A.R., Smidt W.M., Hommel E., Mathisen E.R., Svendsen P.A. (1987). Effects of antihypertensive drugs on renal function with diabetic nephropathy. Br Med J Clin Res Ed, 294:1443-1447
Publisher | Google Scholor - uk prospective Diabetes observer group. (1998). price-effectiveness analysis of stepped-forward blood pressure control in hypertensive sufferers with kind 2 diabetes: UKPDS forty. Br Med J, 317:720-726.
Publisher | Google Scholor - Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. (2008). long - period follow-up after tight manipulation of blood strain in type 2 diabetes. Engl J Med, 359:1565-1576.
Publisher | Google Scholor - Chobanian AV, Bakris GL, Black HR, Cushman WC, green los angeles, Izzo JL Jr, et al. (2003). Countrywide Coronary Heart, Lung, and Blood Institute Joint Countrywide Committee on Prevention, Detection, evaluation, and Remedy of high blood strain; excessive Blood strain schooling program Coordinating Committee. The seventh record of the Joint country-wide Committee on Prevention, Detection, evaluation, and Remedy of Excessive Blood Pressure: the JNC 7 file. JAMA, 289:2560-2572.
Publisher | Google Scholor - Rydén L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, et al. (2007). Task pressure on Diabetes and Cardiovascular illnesses of the European Society of Cardiology (ESC); European Association for the Have a Look at Diabetes (EASD) pointers on diabetes, Diabetes and cardiovascular sicknesses: government precis. Eur coronary heart J, 28:88-136.
Publisher | Google Scholor - Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G., et al. (2007). The undertaking force for the management of Arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). management of arterial high blood Pressure of the European Society of high blood pressure (EU Society of Cardiology: 2007 Recommendations for the control of arterial hypertension. J Hypertens, 25:1105 -1187.
Publisher | Google Scholor - Sarafi dis P, Nilsson PM. (2006). The effects of thiazolidinedione compounds on blood pressure stages: a systematic evaluation. Blood stress, 15:135-150.
Publisher | Google Scholor - Pratt RE, Dzau VJ. (1999). Genomics and hypertension: standards, potentials, and opportunities. Hypertension, 33:238-247.
Publisher | Google Scholor - Lauritzen T, Griffin S, Borch - Johnsen okay Wareham NJ, Wolffen buttel BH, Rutten G. (2000). Anglo-Danish-Dutch looks at an in-depth remedy in humans with displays Detected Diabetes in Primary Care. The ADDITION Take a look at the proposed trial of the cost-effectiveness of an intensive multifactorial intervention on morbidity and mortality among human beings with kind 2 diabetes detected through screening. Int J Obes Relat Metab Disord, 24(3): S6-11.
Publisher | Google Scholor - The ACCORD. (2010). study organization consequences of extensive Blood - strain manipulation in type 2 Diabetes Mellitus. N Engl J Med.
Publisher | Google Scholor - Mancia G, Laurent S, Agabiti - Rosei E Ambrosioni E, Burnier M, Caulfi eld MJ, et al. (2009). Reappraisal of EU tips on hypertension control: an ecu Society of Hypertension venture force document. J Hypertens.
Publisher | Google Scholor - Gaede P, Lund - Andersen H, Parving H - H, Pedersen O. (2008). Effect of a multifactorial intervention on mortality in kind 2 diabetes. N Engl J Med, 358:580-591.
Publisher | Google Scholor - Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, et al. (2000). Association of systolic blood stress bloodstreams with macro vascular and microvascular headaches of type 2 diabetes (UKPDS 36): prospective observational have a look at. BMJ, 32 (7258): 412-419.
Publisher | Google Scholor