Case Report
Brain Glioma Surgery by Craniotomy with The Patient Awake, Report of 2 Cases: Surgical and Anesthetic Considerations
- Doriam Perera Valdivia 1
- Jose Talavera Carrasco 2
- Luis Zapata Vega 1
- Edgar Herrera Perez 1
- Mauricio Augusto Matus 1
- Jose Miguel Hurtado 1
- Lagree Guzman Reynoso 1
- Luis Oporta Campos 2*
1Neurosurgery Service, Military Teaching Hospital Dr Alejandro Dávila Bolaños, Hospital in Managua, Nicaragua.
2Department of Anesthesiology, Military Teaching School Dr Alejandro Dávila Bolaños, Managua, Nicaragua.
*Corresponding Author: Luis Oporta Campos, Department of Anesthesiology, Military Teaching School Dr Alejandro Dávila Bolaños, Managua, Nicaragua.
Citation: Valdivia D. P, Carrasco J. T, Vega L. Z, Pérez E. H, Reynoso L. G, et al. (2024). Brain Glioma Surgery by Craniotomy with The Patient Awake, Report of 2 Cases: Surgical and Anesthetic Considerations, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 1(2):1-7. DOI: 10.59657/2997-6103.brs.24.004
Copyright: © 2024 Luis Oporta Campos, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 26, 2024 | Accepted: May 08, 2024 | Published: May 17, 2024
Abstract
Background: We describe two adult patients, who underwent surgery for brain gliomas near motor control brain areas, using the technique of awake craniotomy plus electrophysiological stimulation.
Description of the cases: Using the technique of awake craniotomy plus electrophysiological stimulation, two patients with brain tumors (glioma type) located in the right frontal lobe were operated on, both of which, due to the large size of the lesions, were in close contact with multiple motor brain structures. In both patients a surgical tumor resection of more than 90 % was achieved without any complication.
Conclusions: The technique of craniotomy with the patient awake and electrophysiological stimulation was very safe and effective in these two patients to resect brain gliomas close to eloquent motor areas.
Keywords: craniotomy; awake surgery; gliomas; monitoring; neuroanesthesiology
Introduction
Surgery for brain tumors that are close to or within highly functional (eloquent) brain structures - such as: motor (both cortical and projection or associative), somatosensory, language, cognitive and deep brain nuclei - may occur in 10-15% of patients [1]. Tumors in these locations represent a challenge for neurosurgeons and usually to avoid neurological complications, less radical tumor resection surgeries have been preferred, which on the other hand decreases patient survival due to residual tumor progression [2]. Awake craniotomy (AC) is a safe and well-established neurosurgical technique that provides maximum resection of lesions in eloquent brain areas while preserving optimal neurological functions by allowing real-time patient monitoring during tumor resection guided with cortical and subcortical electrical stimulation (electrophysiological brain mapping) [3,4,17]. Awake brain tumor resection poses a unique challenge for the neuroanesthesiologist, and the success of the procedure depends largely on careful patient selection and the expertise of the surgical and neuroanesthesia team. Awake-patient neurosurgery, also called "awake-patient craniotomy," is a type of procedure that is performed on the brain while you are awake and conscious [5]. Here we present two cases of gliomas where motor and premotor areas are affected, at frontal level with involvement of the corpus callosum in both patients and therefore the risk of causing a lesion to the motor area is high, which usually also limits us to perform a wide tumor resection. The aim of this article is to describe the two clinical surgical cases with their results and to describe the anesthetic technique.
Material and Methods
In this case report we reviewed the perioperative records of patients scheduled for surgery with the use of the anesthetic technique with the awake patient in our institution, in the first semester of the year 2023. The main perioperative aspects to perform the procedure were investigated such as: surgical indication, craniotomy technique used, assessments, eligibility criteria and the main complications presented intraoperatively and postoperatively. The data were tabulated in a spreadsheet (Microsoft® Office Excel, Microsoft Corporation). The analysis is oriented to the description of the approach, different clinical data of the operated patients are reflected in tables and the pre and postoperative images of each case are attached.
Case 1
A 23-year-old male patient with a history of epilepsy of 6 months of evolution. Physical examination and laboratory tests were normal (Table 1). A brain MRI showed a tumor lesion compatible with a low-grade astrocytoma.
