Case report
Bladder Paraganglioma: Report of Two Cases and A Literature Review
- Amine Slaoui 1*
- Babty Mouftah 1
- Aziz Slaoui 2*
- Yassir Himmi 1
- Amine El Affari 1
- Omar Zineddine 1
- Taha Yassine Abboudech 3
- Zakia Bernoussi 3
- Tarik Karmouni 1
- Khalid El Khader 1
- Aziz Baydada 2
- Aicha Kharbach 2
- Abdellatif Koutani 1
- Ahmen Ibn Attya Andaloussi 1
1Department of Urology B, Avicenne Hospital, University Hospital Center IBN SINA, University Mohammed V, Morocco.
2Department of Gynaecology-Obstetrics, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
3Department of Anatomy and Pathological Cytology, University Hospital Center IBN SINA, University Mohammed V, Morocco.
*Corresponding Author: Aziz Slaoui, Department of Gynaecology-Obstetrics, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
Citation: A Slaoui, B Mouftah, A Slaoui, Y Himmi, Amine E Affari. (2022). Bladder Paraganglioma: Report of Two Cases and A Literature Review. International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(1); DOI: 10.59657/2837-8172.brs.23.004
Copyright: © 2022 Aziz Slaoui, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 17, 2022 | Accepted: December 09, 2022 | Published: January 12, 2023
Abstract
Objective: We report two incidental cases of bladder paraganglioma and a review of the literature published to date.
Methods: Medline was searched for the last 10 years for the terms "paraganglioma" and "urinary" and "bladder".
Results: Bladder paraganglioma (BP) is extremely rare. It represents 10% of all paragangliomas and concerns less than 0.06% of bladder tumors. Often discovered by chance, it can nevertheless be symptomatic, particularly during micturition. The most common symptoms are hematuria, hypertension and headache. About 14% of these tumors are malignant and radio-chemically resistant. Surgery is therefore the cornerstone of treatment. We recommend, cystoscopy, partial cystectomy and regular follow-up based on regular cystoscopy and imaging.
Their rarity explains why, at present, there are no recommendations for treatment and monitoring. However, their risk of malignancy recurrence and metastasis requires regular and long-term follow-up.
Conclusions: Bladder paragangliomas are rare tumors. Treatment should be based on partial cystectomy and their follow-up should be regular.
Keywords: paraganglioma; bladder; treatment; follow-up
Introduction
Bladder paraganglioma (BP) is extremely rare. It represents 10% of all paragangliomas and concerns less than 0.06% of bladder tumors [1]. Often discovered by chance, it can nevertheless be symptomatic, particularly during micturition. The most common symptoms are hematuria, hypertension, headache and micturition syncope [2].
Through the observation of clinical cases that we have treated in the department of urology B, we will review the literature to determine the appropriate management and follow-up of this rare pathology.
Patient and Observation
Case No. 1
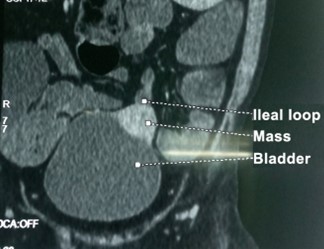
A 37-year-old patient with a history of chronic smoking, thalassemia, who consulted for primary infertility with oligospermia. The radiological workup revealed a bladder mass measuring 47x27 mm in the anterior wall of the bladder, lateralized to the left, with extra-vesical development, which was strongly enhanced by the injection of contrast (Figure 1). Cystoscopy found a healthy-looking bladder mucosa with a mass effect on the anterior wall (Figure 2). The multidisciplinary consultation meeting recommended a partial cystectomy. During the partial cystectomy the blood pressure increased sharply as soon as the mass was compressed. We have suspected the possibility of a paraganglioma confirmed by the pathological examination of the surgical specimen. Postoperative I-123-metaiodobenzylguanidine scintigraphy did not detect any other localization. After 1 year of follow-up with cystoscopy, CT and methoxylated derivatives in 24-hour urine, no recurrence was found.
Figure 1: CT scan showing bladder lesion.
Figure 2: Postoperative photography of the specimen.
Case No. 2
A 23-year-old female patient with a history of three miscarriages, who reported episodes of painless hematuria and micturition syncope. Clinical examination revealed a blood pressure of 17/11mmHg. Urinary normetanephrines are 69mmol/24h and urinary metanephrines are 1.26mmol/24h. Contrast-enhanced CT scan revealed a strongly contrast-enhanced bladder mass. No lymph nodes or peripheral lesions were detected.
