Research Article
Birth Preparedness and Obstetric Danger Signs: Perception and Predictors among Expectant Mothers in Southwest Nigeria
- Adebukunola O Afolabi 1*
- Oluwadamilola Aladegbami 2
- Taiwo Dosunmu 3
- Kolade A Afolabi 4
- Adenike A Olaogun 1
1Department of Nursing Science, Obafemi Awolowo University, Ile-Ife, Osun state, Nigeria.
2Mother and Child Hospital, Akure, Ondo state, Nigeria.
3Department of Nursing Science, BOWEN University, Iwo, Osun state, Nigeria.
4Medical and Health Services, Obafemi Awolowo University, Ile-Ife, Osun state, Nigeria
*Corresponding Author: Adebukunola O. AFOLABI, Department of Nursing Science, Obafemi Awolowo University, Ile-Ife, Osun state, Nigeria.
Citation: Adebukunola O Afolabi, Aladegbami O, Dosunmu T, Kolade A Afolabi, Adenike A Olaogun. (2023). Birth Preparedness and Obstetric Danger Signs: Perception and Predictors among Expectant Mothers in Southwest Nigeria, Journal of Women Health Care and Gynecology, BioRes Scientia publishers. 2(3):1-12, DOI: 10.59657/2993-0871.brs.23.017
Copyright: © 2023 Adebukunola O Afolabi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 15, 2023 | Accepted: October 02, 2023 | Published: October 09, 2023
Abstract
Background: Planning for safe delivery and anticipating actions needed during obstetric emergencies are vital strategies towards reduction in maternal mortality and morbidity.
Objective: Study explored perception about danger signs of pregnancy among expectant mothers, assessed level of knowledge about danger signs of pregnancy, examined birth preparedness and related factors among expectant mothers in Ogbomosho, southwest Nigeria.
Study design: Study employed sequential explanatory mixed method design. Quantitative data was collected using questionnaire adapted from John Hopkins Program for International Education in Gynecology and Obstetrics, JHPIEGO (2004) from 483 expectant mothers, selected through multistage sampling technique. Binary logistic regression examined relationship between dependent and independent variables, p < 0.05 was significant. Focus Group discussion was conducted among 32 participants selected purposively, qualitative responses were analyzed thematically.
Results: Quantitative findings revealed that 34.8% of the mothers had good knowledge about danger signs of pregnancy, 65.2% had poor knowledge,36.9% had adequate preparation towards childbirth while 63.1% had inadequate preparations. Binary logistic regression analysis shows that good knowledge about danger signs of pregnancy (p=0.03, OR=0.54. CI=0.31-0.94) was the main predictor of birth preparedness among expectant mothers. Main themes from qualitative responses include knowledge about obstetric danger signs; recognition of obstetric danger signs; perceived severity of obstetric danger signs and perceived susceptibility to obstetric danger signs.
Conclusion: Good knowledge about obstetric danger signs was the main predictor of birth preparedness; effective maternal health services aiming at favorable pregnancy outcomes should focus on educating women on early identification of obstetric danger signs and prompt decision making capabilities.
Keywords: birth preparedness; obstetric danger signs; expectant mothers; nigeria
Introduction
Safe motherhood ensures that a woman is safe, remain healthy and receives the needed care during pregnancy, labour and puerperium [1]. Pregnancy is a period of expected physiological changes and can also be a period of severe vulnerability to the woman and the unborn child. Global estimate showed that 94% maternal deaths in 2017 reported during pregnancy and after childbirth occurred in low and middle income countries and significant proportion of these death could have been prevented [2]. The report further indicated that Sub-sahara Africa and south Asia accounted for an approximated 86% of the estimated global maternal deaths with sub-sahara Africa alone responsible for nearly two-third of these deaths. Studies have also showed that the risk of maternal death is highest among adolescents girls who are below 15 years old while pregnancy related complications are higher among adolescents girls aged 10-19 years compared to older women [2].
Nigeria is a leading African countries with the highest reported maternal Mortality rate of 814 per 100000 live births [3] whereas significant proportion of these maternal morbidity and mortality resulting from childbirth and related issues in developing countries could however be prevented if pregnant women recognize obstetric danger signs and seek prompt and appropriate obstetric interventions [4]. In order words, early recognition of danger signs of pregnancy and prompt care by skilled professionals before, during and after childbirth could save the lives of both the mother and the child [2]. Obstetric danger signs are indicators of severe unhealthy or harmful occurrences to the pregnant woman and or her fetus requiring urgent skilled intervention. The danger signs could be life threatening and could result into decline in maternal and neonatal health outcomes if not detected early. The common danger signs during pregnancy include vaginal bleeding, high fever, abdominal pain, severe headaches, blurred vision, convulsion, difficulty in breathing, swelling of hands and feet and absence or reduction of fetal movements [4]. The aim of effective antenatal care therefore is to anticipate, prevent and manage the three commonest causes of maternal mortality which include sepsis, hemorrhage and hypertensive disorders [5].