We first performed neuro navigation-guided biopsy surgery in which we confirmed that the tumor was a grade 2 diffuse astrocytoma.
Table 1: Clinical characteristics of patients undergoing awake surgery at the EADB Military Hospital.
| No | Total length of surgery (plus initial anesthesia time) | Awake time during surgery | Clinical data | Electrophysiological monitoring | Postoperative deficit | Percentage of tumor resection |
| 1 | 300 minutes | 210 minutes | Focal and generalized epilepsy | Yes | No | 91% |
| Karnofsky = 100 | ||||||
| 2 | 380 minutes | 230 minutes | Focal and generalized epilepsy | Yes | No (Improvement of Muscular strength 5/5) | 94% |
| Karnofsky = 100 | ||||||
| Headache 4/10(END) | ||||||
| Hemiparesis left 4/5 |
Source: Clinical Record.
In the planning of the tumor resection surgery, due to the proximity of the tumor to the right frontal premotor and motor area and corpus callosum, we decided together with the support of our neuroanesthesiologist to perform craniotomy surgery plus brain tumor resection with the patient awake. The patient's cognitive status was normal (Addenbrookes = 96 /100 points) (Table 2). The advantages and disadvantages of awake surgery were explained to the patient, and the patient accepted and cooperated with the whole process.
Table 2: Cognitive evaluation of patients undergoing awake surgery at the EADB Military Hospital.
| No. | MoCAPre. | MoCAPost | Addenbrookes Pre-surgical | Post-surgical Adden Brookes |
| 1 | 27 | 28 | 96 | 96 |
| 2 | 26 | 26 | 90 | 96 |
First to perform the craniotomy began with the patient asleep, anesthetic depth monitoring with continuous EEG and BIS, starting anesthetic induction with Fentanyl 400 mcg, Atracurium 50 mg and Propofol 60 mg, classic laryngeal mask was placed and dual mechanical ventilation (pressure control + volume guaranteed), scalp block (SCALP) was performed with bupivacaine 0.5% bupivacaine and 2% lidocaine, followed by infusion of Dexmedetomidine at a dose of 0.3/mcg/kg/hr and fentanyl at 39 ng/kg/min and Propofol 90mcg/kg/min. The craniotomy was performed in the conventional way marking the limits of the craniotomy with the help of the neuro navigator (Medtronic S8) and after opening the dura mater (in which nothing was infiltrated) the neuroanesthesiology team proceeded to awaken the patient, having plasma concentration rate of Propofol of 2.7 mcg/mL and fentanyl 3.1 ng/mL, the infusions of Propofol and fentanyl were omitted for 15 minutes and BIS was monitored, waking up the patient with BIS of 88, removing the laryngeal mask, the patient was conscious, oriented, calm, maintaining infusion of Dexmedetomidine 0.2 mcg/kg/hr., administering oxygen through nasal prongs and performing early neurological evaluation to start lesion resection. The tumor resection surgery was performed without any eventuality.
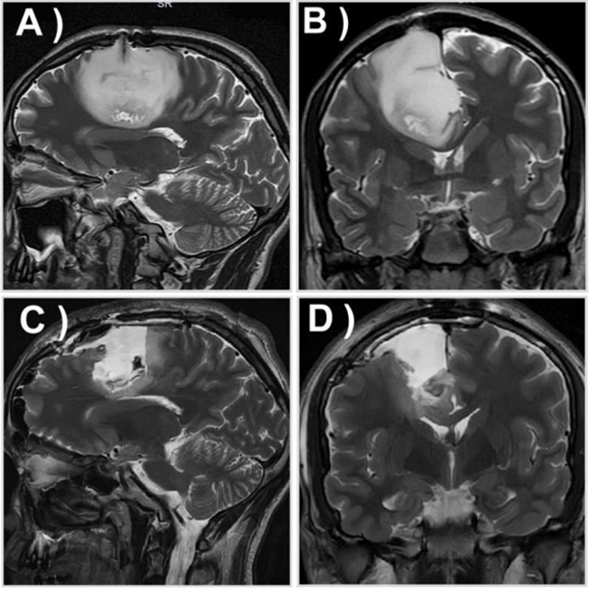
Figure 1: Brain magnetic resonance images of case 1. A) and B) are pre-surgical resonance images in sagittal and coronal T2 sequence respectively, C) and D) are post-surgical resonance images in sagittal and coronal T2 sequence respectively.
