Case report
Button Battery Ingestion: With Fatal Complication of Tracheoesophageal Fistula
- Kenneth Mlay 1,2*
- Desderius Chussi 1,2
- Bernard Minja 1,2
- Philibert Mtenga 1,2
- Adinan Sadiq 3
- Peter Ernest Kipiki 2
1.Department of otorhinolaryngology Kilimanjaro Christian Medical University College, Moshi, Tanzania.
2.Department of otorhinolaryngology Kilimanjaro Christian Medical Centre, Moshi, Tanzania
3.Department of Radiology and Imaging Kilimanjaro Christian Medical University College, Moshi, Tanzania.
*Corresponding Author: Kenneth Mlay, Department of otorhinolaryngology Kilimanjaro Christian Medical University College, Moshi, Tanzania, Department of otorhinolaryngology Kilimanjaro Christian Medical Centre, Moshi, Tanzania.
Citation: Mlay K, Chussi D, Minja B, Mtenga P, Sadiq A, et al. (2024). Button Battery Ingestion: with Fatal Complication of Tracheoesophageal Fistula, International Clinical Case Reports and Reviews, BioRes Scientia Publishers. 2(1):1-4. DOI: 10.59657/2993-0855.brs.24.003
Copyright: © 2024 Kenneth Mlay, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 30, 2023 | Accepted: September 12, 2023 | Published: January 03, 2024
Abstract
Ingestion of button batteries has been seen with increasing frequency over the past decade. Several small number of reported cases, their impaction in the esophagus has led to serious, sometimes fatal, complications. The management of these cases has varied from expectant, supportive therapy to early surgical intervention. We report a case of button battery ingestion that were diagnosed late and resulted in a fatal complication of tracheoesophageal fistula with migratory to the deep mucosa of the thorax which was managed by open surgery.
Keywords: Tracheo esophageal fistula; Foreign body ingestion; children
Introduction
Button batteries ingestion has been seen with increasing frequency in children over the past decade. Several small number of reported cases, their impaction in the oesophagus has led to serious, sometimes fatal, complications. Witnessing the ingestion of a foreign body plays a major role in early diagnosis and prompt urgent intervention, however, in children it is almost always impossible. A high index of suspicion, clinical evaluation, and proper investigations are essential to differentiate FB ingestion or inhalation from other upper aerodigestive tract infections in children. Delayed or missed diagnosis of FB ingestion hinders appropriate and urgent intervention in cases of ingestion of a dangerous FB such as a battery. In this report, we present a case of complications of FB ingestion of button battery and address the importance of a high index of suspicion for signs and symptoms of FB ingestion.
Case Presentation
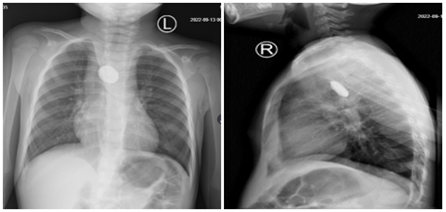
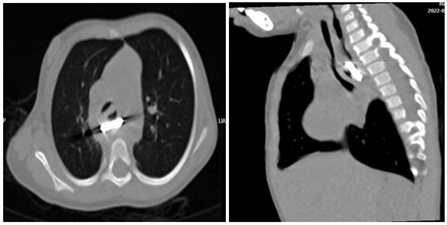
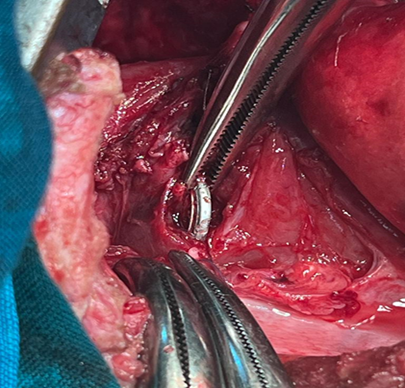
A 2 years old female child with a one-year history of poor feeding, with several episodes of vomiting has been treated for recurrent tonsillitis at a primary care facility where a decision was reached to do a tonsillectomy. Second-day post tonsillectomy the child developed to have difficulty in breathing. A chest x-ray (PA and Lateral) (Figure 1) was ordered and a double-ring round opacification was seen in the oesophagus at the level above the carina. Rigid esophagoscopy was performed and a metallic object was identified. Initial attempts to remove failed. The child was then referred to our tertiary hospital. On arrival, the child was conscious, afebrile not dyspnoeic with stable vitals. A subsequent attempt at rigid esophagoscopy and removal of the FB was unsuccessful. The cardiothoracic team was consulted. A chest CT scan was ordered Figure 2 which showed a round radio-opaque foreign body in the mid-oesophagus and perforation of the mid-oesophagus noted anterior to the lodged foreign body embedded in the deep mucosa with evidence of tracheal and oesophageal communication. A decision was reached to perform a thoracotomy. Intraoperatively, through right posterolateral thoracotomy and an extra pleural approach. The trachea and the oesophagus were found to be embedded in an inflamed fibrotic pleural layer. Dissection to expose the structures was accomplished, and FB was felt at the anterior portion of the oesophageal wall adjacent to the carina. Oesophagostomy was done, and retrieval of the foreign body was accomplished Figure 3. An NGT was inserted, and esophagoplasty was done. A Thoracostomy tube size 14 was inserted and secured. Postoperatively the patient was kept on intravenous antibiotics and dexamethasone injections, physiotherapy and NGT retained for two weeks. 5 days post-thoracotomy, the thoracostomy tube was removed after a control chest x-ray. 7 days post operation the child was doing fine with no fever or difficulty in breathing, Patient was then discharged. NGT was retained for 6 weeks, upon removal of NGT and feeding there was no choking and was scheduled consecutive monthly review at our clinic for 3 months and recovered completely.