Broadly speaking, major causes of maternal deaths can be categorized as direct and indirect causes: the direct obstetric causes of maternal death are obstetric complications resulting from omissions in the course of treatments or interventions, inappropriate diagnosis and treatment while indirect obstetric causes of maternal death are those causes resulting from existing medical conditions that are developed during pregnancy and which were not due to obstetric causes but may have been aggravated by physiologic effects of pregnancy [4].
Birth preparedness and complication readiness involve planning for safe delivery and anticipating actions needed during obstetric emergencies [6]. This phenomenon is an essential aspect of safe delivery designed to solve various stages of delays in accessing prompt health care during emergencies by empowering women, familes and the community in general towards prompt informed decision making. The components of birth preparedness therefore include identification of a convenient place of delivery and skilled health care provider, making adequate financial preparation and savings, making preparation for important items needed for childbirth, securing a reliable means of transportation, making proper arrangement for blood donation, securing a mode of communication, designating a next of kin whenever necessary, adequate knowledge about obstetric danger sign and preparation to take action when necessary [7,8].
Birth preparedness and complication readiness remain vital strategy towards reduction in maternal mortality and morbidity. Additionally, women’s perception about danger signs of pregnancy has been linked to care seeking habits among expectant mothers worldwide [9]. Pregnant women’s ability to recognize danger signs during pregnancy, child birth and post-partum period are therefore essential towards prompt decision making and early medical care.
Birth preparedness can be measured by assessing mothers’ knowledge about identification of obstetric danger signs, and level of preparation towards childbirth [6]. A typical African setting believes dangers during pregnancy could result from witchcraft activities and ancestral displeasure (10). Such misconceptions result in consultations with traditionalists, local birth attendants; contributing to delay in seeking skilled medical care [11,12]. In addition, studies have further demonstrated that insufficient knowledge about obstetric danger signs among women, families and birth attendants in developing countries contribute to delay in seeking appropriate obstetric care which often result in high incidence of maternal and neonatal mortalities [9,13]. Adequate and appropriate knowledge about obstetric danger signs remain essential because it help in ensuring adequate birth preparedness for the woman and her spouse. Tamang et al. [14] similarly submitted that adequate knowledge about obstetric danger signs is the first essential step in accepting appropriate and timely referral while positive perception about obstetric danger signs by the pregnant woman will enhance her cognitive disposition towards pregnancy complications and reduce cultural and religious misconceptions typical of most African setting [15]. Perception and knowledge about obstetric danger signs has been linked to care seeking habits among expectant mothers [9]. There are however dearth of information regarding perception, knowledge about obstetric danger signs and objective evaluation of level of birth preparedness in this study area; hence this study which aimed at exploring perception about danger signs of pregnancy among expectant mothers, assessed level of knowledge about danger signs of pregnancy, examined birth preparedness and related factors among expectant mothers in Ogbomosho, Southwest Nigeria.
Method
Variables defined: Outcome variable is birth preparedness categorized as adequate or inadequate. Main independent variables include selected socio-demographic characteristics of expectant mothers. These are variables observed in previous studies to influence birth preparedness among mothers. Other independent variables include mothers’ knowledge about danger signs in pregnancy. An expectant mother is a woman whose pregnancy has been confirmed. Study design: Study employed sequential explanatory mixed method design using quantitative and qualitative data collection methods. The ‘Fixed Mixed Method design’ was employed in which quantitative and qualitative data collection methods were pre-determined and planned at the beginning of the research process. Quantitative data were collected first using structured interviewer-administered questionnaire from 483 expectant mothers, selected through multistage sampling technique. This was followed by qualitative data collection. Four sessions of Focus Group Discussion (FGD) were held for the qualitative study using a 12-item FGD guide, 8 discussants participated in each of 4 sessions of Focus Group Discussion giving a total of 32 participants. The FGD guide explored perception about danger signs in pregnancy and birth preparedness among the expectant mothers. Qualitative responses were used to validate quantitative findings.
Study setting
The study was conducted in selected health facilities in Ogbomosho town, Oyo state, an area between the savannah and rain forest belts of the south-western Nigeria. Ogbomosho is a metropolitan town founded in the mid-17th century and one of the major towns in southwest Nigeria with an estimated 245,000 inhabitants according to 2006 population census [16]. Ogbomosho has five Local Government Areas (LGAs) namely: Ogbomosho south, Ogbomosho north, Oriire, Surulere, and Ogo Oluwa Local Government Areas for ease of political administration and majority of the inhabitants are of the Yoruba ethnic group, which constitute one of the major ethnic groups in Nigeria. The inhabitants are traditional farmers while other forms of skilled professional carrier are also obtainable within the Ogbomosho metropolis. There are however other ethnic groups residing in the metropolitan city including Ibos, Hausas, Fulanis, Ijaws, Igbiras, Urhobos who are engaging in different forms of trading and commercial activities. The town has over ten health institutions which are either privately owned or are owned by the state government.