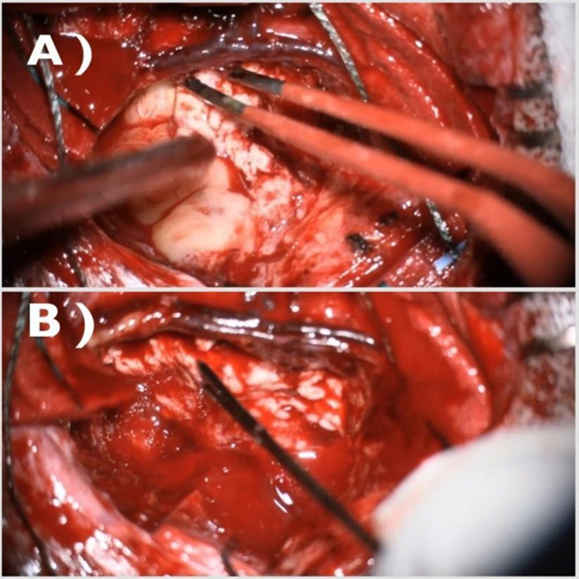
Again with the help of the neuro navigator and now also aided with bipolar electrophysiological stimulation (NIM - Eclipse Medtronic System, with motor mapping and language mapping protocol) performing neurological tests to evaluate motor and cognitive function (tests of judgment, abstraction, calculation, language, memory, and integrity of the motor areas, evaluating the latter through movements and exercises such as "holding objects"), The cortical limits of the tumor were established, as well as the safe areas (negative areas) by marking the eloquent area with cotonoids. The tumor lesion was resected, then the patient was put to sleep and closed in planes (Figure 2).
Figure 2: Images during surgical resection of the tumor. A) Surgical resection of the tumor, B) Electrophysiological stimulation of surgical resection edges to confirm proximity of neurological motor structures.
In the postoperative MRI (on the 3rd postoperative day) a subtotal resection of the tumor of approximately 91% was verified (in T2 sequence, which is a low-grade glioma) (Figure 1). There were no postoperative complications and the patient was discharged on the fourth postoperative day.
Case 2
A 42-year-old male patient with a history of suffering from epilepsy for 5 years and having been diagnosed 4 years ago with a grade II diffuse astrocytoma, but on that occasion the patient did not want to undergo surgery.
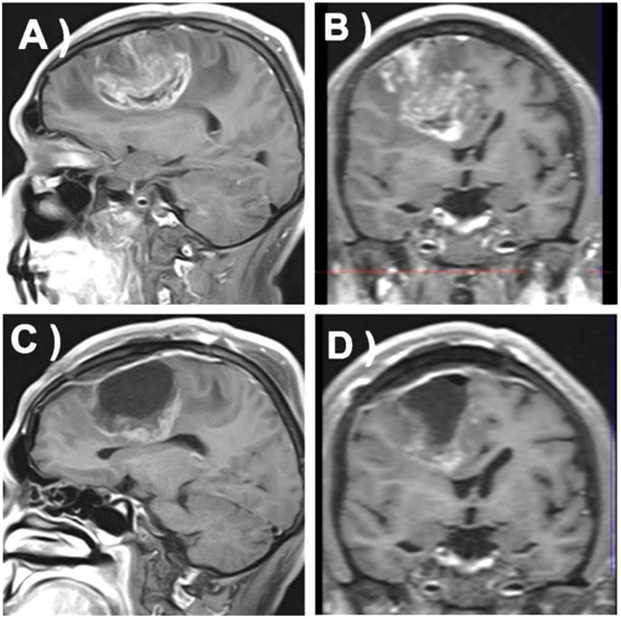
Three months prior to his last admission the patient began to present mild left hemiparesis (Daniels Scale = 4/5) and increased frequency of focal epileptic seizures in the left upper limb. A brain MRI was performed which revealed growth and most probably tumor progression to a high-grade glioma (Figure 3).
Figure 3: Brain magnetic resonance images of case 2. A) and B) are pre-surgical sagittal and coronal contrasted T1- weighted sagittal and coronal contrasted T1-weighted sagittal and coronal contrasted T1-weighted images respectively, C) and D) are post-surgical sagittal and coronal contrasted T1-weighted images respectively.
