Review Article
Calcium Pyrophosphate Deposition Disease
1Department of chemistry Sri Sharda Group of Institutions Lucknow U.P. India.
2Department of Biochemistry, Dolphin Institute Dehradun U.K. India.
*Corresponding Author: D.K. Awasthi, Department of Chemistry, Sri J.N.M.PG College, Lucknow UP, India.
Citation: Awasthi D. K, Awasthi G. (2023). Calcium Pyrophosphate Deposition Disease. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(6):1-5. DOI: 10.59657/2837-4681.brs.24.087
Copyright: © 2024 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 09, 2024 | Accepted: May 23, 2024 | Published: May 31, 2024
Abstract
1Department of chemistry Sri Sharda Group of Institutions Lucknow U.P. India.
2Department of Biochemistry, Dolphin Institute Dehradun U.K. India.
Keywords: syndrome; joints; inflammatory; pseudogout
Introduction: Description
Chondrocalcinosis and CPPD crystals may be associated with certain underlying diseases such as trauma to the joint, hyperparathyroidism, hypomagnesemia, hypophosphatasia, hypothyroidism, and hemochromatosis. This highlights the importance of addressing other possible underlying diseases when evaluating the patient with CPPD and chondrocalcinosis.
The CPPD disease encompasses a variety of clinical manifestations:
- Asymptomatic to gout-like symptoms (pseudogout),
- Rheumatoid arthritis-like symptoms (pseudo-rheumatoid arthritis), and
- Osteoarthritis-like symptoms (pseudo-osteoarthritis).
Calcium pyrophosphate deposition disease is distinguished by acute attacks of synovitis that mimic gout. These acute or subacute attacks can involve one or multiple joints, but usually not more than four or five joints. Similar to gout, CPPD disease can manifest with systemic features such as fevers, malaise, leukocytosis, and elevated acute-phase reactants (sedimentation rate and CRP). Acute attacks may be indistinguishable from acute gout. In fact, it is often difficult to differentiate both without a synovial fluid analysis. Patients have joint pain, synovitis with joint tenderness, and swelling. Although CPPD disease and gout share similar joint predilection, CPPD disease tends to affect larger joints (knee joints) more commonly than gout and smaller joints (first metatarsophalangeal joints) less commonly than gout. Calcium pyrophosphate deposition disease also affects the elbow, shoulder, wrist, and metacarpophalangeal joints. Because acute CPPD disease closely resembles gout, the definitive diagnosis often requires synovial fluid analysis. Synovial fluid should be microscopically analyzed for cell count and crystal analysis under compensated polarizing microscopy. In addition, fluid should be examined by Gram stain and culture, especially if crystals are not found. On synovial fluid polarization, CPPD crystals might not be as evident as MSU crystals. They are weakly birefringent under polarized light and have a rhomboid or rod-shaped appearance. They are seen either intracellularly or extracellularly; however, detection might not be as accurate if fluid analysis is delayed. In addition, because CPPD disease and gout can coexist, MSU crystals might be observed. White cell counts can range from a few thousand cells up to 80,000 to 100,000 per high-power field.
Figure 1
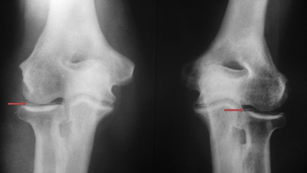
Radiographs can show chondrocalcinosis in the joint involved and other more typical joints even if CPPD disease is not clinically active at the time of presentation. Radiographs can help confirm the clinical impression (especially the knee joints, wrists, and anteroposterior view of the pelvis) and extent of joint degeneration; however, radiographs are not required to make the diagnosis once CPPD crystals are seen under polarized light. Chondrocalcinosis is seen in the knees (hyaline cartilage and menisci), the wrists (fibrocartilage), and other joints such as intervertebral discs and symphysis pubis. Other radiographic features include joint space narrowing, subchondral new bone formation, normal mineralization, cysts more prominent than in osteoarthritis, bilateral preponderance, and osteophyte formation. Certain metabolic conditions associated with CPPD disease, such as in hemochromatosis, have characteristic findings such as joint narrowing of the metacarpophalangeal joint spaces, squaring of the bone ends, subchondral cysts, and hook-like osteophytes on the radial aspects of the metacarpal heads, especially the second and third metacarpophalangeal joints Most of the differential diagnosis factors with gout can be considered here. Infection is always a major differential, especially in the patient presenting with new acute monoarticular arthritis.