Study population
Study was conducted among expectant mothers attending routine ante natal clinics in selected health facilities within Ogbomosho metropolis. An expectant mother in this study is a pregnant woman, whose pregnancy has been duly confirmed.
Inclusion criteria
Expectant mothers whose pregnancies have been booked in the selected health facilities were included in this study.
Exclusion criteria
Expectant mothers who were critically ill, posing significant challenge to data collection were excluded from this study.
Sample size estimation for quantitative study
The Taro Yamane method for sample size estimation was used to estimate sample size for this study: Given n= N / 1+N (e)2, where n = estimated sample size, N = sample frame (estimated population under study), e = margin error (given as 0.05 in this study). With 10% attrition rate, an estimated 495 expectant mothers was recruited for this study.
Sampling technique for quantitative study
A total of 495 expectant mothers attending antenatal clinics in selected health facilities within Ogbomosho metropolis were selected through a multi-stage sampling technique: Stage one involved purposive selection of four health facilities namely: Bowen University Teaching Hospital, Ladoke Akintola Teaching Hospital, Ibrahim Taiwo Primary Healthcare centre and Adebayo Taiwo Primary Health care centre, all in Iwo, Oyo state, southwest Nigeria. These are health facilities within Ogbomosho metropolis with highest number of expectant mothers attending antenatal clinics observed during preliminary survey. In the second stage, the total estimated 495 expectant mothers were distributed proportionately among the four selected health facilities (sample proportionate to size). In stage three, eligible mothers in each health facilities were selected by convenience sampling technique. Selection of eligible mothers continued daily at the antenatal clinics in the selected health facilities until the sample size allotted to each facility was attained.
Sample size and sampling technique for qualitative study
Eight expectant mothers purposively selected participated in each of four sessions of the Focus Group Discussion giving a total of 32 participants. Two sessions of the FGD were held among mothers aged 20-29 years old and 40-49 years old respectively giving a total of 4 sessions (these are age groups observed to have higher risk of obstetric dangers in previous studies [17].
Research instruments
An adapted Johns Hopkins Program for International Education in Gynaecology and Obstetrics (JHPIEGO) Maternal and Neonatal Health Program Monitoring Tool (7) was used for quantitative data collection. The questionnaire was interviewer-administered and consists of section A-D. Qualitative data were collected using a Focus Group Discussion (FGD) guide with 12-item open-ended questions.
Validity of research instruments
Face and content validity of the research instruments were ensuring through subjection of the instruments to review by experts in Nursing and Midwifery, Obstetrics and Gynaecology, Demography and Social Statistics. Each item of the instruments was reviewed to ensure its appropriateness and ability to meet stated objective. Necessary corrections were affected on the research instruments after review by experts.
Reliability of the instrument
Reliability of the instruments was assessed through test-retest to ensure stability of the research instruments. This involved administering the questionnaire to expectant mothers in a health facility within the study area. This was repeated two weeks apart while internal consistency of questionnaire was examined by calculating Cronbach’s alpha value for the questionnaire. A value of 0.78 was estimated.
Procedure for data collection
The aim and objectives of this study were explained to the expectant mothers and informed consent to participate was obtained. Mothers’ socio-demographic characteristics such as age, marital status, occupation, highest education status, employment status, average monthly income was obtained using section A of the questionnaire. Section B obtained birth history, Section C assessed knowledge about danger signs of pregnancy, Section D examined birth preparedness among expectant mothers. FGD guide for qualitative data was translated into the local language (Yoruba) and recorded responses were transcribed into English by a language editor. Each session of FGD lasted approximately 60–90 minutes. Handwritten notes were also taken during the discussion and were used to supplement the audio recordings.
Data analysis and scoring
Quantitative data was processed using the Statistical Package for Social Sciences version 25. Analysis was carried out at univariate, bivariate and multivariate levels. Univariate analysis was conducted using the frequency and percentage distribution of mothers’ socio-demographic characteristics. Knowledge about obstetric danger signs was assessed using 16 items in section C of the questionnaire. Each correct response was scored ‘1’ point while incorrect option was scored ‘0’. Scores were summed up to a maximum of 16 points and minimum of ‘0’. Expectant mothers with total score of 8-16 points were categorized as ‘good knowledge’ while mothers with total score below 8 points were categorized as ‘poor knowledge’. Birth preparedness was assessed as a composite variable using the 10 items in section D of the questionnaire. Each of the 10 items were scored ‘1’ point. Scores were summed up to a maximum of 10 points and minimum of ‘0’. Expectant mothers with total score of 5-10 points were categorized as having ‘adequate preparation’ while mothers with total score below 5 points were categorized as having ‘inadequate preparation’. Predictors of birth preparedness among expectant mothers were examined at the bivariate level with Chi-square statistic to examine association between dependent variable and independent variables while binary logistic regression analysis was done to examine the simultaneous influence of independent variables on the dependent variables.