Figure 1: Chest x-ray (AP and lateral) views demonstrate a round radio-opaque foreign body in the mid oesophagus shown by a blue arrow at the level above the carina.
Figure 2: Non-contrast CT of the chest (axial and sagittal views) show a round radio-opaque foreign body in the mid oesophagus. Trachea is shown by the blue arrow. Perforation of the mid oesophagus noted anterior to the lodged foreign body as shows by red arrow. No evidence of trachea-oesophageal fistula.
Figure 3: Extraction of the Lithium battery from the oesophagus through thoracotomy.
Discussion
FB ingestion is more prevalent in children especially those below 5 years of age. This may be attributed to their tendency to explore the environment by placing objects in their natural orifices, playing while having objects in their mouths, and less controlled coordination of swallowing [1]. Prevalence is reported to vary between 57 and 80%. Foreign body aspiration or ingestion in adults is often accidental. Commonly ingested objects by children include coins, fish bones, metallic objects, rubber and plastic materials (from toys), and glass objects. Of these coins are the commonest [2, 3]. Button batteries account for less than 2% of ingested FB however this prevalence is on the rise as now button batteries are found in many children’s toys, increasing their accessibility to children [4]. Clinical presentation of a foreign body in the oesophagus may be asymptomatic or symptomatic with gastrointestinal symptoms or with respiratory symptoms [5, 2, 6]. At times, these symptoms produce a nonspecific picture such that a child might present with vomiting, fever, lethargy, poor appetite, irritability, cough, stridor, wheezing, and dehydration [7] as noted in our cases, which were thought to be common respiratory tract infection not responding well to treatment. Overall being asymptomatic, vomiting and drooling have been found to be the most predominant presenting symptoms in cases of ingested FB [5].
Mechanisms of injury caused by batteries show why ingestion of batteries is very dangerous compared to other commonly FB ingested such as coins. The mechanisms of injury proposed include electrolyte leakage from a battery, alkali produced ‘‘de novo’’ from external current, mercury toxicity, and pressure necrosis [8]. All these together result in local damage and even systemic effects and hence cause fatal complications. Some of the reported complications can be immediate or delayed. For example, oesophageal or aortic perforation, tracheoesophageal fistula, tracheoesophageal fistula with a fatal haemorrhagic shock due to erosion of the inferior thyroid vessels, oesophageal bleeding, rare cases of bilateral vocal cord paralysis, and heavy metal (lithium, mercury) intoxication [9]. Complication rates tend to increase with an extended duration of impaction [3] In the literature, the reported duration of the impaction has been mostly in the range of hours to 4 weeks [4]. To our knowledge, there have not been cases reported with such suspected long duration of 1 year of impaction of a button battery in the oesophagus. Factors such as location, duration of exposure, remaining voltage, and chemical composition all determine the clinical course or eventual complication [8]. Initially it was recommended that batteries should be removed as early as possible upon diagnosis, as perforation can occur as early as within 5 hours [4, 10]. However, now it has been found that to attain an injury-free removal of an esophageal battery it should be done in less than 2 hours [7].