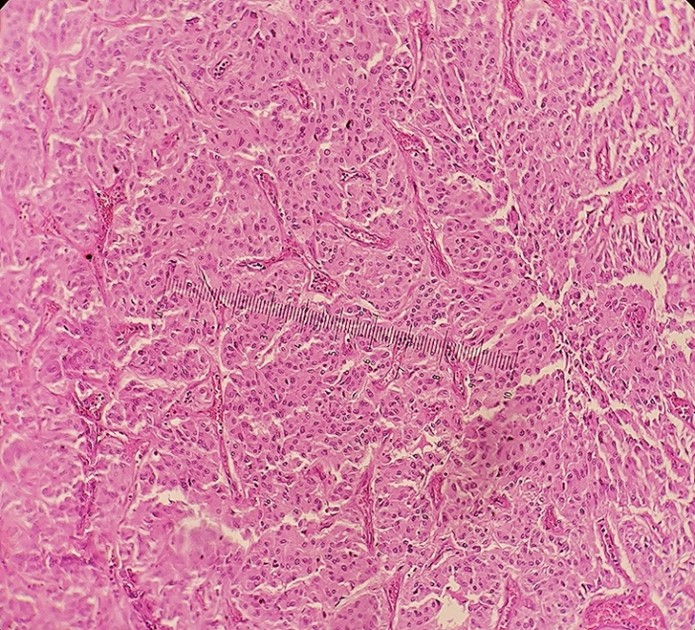
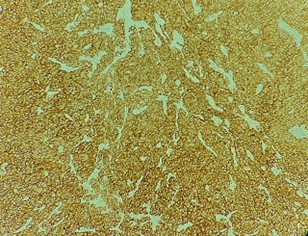
She underwent laparoscopic partial cystectomy. Histological examination of the specimen showed the presence of a paraganglioma (Figure 3-5). One month after the operation, the plasma concentrations of metanephrines (MP) and vanillylmandelic acid (VMA) in the urine were normal. Histological examination showed GMP. After 4 years of follow-up with cystoscopy, CT and methoxylated derivatives in 24-hour urine, no recurrence was found.
Figure 3: Histological study revealing zellballen nests of epithelioid cells with abundant eosinophilic cytoplasm and a vascular stroma.
Figure 4: Immunohistochemical study: positive cytoplasmic granular labelling by anti-synaptophysin.
Discussion
Pheochromocytomas are tumors of the adrenal medulla and sympathetic nervous system. They secrete catecholamines (norepinephrine, epinephrine, and dopamine).
Extra-adrenal pheochromocytomas, called paragangliomas, account for about 10% of all pheochromocytomas [3]. Bladder paraganglioma is a non-urethral tumor of the bladder. In 1953 Zimmerman described it for the first time [4].
Das et al. reported that the classic triad of vesical paraganglioma includes macroscopic hematuria, hypertension and hypertensive crisis on voiding [5]. eIn 234 Japanese cases examined by Yamamoto et al. 41.3% had macroscopic hematuria, 33.2% had hypertension and 23.0% had hypertensive crisis on voiding. Only 1.4% had all three symptoms, while 10.6% had none of these symptoms [6]. The related symptoms are most often at micturition or excessive bladder distension leading to catecholamine release.
The preoperative diagnosis is usually suspected on questioning, which should be thorough to look for the typical clinical signs mentioned and the triggering factors. CT and MRI are both useful to localize the primary tumor and sometimes possible metastases. However, metaiodinebenzylguinidine (MIBG) iodine scintigraphy has a very high sensitivity and specificity for the detection of pheochromocytomas [7].
The biology finds high methoxylated derivatives. They must be measured on the 24-hour urine or a plasma assay in case of renal insufficiency.
Their rarity explains why, at present, there are no recommendations for treatment and monitoring. Thus, complete surgical resection of the tumor remains the gold standard in the management of bladder paragangliomas: partial cystectomy or cystectomy. Transurethral resection of the bladder may be incomplete and may result in morbid hypertensive peaks. The literature does not find any interest in radiotherapy and chemotherapy because they have shown limited efficacy [8].
Histologically, the tumor is composed of "zellballen" nests of epithelioid cells with abundant eosinophilic cytoplasm and a vascular stroma. The immunohistochemical study shows positive cytoplasmic granular labeling by anti-synaptophysin and anti-chromogranin A [9]. According to Pattarino et al, metastatic dissemination is the only true evidence of malignancy. The other characteristics are according to the literature unreliable to distinguish formally and definitively benign from malignant tumors [10].
Syncopal micturition is pathognomonic for the release of catecholamines induced by urination. Pre-, per- and postoperative preparation can drastically reduce perioperative mortality and morbidity.
Thus, preoperatively, the patient requires α-adrenergic blockade and volume expansion. During surgery the risk of hypertensive crisis must be controlled by an α-blocker. Finally, postoperatively, close monitoring of blood glucose and blood pressure is recommended [11].
There is no consensus on the follow-up of patients with paraganglioma. Most authors agree on the importance of clinical and biological follow-up of patients throughout their lives. Indeed, the dissemination or local recurrence of malignant paragangliomas can occur very late in the clinical course. Lenders JWM et al. suggest annual cystoscopy, plasma or urine catecholamine analysis and MIBG scintigraphy [12]. On the other hand, Young et al. consider the annual determination of vanyl mandelic acid as the best tool to detect clinical recurrence or distant metastases [13].