Analysis of qualitative data
The qualitative study explored similarities and differences in views regarding mothers’ perception about obstetric danger signs. Responses were analyzed and presented thematically.
Trustworthiness of qualitative data
Trustworthiness of qualitative data was evaluated in respect of credibility; dependability; confirmability and transferability.
Credibility of data: The aim and objectives of the study were explained to FGD participants prior data collection. Handwritten notes were also taken during the discussion and were used to supplement the audio recordings. FGD participants were given sufficient time to give their thoughts, clarify issues and contribute to discussion. Each session of FGD lasted approximately 60–90 minutes while total duration for qualitative data collection lasted 4 weeks.
Dependability: Qualitative responses were transcribed into English language by the researchers, codes were generated from FGD responses and were compared. A harmonized version was adopted.
Confirmability: Both audio recordings and field notes were compared and evaluated by researchers during transcription and coding of qualitative responses
Transferability: FGD sessions were held among expectant mothers aged 20-29 years old and 40-49 years old respectively. These are age groups observed to have higher risk of obstetric dangers in previous studies [17]. FGD sessions were held independently among these groups of expectant mothers to ensure homogeneity of responses and to ensure generalizability of our study findings.
Results
Quantitative findings shows that 30.4% of the expectant mothers were aged 20-29 years old, 61.7% were aged 30-39 years old, 7.9% were aged 40-49 years old, the mean age of the expectant mothers was 31 years ± 6SD while 33.1% were nullipara, 58.8% were primipara, 8.1% were multipara (Table1).
Table 1: Socio-demographic characteristics of Expectant mothers N=483
| Variables | Frequency | % |
| Age at last birthday (years) Mean=31±6SD | ||
| 20-29 | 147 | 30.4 |
| 30-39 | 298 | 61.7 |
| 40-49 | 38 | 7.9 |
| Marital status | ||
| Single | 38 | 7.9 |
| Married | 445 | 92.1 |
| Gravidity | ||
| Primigravida | 16 | 3.3 |
| Multigravida | 428 | 88.6 |
| Grand multigravida | 39 | 8.1 |
| Parity | ||
| Nullipara | 160 | 33.1 |
| Primipara | 284 | 58.8 |
| Multipara | 39 | 8.1 |
| Ethnicity | ||
| Yoruba | 345 | 71.4 |
| Igbo | 131 | 27.2 |
| Hausa | 07 | 1.4 |
| Religion | ||
| Christianity | 341 | 70.6 |
| Islam | 138 | 28.6 |
| Traditionalist | 04 | 0.8 |
| Highest level of education | ||
| Primary | 74 | 15.3 |
| Secondary | 216 | 44.7 |
| Tertiary | 193 | 40.0 |
| Employment status | ||
| Not employed | 70 | 14.5 |
| Self employed | 72 | 14.9 |
| Employed by Government | 150 | 31.1 |
| Employed by private sector | 191 | 39.5 |
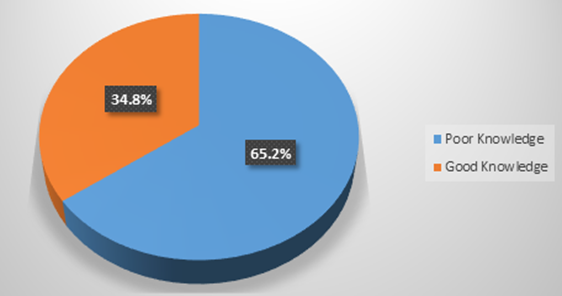
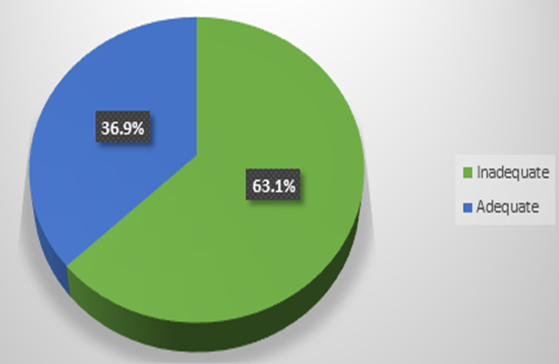
Study also observed that 34.8% of the expectant mothers had good knowledge about obstetric danger signs, 65.2% had poor knowledge (Figure1), 36.9% had adequate preparation towards childbirth while 63.1% had inadequate preparations (Figure2).
Figure 1: Knowledge about danger signs of Pregnancy.
Figure 2: Birth preparedness among expectant mothers.
Bivariate analysis of factors influencing birth preparedness among expectant mothers revealed significant relationship between birth preparedness and mother’s employment status (p=0.01) (Table2) while regression analysis shows that good knowledge about obstetric danger signs (p=0.03, OR=0.54. CI=0.31-0.94) was the main predictor of birth preparedness among expectant mothers. The odd that birth preparedness will be influenced by good knowledge about danger signs of pregnancy (OR=0.54) is less than that of poor knowledge. (Table3).