Endoscopic removal has been found to have the highest success rate compared to other modalities such as foley catheter extraction, esophageal bougienage, and extraction with McGill forceps and magnet catheters [5]. Emergency esophagoscopy either flexible or rigid can be done. The efficacy of either approach has been found to be equal in the removal of oesophageal FB [11, 12]. Surgical intervention is warranted in cases of failure to retrieve the FB by endoscopic means. Depending on the location of the FB, cervicectomy, thoracotomy, or gastrotomy might be done. Oesophageal stricture or stenosis may result after ingestion and subsequent removal modality. Hence there is a need to put a post-removal follow-up plan for the individual patient, some patients may end up requiring a series of oesophageal dilatation after the ordeal.
Conclusion
Complications of FB ingestion in the paediatric population can come with serious complications. High morbidity and mortality may be attributed to delayed diagnosis and intervention. Clinicians are emphasized to have a high index of suspicion for possible FB ingestion or aspiration in children who present with upper aerodigestive tract symptoms.
Abbreviations
CT scan - Computer Tomography
FB - Foreign Body
OGD - Esophagogastroduodenoscopy
NGT- Nasogastric feeding Tube
Declarations
Declaration of competing interest
The authors declare no conflict of interest.
Funding
No financial support for the research, authorship, and/or publication of this article was received for this article.
Ethical approval
Institutional Ethical approval not required for reporting individual cases and or case series.
Consent
Written informed consent was obtained from the patient's parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Credit authorship contribution statement
Kenneth Mlay and Peter Ernest Kipiki: conceptualized and wrote the first draft of the manuscript: Adnan Sadiq and Bernard Minja collected and summarized patients’ data. Desiderius Chussi and Philibert Mtenga: Revised and wrote the final version of the manuscript. All authors read and accepted the final version for submission
Acknowledgements
The authors would like to thank the patient for allowing us to use his medical information for academic purposes.
References
- Rybojad B, Niedzielski A, Niedzielska G, Rybojad P. (2012). Risk factors for otolaryngological foreign bodies in eastern poland. Otolaryngol Head Neck Surg. 147(5):889-893.
Publisher | Google Scholor - Cheng W, Tam PKH. (1999). Foreign-body ingestion in children: Experience with 1,265 cases. J Pediatr Surg. 34(10):1472-1476.
Publisher | Google Scholor - Sink JR, Kitsko DJ, Mehta DK, Georg MW, Simons JP. (2016). Diagnosis of pediatric foreign body ingestion: Clinical presentation, physical examination, and radiologic findings. Ann Otol Rhinol Laryngol. 125(4):342-350.
Publisher | Google Scholor - Yardeni D, Yardeni H, Coran AG, Golladay ES. (2004). Severe esophageal damage due to button battery ingestion: Can it be prevented? Pediatr Surg Int. 20(7):496-501.
Publisher | Google Scholor - Jayachandra S, Eslick GD. (2013). A systematic review of paediatric foreign body ingestion: Presentation, complications, and management. Int J Pediatr Otorhinolaryngol. Elsevier Ireland Ltd, 77(3):311-317.
Publisher | Google Scholor - Alam E, Mourad M, Akel S, Hadi U. (2015). A Case of Battery Ingestion in a Pediatric Patient: What Is Its Importance? Case Rep Pediatr. Hindawi Publishing Corporation, 1-3.
Publisher | Google Scholor - Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. (2010). Emerging battery-ingestion hazard: Clinical implications. Pediatrics, 125(6):1168-1177.
Publisher | Google Scholor - Lin VYW, Daniel SJ, Papsin BC. (2004). Button batteries in the ear, nose and upper aerodigestive tract. Int J Pediatr Otorhinolaryngol. 68(4):473-479.
Publisher | Google Scholor - Marom T, Goldfarb A, Russo E, Roth Y. (2010). Battery ingestion in children. Int J Pediatr Otorhinolaryngol. Elsevier Ireland Ltd, 74(8):849-854.
Publisher | Google Scholor - Chiang MC, Chen YS. (2000). Tracheoesophageal fistula secondary to disc battery ingestion. Am J Otolaryngol - Head Neck Med Surg. 21(5):333-336.
Publisher | Google Scholor - Kimball SJ, Park AH, Rollins MD, Grimmer JF, Muntz H. (2010). A review of esophageal disc battery ingestions and a protocol for management. Arch Otolaryngol Head Neck Surg, 136(9):866-871.
Publisher | Google Scholor - Popel J, El-Hakim H, El-Matary W. (2011). Esophageal foreign body extraction in children: Flexible versus rigid endoscopy. Surg Endosc. 25(3):919-922.
Publisher | Google Scholor