In addition, septic arthritis can coexist in a joint that has been or is involved in an acute CPPD disease attack as with gout. Thus, it is important to aspirate the involved joint whenever possible for microscopic examination of the synovial fluid and Gram stain and culture. Other differentials include trauma, bleeding, and other crystal-deposit diseases. Calcium pyrophosphate deposition disease may mimic polymyalgia rheumatica. The treatment of CPPD disease is mostly tailored to the manifesting symptoms. In patients presenting with one or two points of acute synovitis and no infection, rapid relief of pain and inflammation is accomplished with joint aspiration and steroid injection. Many patients find relief from the joint aspiration itself. When more than two joints are involved, it is not feasible to inject all the joints, so treatment is directed more toward systemic therapy. The side effects and toxicities of NSAIDs, colchicine, or systemic glucocorticoids are similar to those for patients with gout. Colchicine at a dose of 0.6 mg once or twice daily may be effective as a prophylactic measure to reduce the number of attacks in a year, especially in patients who experience three or more attacks a year. Unlike gout, however, there are no hypouricemic equivalents to improve the long-term control of acute attacks or to prevent or reverse CPPD disease. The outcome of patients with CPPD disease is influenced by genetic predisposition, extent of crystal deposition and joint degeneration, and aggravating factors from the underlying associated diseases. some patients did not have progressive disease. Because CPPD disease is associated with variety of underlying conditions, practitioners should screen for hyperparathyroidism, hypothyroidism, hypomagnesemia, hypophosphatasia, and hemochromatosis. Blood should be tested for intact parathyroid hormone, calcium, phosphorous, thyroid-stimulating hormone, magnesium, ferritin, iron transferrin, and alkaline phosphatase. Treatment is recommended for any associated diseases; however, it is unclear if treatment of comorbid conditions would decrease the chondrocalcinosis or reverse joint degeneration. Crystal deposition disease is a relatively common condition. Gout and CPPD disease are the most common of these disorders, but practitioners need to be aware of the presence of other types of crystal arthropathy, such as hydroxyapatite crystal deposition disease. In this case, crystals might not be seen on classic synovial analysis and some may require special staining. Gout and pseudogout can manifest with similar symptoms, and their clinical presentation might not be distinguishable; thus, it is essential to aspirate the affected joint or bursa for synovial fluid and crystal analysis whenever possible. Cell count, Gram stain, and culture, in the right clinical setting, should be sought. Once the diagnosis is made, treatment for acute attack should be commenced using the least toxic agent or the one that carries least risk for the patient. Treatment should be initiated while taking into consideration other comorbid conditions, such as renal disease, gastric disease, organ transplant, drug interactions, and others, because these will affect the choice of therapy. In the case of gout, once the acute disease has resolved, the patient should be followed to assess for indications and need for hypouricemic therapy. New drugs are on the horizon for managing chronic tophaceous gout. Over the years, several medications have been approved for the management of gout, such as febuxostat and pegloticase. Additional medications, such as IL-1 inhibitors and biologic therapy are being investigated, allowing for additional treatment options for acute crystalline arthritis with gout and CPPD disease. It is essential for practitioners to keep current with new research data on the indications, safety, and efficacy of these drugs to use them competently in clinical practice.
Conclusion
- In patients presenting with acute joint swelling, the differential diagnosis should include evaluation for infection.
- Joint aspiration should be considered in acute swollen joints, if possible, and fluid should be analyzed for cell count, cultures, and crystals.