Table 2: Bivariate analysis of factors influencing Birth Preparedness among Expectant mothers N=483.
| Birth Preparedness | ||||
| Variables | Inadequate n (%) | Adequate n (%) | Total n (%) | Statistic χ2 df p |
| Age at last birthday(years) | 1.45 2 0.49 | |||
| 20-29 | 98 (66.7) | 49 (33.3) | 147 (100.0) | |
| 30-39 | 182 (61.1) | 116 (38.9) | 298 (100.0) | |
| 40-49 | 25 (65.8) | 13 (34.2) | 38 (100.0) | |
| Marital status | 0.13 1 0.94 | |||
| Single | 23 (60.5) | 15 (39.5) | 38 (100.0) | |
| Married | 282 (63.4) | 163 (36.6) | 445 (100.0) | |
| Gravidity | 3.01 2 0.22 | |||
| Primigravida | 13 (81.3) | 3 (18.8) | 16 (100.0) | |
| Multigravida | 270 (63.1) | 158 (36.9) | 428 (100.0) | |
| Grand multigravida | 22 (56.4) | 17 (43.6) | 39 (100.0) | |
| Parity | ||||
| Nullipara | 104 (65.0) | 56 (35.0) | 160 (100.0) | 1.00 2 0.61 |
| Primipara | 179 (63.0) | 105 (37.0) | 284 (100.0) | |
| Multipara | 22 (56.4) | 17 (43.6) | 39 (100.0) | |
| Ethnicity | ||||
| Yoruba | 215 (62.3) | 130 (37.7) | 345 (100.0) | 1.94 2 0.38 |
| Igbo | 87 (66.4) | 44 (33.6) | 131 (100.0) | |
| Hausa | 3 (42.9) | 4 (57.1) | 7 (100.0) | |
| Religion | 2.78 2 0.25 | |||
| Christianity | 214 (62.8) | 127 (37.2) | 341 (100.0) | |
| Islam | 90 (65.2) | 48 (34.8) | 138 (100.0) | |
| Traditionalist | 1 (25.0) | 3 (75.0) | 4 (100.0) | |
| Highest level of education | 5.35 2 0.07 | |||
| Primary | 47 (63.5) | 27 (36.5) | 74 (100.0) | |
| Secondary | 125 (57.9) | 91 (42.1) | 216 (100.0) | |
| Tertiary | 133 (68.9) | 60 (31.1) | 193 (100.0) | |
| Employment status | 14.77 3 0.01 | |||
| Not employed | 43 (61.4) | 27 (38.6) | 70 (100.0) | |
| Self employed | 42 (58.3) | 30 (41.7) | 72 (100.0) | |
| Employed by Government | 112 (74.7) | 38 (25.3) | 150 (100.0) | |
| Employed by private sector | 108 (56.5) | 83 (43.5) | 191 (100.0) | |
| Knowledge about danger signs of pregnancy | 1.45 1 0.23 | |||
| Poor | 205 (65.1) | 110 (34.9) | 315 (100.0) | |
| Good | 100 (59.5) | 68 (40.5) | 168 (100.0) | |
Table 3: Binary Logistic Regression Analysis of Factors Influencing Birth Preparedness among Expectant Mothers.
| Variables | P value | Odd ratio (OR) | Confidence interval (CI) |
| Age at last birthday (years) | |||
| 20-29 | RC | ||
| 30-39 | 0.53 | 1.38 | 0.51-3.76 |
| 40-49 | 0.11 | 2.38 | 0.83-6.80 |
| Marital status | |||
| Single | RC | ||
| Married | 0.42 | 0.61 | 0.18-2.05 |
| Gravidity | |||
| Primigravida | RC | ||
| Multigravida | 0.87 | 1.16 | 0.20-6.65 |
| Grand multigravida | 0.45 | 1.36 | 0.61-3.03 |
| Parity | |||
| Nullipara | RC | ||
| Primipara | 0.97 | 0.99 | 0.60-1.64 |
| Multipara | |||
| Ethnicity | |||
| Yoruba | RC | ||
| Igbo | 0.18 | 0.34 | 0.07-1.67 |
| Hausa | 0.22 | 0.35 | 0.07-1.67 |
| Religion | |||
| Christianity | RC | ||
| Islam | 0.21 | 0.22 | 0.02-2.32 |
| Traditionalist | 0.24 | 0.25 | 0.02-2.60 |
| Highest level of education | |||
| Primary | RC | ||
| Secondary | 0.89 | 1.05 | 0.51-2.16 |
| Tertiary | 0.92 | 0.97 | 0.56-1.68 |
| Employment status | |||
| Not employed | RC | ||
| Self employed | 0.83 | 1.11 | 0.43-2.89 |
| Employed by Government | 0.06 | 2.56 | 0.96-6.84 |
| Employed by private sector | 0.11 | 2.51 | 0.80-7.82 |
| Knowledge about danger signs of pregnancy | |||
| Poor | RC | ||
| Good | 0.03 | 0.54 | 0.31-0.94 |
| Model statistics: N=483, χ2= 25.78, P= 0.11. | |||
Qualitative findings
FGD were held among mothers aged 20-29 years old and 40-49 years old respectively. Main themes from qualitative responses regarding perception about danger signs of pregnancy include Knowledge about obstetric danger signs; Recognition of obstetric danger signs; Perceived severity of obstetric danger signs and Perceived susceptibility to obstetric danger signs (Table 4).