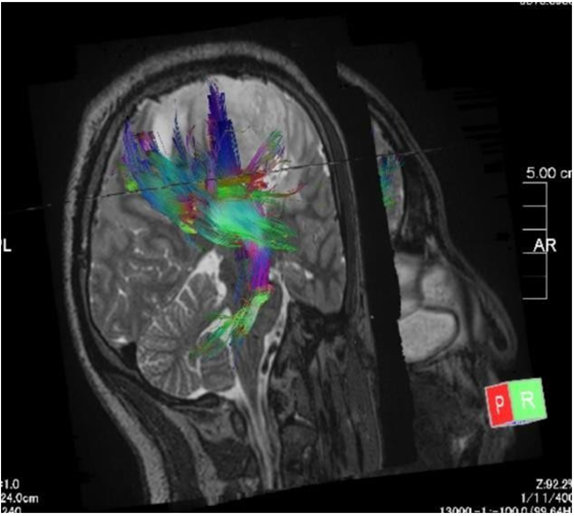
The patient was scheduled for tumor resection surgery but due to the proximity of the tumor to cortical motor and premotor areas, corpus callosum and corona radiata fibers (Figure 4), it was decided in conjunction with neuroanesthesiology to perform the surgery with the patient awake (Figure 5).
Figure 4: Pre-surgical tractography images of case 2.
Figure 5: Brain glioma resection surgery with the patient awake. While applying bipolar cortical brain stimulation, the patient's motor response is assessed: the patient is asked to move his fingers and hand.
The patient's post-surgical course was adequate, presenting normalization of motor strength and slight improvement of cognitive status. The post-surgical MRI showed a subtotal resection of approximately 94% (assessed in contrasted T1 sequence when it was later proved that it was indeed a high-grade glioma). Histopathology revealed a grade 3 anaplastic astrocytoma. The surgery was performed following the same steps as in case 1, with anesthetic management very similar to the previous case. In this opportunity, the procedure was stopped in the final stages of the resection of the inferoposterior part of the tumor because the patient presented focal seizure of the left upper limb of 30 to 40 seconds duration, secondary to the subcortical stimulation, which ceased when irrigating with cold saline solution in the area of subcortical stimulation and additionally 50 mg of Propofol were administered, with which the seizures ceased.
Discussion
In these two very similar cases in terms of size and anatomical location of the brain tumors, where in both cases there was proximity of the tumor to cortical and subcortical motor and premotor areas, in which we considered that the risk of neurological injury was high, we considered that craniotomy surgery with the patient awake allowed us to resect as much of the tumor as possible without causing any damage to the patients. Both patients met the requirements to be operated with the awake craniotomy technique: age over 18 years and under 60, favorable Karnofsky index, adequate survival from initial diagnosis, no obesity, no obstructive sleep apnea, hydro electrolytic, coagulation or infectious disorders were ruled out, patients without cognitive deficit, the presence of claustrophobia and other diseases were ruled out through psychological assessment and that the patients agreed and understood the procedure, because the vigil stage in the patient is crucial to successfully perform such procedure. This facilitated the surgical team's approach at the time of performing the procedures [6,7,14,15].
Currently the most appropriate technique that guarantees the best results, both oncological and neurological, is to couple awake craniotomy with cortical and subcortical electrophysiological stimulation (brain mapping), since the use of brain mapping further reduces the possibility of causing neurological damage (40-50% less risk) and further increases the degree of tumor resection [8,9,16]. In both cases tumor resection greater than 90 % was achieved, and the eloquent areas were preserved and none of the patients presented any post-surgical complication or neurological deficits. Our results coincide with the international literature where the mean tumor resection extension is 90%, with the use of awake surgery plus electrophysiological stimulation. While with general anesthesia the mean extent of tumor resection is 81.7% [8]. Given the limited life expectancy, particularly of high-grade gliomas, postoperative quality of life is as important as the actual length of survival. None of the patients presented any complication or neurological deterioration. The first patient after resection did not present any deficit and the second one, improvement in muscle strength was observed increasing to 5/5, from the clinical point of view, 24 hours after the surgical procedure. In this aspect with respect to the international literature, transient neurological deterioration has been described in 15-30% of patients and permanent neurological complications have been described in 5.4% of patients operated by awake craniotomy and electrophysiological stimulation [9-13].
Conclusion
The technique of craniotomy with the patient awakes and electrophysiological stimulation was very safe and effective in these two patients to resect gliomas in eloquent motor areas.