- The technical standard for diagnosing gout or CPPD disease has been synovial fluid analysis using polarized light microscopy. Additional investigational modalities are proving beneficial such as high-resolution ultrasound and dual-energy CT studies; however, it is important to note that these may not replace the utility of synovial fluid analysis to exclude infections.
- The examiner should be familiar with and trained in crystal identification using polarized light microscopy.
- The MSU crystals appear yellow when parallel to the axis and blue when perpendicular; calcium pyrophosphate dihydrate crystals appear blue when parallel to the axis and yellow when perpendicular.
- The selection of therapy for acute gout or CPPD disease should consider the patient's comorbidities and risks with the medication.
- Acute gout and CPPD disease may be treated with colchicine, NSAIDs, or corticosteroids (systemic or intra-articular).
- Treatment of chronic gout and hyperuricemia requires a hypouricemic agent.
- New drugs being investigated for the management of gout (and, possibly, CPPD disease) may offer additional treatment options, especially in patient who are unable to take the available drug therapy.
References
- Lawrence RC, Felson DT, Helmick CG, et al. (2008). National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum, 58:26.
Publisher | Google Scholor - Roddy E, Doherty M. (2010). Epidemiology of gout. Arthritis Res Ther; 12:223.
Publisher | Google Scholor - Zhu Y, Pandya BJ, Choi HK. (2011). Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum, 63:3136-3141.
Publisher | Google Scholor - Mikuls TR, Farrar JT, Bilker WB, et al. (2005). Gout epidemiology: results from the UK general practice research database, 1990–1999. Ann Rheum Dis, 64:267-272.
Publisher | Google Scholor - Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R. (2004). Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol, 31:1582-1587.
Publisher | Google Scholor - Choi HK, Curhan G. (2005). Gout: epidemiology and lifestyle choices. Curr Opin Rheumatol, 17:341-345.
Publisher | Google Scholor - Emmerson BT. (1996). The management of gout. N Engl J Med, 334:445-451.
Publisher | Google Scholor - Choi HK, Mount DB, Reginato AM; (2005). American College of Physicians; American Physiological Society. Pathogenesis of gout. Ann Intern Med, 143:499-516.
Publisher | Google Scholor - Martinon F, Glimcher LH. (2006). Gout: new insights into an old disease. J Clin Invest, 116:2073-2075.
Publisher | Google Scholor - Pascual E, Jovani V. (2005). Synovial fluid analysis. Best Pract Res Clin Rheumatol, 19:371-386.
Publisher | Google Scholor - Choi MH, MacKenzie JD, Dalinka MK. Imaging features of crystal-induced arthropathy. Rheum Dis Clin North Am, 32:427-446.
Publisher | Google Scholor - Bongartz T, Glazebrook KN, Kavros SJ, et al. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis, 74:1072-1077.
Publisher | Google Scholor - Frediani B, Filippou G, Falsetti P, et al. (2005). Diagnosis of calcium pyrophosphate dihydrate crystal deposition disease: ultrasonographic criteria proposed. Ann Rheum Dis, 64:638-640.
Publisher | Google Scholor - Thiele R, Schlesinger N. (2007). Diagnosis of gout by ultrasound. Rheumatology, 46:1116-1121.
Publisher | Google Scholor - Khanna D, Fitzgerald JD, Khanna PP, et al. (2005). 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 64:1431-1446.
Publisher | Google Scholor - Khanna D, Khanna PP, Fitzgerald JD, et al. (2005). American College of Rheumatology guidelines for management of gout. Part 2: therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res (Hoboken), 64:1447.
Publisher | Google Scholor - Becker MA, Schumacher HR Jr, Wortmann RL, et al. (2005). Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med, 353:2450-2461.
Publisher | Google Scholor - Borstad GC, Bryant LR, Abel MP, et al. (2004). Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol, 31:2429-2432.