Table 4: Thematic analysis of responses from focus group discussions
| Main Themes | Sub-themes |
| Knowledge about obstetric danger signs | -Obstetric danger signs are warning signs |
| -Obstetric danger signs point to severe | |
| consequences | |
| -Obstetric danger signs could appear | |
| during any stage of pregnancy | |
| Recognition of obstetric danger signs | -Obstetric danger signs could occur during pregnancy, labour and puerperium |
| -Obstetric dangers could be averted or | |
| consequences reduced | |
| Perceived severity of obstetric danger signs. | -Obstetric danger signs could be life |
| threatening | |
| -Obstetric danger signs require prompt | |
| medical attention | |
| Perceived susceptibility to obstetric danger signs | -Recognizing obstetric danger signs is |
| important towards seeking treatment | |
| -Cultural and social misconception are | |
| responsible for severity and poor help | |
| seeking behavior |
Knowledge about obstetric danger signs: FGD participants generally described obstetric danger signs as those warning signs that point to severe consequences during any stage of pregnancy. Majority of the FGD participants had good knowledge about obstetric danger signs while significant proportion also had inadequate birth preparations Participants opined that these dangers could be averted or their consequences reduced if reported early. FGD participants opined that vaginal bleeding, drainage of fluids, severe pain, headache are among danger signs of pregnancy and these signs could appear at any stage during pregnancy.
Recognition of obstetric danger signs: Participants at the FGD generally opined that danger signs could occur during pregnancy, labour and pueperium and these signs could include but not limited to headache, blurring of vision, body weakness, loss of appetite, body swelling and reduced fetal activities. Below are exerts from FGD responses:
‘…If a pregnant woman experiences headache, body pain, or leg swelling, she must immediately visit the hospital because these may be signs of danger or complications. I do not know of any danger signs during labour but I have experienced tiredness after delivery before and the nurses said it a sign of danger’ (a 25-year-old discussant)
‘…I know of headache and abdominal pain as danger signs during pregnancy. I have experienced severe abdominal pain and dizziness during pregnancy when I am close to giving birth before, I report at the hospital and I was admitted and given medications’ (41-year-old discussant)
Perceived severity of obstetric danger signs: FGD participants believed that pregnancy and labour are life threatening processes and any discomfort or danger signs should be considered life threatening requiring prompt attention.
A 32-year-old discussant retorted that ‘…Pregnancy and labour could be life threatening to the mother and child. The discomfort and pain during labour is very high. Sometimes one feels like dying or fainting. Any signs of abnormality during this period could be life threatening especially if not recognized or properly managed’.
Perceived susceptibility to obstetric danger signs: Responses from the FGD revealed that ability of a pregnant woman to recognize danger signs during pregnancy remain an important step towards seeking solution or treatment. Participants opined that most fatalities during pregnancy are as a result of failure to recognize these danger signs, belief or misconception that such danger signs are not severe enough to cause harm, or when such danger signs occur, they could be managed in a traditional way such as use of herbs are responsible for poor health seeking behavior among pregnant women. Below are exerts from participants:
naeco‘…When danger signs such as headache, abdominal pains or bleeding during pregnancy are not reported to the hospital early enough, the pregnancy might be at risk for the woman and her baby. A pregnant woman must book early so that nurses or doctors can recognize the danger signs and treat before complications happen’ (a 27 year old discussant).
‘…Some danger signs may not be as severe as others. Some danger signs in pregnancy such as headache can resolve on its own if the woman rest properly at home especially if the clinic is too far from the woman’s house’ (a 43 year old discussant).
Qualitative responses also observed that various forms of cultural and social misconceptions were responsible for poor health seeking behaviours including birth preparedness among expectant mothers and most fatalities during pregnancy.
‘…There are traditional herbs or cultural practices that can stop or prevent pregnant women from having complications, but for me, I only take herbs after delivery only’ (25-year-old discussant).
Discussion of findings
Study observed that 34.8% of the expectant mothers had good knowledge about obstetric danger signs while 65.2% had poor knowledge. A similar study undertaken by Salem et al. [18] in Madagascar observed that the proportion of pregnant women who has knowledge about obstetric danger signs was at least 51.9% while Nigussie et al [13] in their study involving pregnant women in northwestern Ethiopia found that 37.9% of the women had good knowledge about danger signs of pregnancy. The above finding however contrast the result of similar study in southern Ethiopia which observed that 16.8% of the pregnant women studied were knowledgeable about obstetric danger signs[19]. Adequate knowledge about obstetric danger signs is essential towards early recognition and prompt intervention or timely referral [14].