Conclusion
Bladder paraganglioma (BP) is extremely rare. Often discovered by chance, it can nevertheless be symptomatic, particularly during micturition. These tumors are malignant and radio-chemically resistant. Surgery is therefore the cornerstone of treatment. Their rarity explains why, at present, there are no recommendations for treatment and monitoring. We recommend, cystoscopy, partial cystectomy and regular follow-up based on regular cystoscopy and imaging.
Abbreviations
BP: Bladder paraganglioma
MRI: Magnetic Resonance Imaging
Declarations
Conflicts of interest
The authors declare that they have no competing interests.
Sources of funding
There are no funding sources to be declared.
Ethical approval
Ethics approval has been obtained to proceed with the current study.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author contribution
AS: study concept and design, data collection, data analysis and interpretation, writing the paper. BM: study concept and design, data collection, data analysis and interpretation, writing the paper. AS: study concept, data collection, data analysis, writing the paper. YH: study concept, data collection, data analysis, writing the paper. AEA: study design, data collection, data interpretation, writing the paper. OZ: study design, data collection, data interpretation, writing the paper. TYA: study design, data collection, data interpretation, writing the paper. ZB: study concept, data collection, data analysis, writing the paper. TK: study concept, data collection, data analysis, writing the paper. KEK: study concept, data collection, data analysis, writing the paper. AB: study concept and design, data collection, data analysis and interpretation, writing the paper. AK: study concept and design, data collection, data analysis and interpretation, writing the paper. AK: study concept and design, data collection, data analysis and interpretation, writing the paper. AIAA: study concept and design, data collection, data analysis and interpretation, writing the paper.
Guarantor of Submission
The corresponding author is the guarantor of submission.
Acknowledgements: None.
Availability of data and materials
Supporting material is available if further analysis is needed.
Provenance and peer review Not commissioned, externally peer-reviewed.
References
- Matsuzawa N, Nishikawa T, Ohno R, Inoue M, Nishimura Y, Okamoto T, Shimizu T, Shinagawa T, Nishizawa Y, Kazama S. (2022). Paraganglioma of the urinary bladder initially diagnosed as gastrointestinal stromal tumor requiring combined resection of the rectum: a case report. World J Surg Oncol, 20(1):185.
Publisher | Google Scholor - Sunil V N, John K, Nawahirsha S, Iyyadurai R. (2020). Micturition syncope: a rare presentation of bladder paraganglioma. BMJ Case Rep, 13(9):e235353.
Publisher | Google Scholor - Pelegrín-Mateo Francisco j, Fernández-Cruz Marian, Seguí-Moya Elena, García-Seguí Alejandro, Ernesto de Nova-Sánchez, Sánchez-Heras Ana Beatriz. (2021). Paraganglioma vesical reporte de dos casos clínicos y revisión de la literatura. Archivos españoles de urología, 74(4):445-449.
Publisher | Google Scholor - Zimmerman I.L, Biron R.E, Mcmahon M.E. (1953). Pheochromocytoma of the urinary bladder. N. Engl. J. Med, 249:25-26.
Publisher | Google Scholor - Das S, Bulusu NV, Lowe P. (1983). Primary vesical pheochromocytoma. Urology, 21(1):20-25.
Publisher | Google Scholor - Yamamamoto, Y. (2013). Shigeaki nakazawa: paraganglioma of the urinary bladder managed by transurethral resection: a case report. Jpn J Urol Surg, 26(2):231-234.
Publisher | Google Scholor - Aygun N, Uludag M. (2020). Pheochromocytoma and paraganglioma: from clinical findings to diagnosis. Sisli Etfal Hastan Tip Bul, 54:271-280.
Publisher | Google Scholor - Tu X, Zhang N, Zhuang X, Chen S, Luo X. (2021). Incidental diagnosis of nonfunctional bladder paraganglioma: a case report and literature review. BMC Urol, 21(1):98.
Publisher | Google Scholor - Sunil V N, John K, Nawahirsha S, Iyyadurai R. (2020). Micturition syncope: a rare presentation of bladder paraganglioma. BMJ Case Rep, 13(9):e235353.
Publisher | Google Scholor - Quist EE, Javadzadeh BM, Johannesen E, Johansson SL, Lele SM, Kozel JA. (2015). Malignant paraganglioma of the bladder: a case report and review of the literature. Pathol Res Pract, 211:183-188.
Publisher | Google Scholor - Tu X, Zhang N, Zhuang X, Chen S, Luo X. (2021). Incidental diagnosis of nonfunctional bladder paraganglioma: a case report and literature review. BMC Urol, 21(1):98.
Publisher | Google Scholor - Lenders JWM, Eisenhofer G. (2017). Update on modern management of pheochromocytoma and paraganglioma. Endocrinol Metab (Seoul), 32:152-161.
Publisher | Google Scholor - William Young. (2006). Paragangliomas: clinical overview. Ann N Y Acad Sci, 1073:21-29.
Publisher | Google Scholor