Conflict of Interest
None reported by the authors.
References
- Dreier JD, Williams B, Mangar D, Camporesi EM. (2019). Patients Selection for Awake Neurosurgery. HSR Proc Intensive Care Cardiovasc Anesth. 1(4):19-27.
Publisher | Google Scholor - J. Chui. (2015). Anesthesia For Craniotomy in The Awake Patient: An Update. Rev colomb anesthesiol. 43(S1):22-28.
Publisher | Google Scholor - Velázquez González K BSDVER. (2021). Craniotomy In the Awake Patient. Cuban Journal of Anesthesiology and Resuscitation. 20(1): P. 644.
Publisher | Google Scholor - Ibrahim GM, Bernstein M. (2012). Awake Craniotomy for Supratentorial Gliomas: Why, When and How? Future Medicine, Toronto Western Hospital, University of Toronto. 1(1): P. 71-83.
Publisher | Google Scholor - Lacroix M, Abi-Said D, Fourney DR, et al. (2001). A Multivariate Analysis Of 416 Patients with Glioblastoma Multiforme: Prognosis, Extent of Resection, And Survival. J Neurosurg. 95(2):190-198.
Publisher | Google Scholor - Zhang Kaiying, Gelb Adrian W. (2018). Awake Craniotomy: Indications, Benefits, And Techniques. Colombian Rev. Anesthesiol, 46(Suppl 1): 46-51.
Publisher | Google Scholor - Gogos AJ, Young JS, Morshed RA, Hervey-Jumper SL, Berger MS. (2020). Awake Glioma Surgery: Technical Evolution and Nuances. J Neurooncol. 147(3):515-524.
Publisher | Google Scholor - Suarez-Meade P, Marenco-Hillembrand L, Prevatt C, Murguia-Fuentes R, Mohamed A, et al. (2020). Asleep Motor Mapping for Glioma Resection: A Systematic Review and Meta-Analysis. Acta Neurochir. 162(7):1709-1720.
Publisher | Google Scholor - Bu LH, Zhang J, Lu JF, Wu JS. (2021). Glioma Surgery with Awake Language Mapping Versus Generalized Anesthesia: A Systematic Review. Neurosurg Rev. 44(4):19972011.
Publisher | Google Scholor - Demitre Serletis MD, AMB. (2007). Prospective Study of Awake Craniotomy Used Routinely and Non selectively for Supratentorial Tumors. Division Of Neurosurgery, Toronto Western Hospital, Toronto, Ontario, Canada. 107:1-6.
Publisher | Google Scholor - Erez Nossek MIM. (2013). Intraoperative Seizures During Awake Craniotomy: Incidence and Consequences: Analysis Of 477 Patients. Research-Human-Clinical Studies. 73(1).
Publisher | Google Scholor - Philip C. Dewitt Hamer SGRAH. (2012). Impact Of Intraoperative Stimulation Brain Mapping on Glioma Surgery Outcome: A Meta-Analysis. Journal of Clinical Oncology. 30(20).
Publisher | Google Scholor - Hervey-Jumper SL, Li J, Lau D, Molinaro AM, Perry DW, et al. (2015). Awake Craniotomy to Maximize Glioma Resection: Methods and Technical Nuances Over A 27year Period. J Neurosurg. 23(2):325-339.
Publisher | Google Scholor - T B, H A, B A. (2013). Awake Craniotomy for Brain Tumor Resection: The Rule Rather Than the Exception? 25(3).
Publisher | Google Scholor - Dziedzic T, Bernstein M. (2014). Awake Craniotomy for Brain Tumor: Indications, Technique and Benefits. Medical University of Warsaw Neurosurgery. 14:1405-1415.
Publisher | Google Scholor - Ottenhausen M, Krieg SM, Meyer B, Ringel F. (2015). Functional Preoperative and Intraoperative Mapping and Monitoring: Increasing Safety and Efficacy in Glioma Surgery. Neurosurg Focus. 38(1):E3.
Publisher | Google Scholor - Mofatteh M, Mashayekhi MS, Arfaie S, Chen Y, Hendi K, et al. (2023). Stress, Anxiety, And Depression Associated with Awake Craniotomy: A Systematic Review. Neurosurgery. 92(2):225-240.
Publisher | Google Scholor