This study also found that 36.9% of the expectant mothers had adequate preparation towards childbirth while 63.1% had inadequate preparations. This finding corroborate the observation made by a study conducted in Abakaliki, eastern Nigeria found that 36.9% of women studied had birth preparedness while 44.9% had adequate knowledge about birth preparedness [20]. This however contrast the observation by Kamineni et al. [21] who observed that 71.5% of studied women in an Indian study were birth prepared. Teekhasaenee & Kaewkiattikun similarly found that 78.4% of pregnant adolescents in a study in Thailand had good birth preparedness and complication readiness [22]. A study conducted in Ethiopia however revealed that 34% of the women studied implemented complication readiness and birth preparedness [8]. Similarly, another cross-sectional study conducted in western Ethiopia women revealed that 27.5% of the women had adequate preparation for childbirth [23]. The above findings however contrast the report of a study conducted in Cameron which found that 18.8% of the women studied were considered to have adequate birth preparation [24].
Regarding factors that are associated with birth preparedness, regression analysis shows that good knowledge about danger signs of pregnancy was the main predictor of birth preparedness among expectant mothers. Similarly Markos & Bogale [8] in their study among pregnant women in Ethiopian observed that place of residence, educational status, antenatal care follow up, previous history of still births, knowledge about birth preparedness, knowledge about danger signs of pregnancy, were significantly associated with birth preparedness. Similarly, Kamineni et al. [21] in their study among pregnant women in India observed that maternal education attainment and early booking were significantly associated with birth preparedness while Asrat et al. [23] found that urban residency, prim gravidity, previous history of obstetric complication and attendance of antenatal care were associated with birth preparedness. Teekhasaenee & Kaewkiattikun [22] in Thailand however found that frequency of antenatal care visits was associated with birth preparedness. Birth preparedness and complication readiness remain vital strategy towards reduction in maternal mortality and morbidity [8].
Regarding perception about danger signs of pregnancy, participants at the FGD generally opined that danger signs could occur during pregnancy, labour and puerperium and that undesirable events during pregnancy and labour should be considered life threatening requiring prompt attention. A section of FGD participants however believed that culture and traditions have some role to play in managing danger signs in pregnancy. This assertion corroborate finding made by Bakar et al. [15] from a qualitative study involving women of reproductive age in Unguja Island, Zanzibar where it was observed that study participants believed that danger signs during pregnancy and puerperium are as a result of witchcraft activities resulting in some consultations with traditionalists thereby contributing to delay in seeking skilled medical care. Positive perception and adequate knowledge about obstetric danger signs by the pregnant woman enhances her cognitive disposition towards pregnancy complications and appropriate decision making ability, thereby reducing cultural and religious misconceptions typical of most African setting [15].
Strength and limitation of the study
This study was carried out in southwest Nigeria. A more nationally representative data could be necessary for public health policy planning. The study sample in this study could however be considered reasonably representative comprising of different categories of expectant mothers with respect to educational background, marriage types, parity and employment status. The statistical tool employed and findings obtained in this study could be comparable with those obtainable from previous studies.
Conclusion
Good knowledge about obstetric danger signs was the main predictor of birth preparedness among expectant mothers; effective maternal health services aiming at favorable pregnancy outcomes should focus on educating women on early identification of obstetric danger signs and prompt decision making capabilities.
Declarations
Implication of findings for Nursing and Midwifery practices
Functional midwifery practices should continue to focus on designing appropriate strategies towards educating expectant mothers on regular antenatal visit, early recognition of danger signs of pregnancy and need for prompt intervention during pregnancy, labour, and postpartum.
Ethical consideration
Ethical permissions for this study were obtained from the Ethics and Research Committee of Bowen University, Iwo, Osun state, Southwest Nigeria and Ladoke Akintola Teaching Hospital, Ogbomosho, Oyo state, south-west Nigeria. Informed consent was also obtained from selected expectant mothers prior data collection.
Conflicts of interest
Authors declare no conflict of interest in the course of conduct and publication of this manuscript.
Funding
This research did not receive any grant or financial aid from any funding agencies in the public, commercial, or not-for-profit sectors.
References
- World Health Organization (WHO). (1998). Safe Motherhood Initiative.
Publisher | Google Scholor - World Health Organization (WHO). (2019). World Health Statistics 2019: Monitoring Health for the Sustainable Development Goals.
Publisher | Google Scholor - Ope BW. (2020). Reducing maternal mortality in Nigeria: addressing maternal health services’ perception and experience. J Glob Heal Reports, 4:1-4.
Publisher | Google Scholor - Wassihun B, Negese B, Bedada H, Bekele S, Bante A, Yeheyis T, et al. (2020). Knowledge of obstetric danger signs and associated factors: a study among mothers in Shashamane town, Oromia region, Ethiopia. Reprod Heal, 17(4):1-8.