Publisher | Google Scholor - Faruque LI, Ehteshami-Afshar A, Wiebe N, Tjosvold L, Homik J, Tonelli M. (2013). A systematic review and meta-analysis on the safety and efficacy of febuxostat versus allopurinol in chronic gout. Semin Arthritis Rheum, 43:367-375.
Publisher | Google Scholor - Schlesinger N. (2004). Management of acute and chronic gouty arthritis: present state-of-the-art. Drugs, 64:2399-2416.
Publisher | Google Scholor - Becker MA, Schumacher HR Jr, Wortmann RL, et al. (2005). Febuxostat, a novel nonpurine selective inhibitor of xanthine oxidase: a twenty-eight–day, multicenter, phase II, randomized, double-blind, placebo-controlled, dose-response clinical trial examining safety and efficacy in patients with gout. Arthritis Rheum, 52:916-923.
Publisher | Google Scholor - Tayar JH, Lopez-Olivo MA, Suarez-Almazor ME. (2005). Febuxostat for treating chronic gout. Cochrane Database Syst Rev, 11:CD008653.
Publisher | Google Scholor - Schumacher HR Jr, Becker MA, Lloyd E, MacDonald PA, et al. (2009). Febuxostat in the treatment of gout: 5-yr findings for the FOCUS efficacy and safety study. Rheumatology, 48:188-194.
Publisher | Google Scholor - Choi HK, Atkinson K, Karlson EW, et al. (2004). Alcohol intake and risk of incident gout in men: a prospective study. Lancet, 363:1277-1281.
Publisher | Google Scholor - Choi HK, Atkinson K, Karlson EW, et al. (2004). Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med, 350:1093-1103.
Publisher | Google Scholor - Lee SJ, Terkeltaub RA, Kavanaugh A. (2006). Recent developments in diet and gout. Curr Opin Rheumatol, 18:193-198.
Publisher | Google Scholor - De Souza AW, Fernandes V, Ferrari AJ. (2005). Female gout: clinical and laboratory features. J Rheumatol, 32:2186-2188.
Publisher | Google Scholor - Stamp L, Searle M, O'Donnell J, Chapman P. (2005). Gout in solid organ transplantation: a challenging clinical problem. Drugs, 65:2593-2611.
Publisher | Google Scholor - Wilkins E, Dieppe P, Maddison P, Evison G. (1983). Osteoarthritis and articular chondrocalcinosis in the elderly. Ann Rheum Dis, 42:280-284.
Publisher | Google Scholor - Neame RL, Carr AJ, Muir K, Doherty M. (2003). UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis, 62:513-518.
Publisher | Google Scholor - Tenenbaum J, Muniz O, Schumacher HR, et al. (1981). Comparison of phosphohydrolase activities from articular cartilage in calcium pyrophosphate deposition disease and primary osteoarthritis. Arthritis Rheum, 24:492-500.
Publisher | Google Scholor - Johnson K, Pritzker K, Goding J, Terkeltaub R. (2001). The nucleoside triphosphate pyrophosphohydrolase isozyme PC-1 directly promotes cartilage calcification through chondrocyte apoptosis and increased calcium precipitation by mineralizing vesicles. J Rheumatol, 28:2681-2691.
Publisher | Google Scholor - Dieppe PA, Alexander GJ, Jones HE, et al. (1982). Pyrophosphate arthropathy: a clinical and radiological study of 105 cases. Ann Rheum Dis, 41:371-376.
Publisher | Google Scholor - Adamson TC 3rd, Resnik CS, Guerra J Jr, et al. (1983). Hand and wrist arthropathies of hemochromatosis and calcium pyrophosphate deposition disease: distinct radiographic features. Radiology, 147:377-381.
Publisher | Google Scholor - Alvarellos A, Spilberg I. (1986). Colchicine prophylaxis in pseudogout. J Rheumatol, 13:804-805.
Publisher | Google Scholor - Doherty M, Dieppe P, Watt I. (1993). Pyrophosphate arthropathy: a prospective study. Br J Rheumatol, 32:189-196.
Publisher | Google Scholor