Publisher | Google Scholor - Ngonzi J, Tornes YF, Mukasa PK, Salongo W, Kabakyenga J, Sezalio M, et al. (2016). Puerperal sepsis, the leading cause of maternal deaths at a Tertiary University Teaching Hospital in Uganda. BMC Pregnancy Childbirth, 16(207):1-7.
Publisher | Google Scholor - Limenih MA, Belay HG, Tassew HA. (2019). Birth preparedness, readiness planning and associated factors among mothers in Farta district, Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth, 19(171):1-10.
Publisher | Google Scholor - (2004). Johns Hopkins Program for International Education in Gynaecology and Obstetrics (JHPIEGO). Maternal and Neonatal Health Program Monitoring Tool and indicators for maternal and newborn health. Johns Hopkins: Bloomberg school of Public Health, Centre for Communication programs. Family Care International.
Publisher | Google Scholor - Markos D, Bogale D. (2014). Birth preparedness and complication readiness among women of child bearing age group in Goba woreda, Oromia region, Ethiopia. BMC Pregnancy Childbirth, 14(282):1-9.
Publisher | Google Scholor - Bintabara D, Mpembeni RNM, Mohamed AA. (2017). Knowledge of obstetric danger signs among recently-delivered women in Chamwino district, Tanzania: a cross-sectional study. BMC Pregnancy Childbirth, 17(276):1-10.
Publisher | Google Scholor - Ayebare E, Lavender T, Mweteise J, Nabisere A, Nendela A, Mukhwana R, et al. (2021). The impact of cultural beliefs and practices on parents’ experiences of bereavement following stillbirth: a qualitative study in Uganda and Kenya. BMC Pregnancy Childbirth, 21(443):1-10.
Publisher | Google Scholor - Rianga MR, Nangulu AK, Broerse JEW. (2018). Perceived causes of adverse pregnancy outcomes and remedies adopted by Kalenjin women in rural Kenya. BMC Pregnancy Childbirth, 18(408):1-16.
Publisher | Google Scholor - Ntoimo FLC, Okonofua EF, Ekwo C, Solanke TO, Igboin B, Imongan W, et al. (2022). Why women utilize traditional rather than skilled birth attendants for maternity care in rural Nigeria: Implications for policies and programs. Midwifery, 104:103-158.
Publisher | Google Scholor - Nigussie AA, Emiru AA, Demilew YM, Mersha EA. (2019). Factors associated with knowledge on obstetric danger signs among women who gave birth within 1 year in Bahir Dar city administration, North West, Ethiopia. BMC Res Notes, 12(117):1-6.
Publisher | Google Scholor - Tamang ST, Dorji T, Yoezer S, Phuntsho T, Dorji P. Knowledge and understanding of obstetric danger signs among pregnant women attending the antenatal clinic at the National Referral Hospital in Thimphu, Bhutan: a cross-sectional study. BMC Pregnancy Childbirth, 21:104.
Publisher | Google Scholor - Bakar RR, Mmbaga B, Manongi R. (2019). Awareness of danger signs during pregnancy and post-delivery period among women of reproductive age in Unguja Island, Zanzibar: A Qualitative study. Afr J Reprod Health, 29063.
Publisher | Google Scholor - (2006). Federal Republic of Nigeria. National Population and Housing Census.
Publisher | Google Scholor - Afolabi OA, Olaogun AA, Afolabi KA, Afolabi EK. (2020). Determinants of unintended pregnancies among nursing mothers in southwest Nigeria. Afr J Midwifery Womens Health, 1-17.
Publisher | Google Scholor - Salem A, Lacour O, Scaringella S, Herinianasolo J, Benski AC, Stancanelli G, et al. (2018). Cross-sectional survey of knowledge of obstetric danger signs among women in rural Madagascar. BMC Pregnancy Childbirth, 18(46):1-9.
Publisher | Google Scholor - Bolanko A, Namo H, Minsamo K, Addisu N, Gebre M. (2021). Knowledge of obstetric danger signs and associated factors among pregnant women in Wolaita Sodo town, South Ethiopia : A community-based cross-sectional study. SAGE Open Med, 9:1-9.
Publisher | Google Scholor - Anikwe CC, Okorochukwu BC, Ikeoha CC, Asiegbu OGK, Nnadozie UU, Eze JN, et al. (2020). Birth Preparedness and Complication Readiness among Pregnant Women in a Secondary Health Facility in Abakaliki, Ebonyi. Biomed Res Int.
Publisher | Google Scholor - Kamineni V, Murki AD, Kota VL. (2017). Birth preparedness and complication readiness in pregnant women attending urban tertiary care hospital. J Fam Med Prim Care, 297-300.
Publisher | Google Scholor - Teekhasaenee T, Kaewkiattikun K. (2020). Birth Preparedness and Complication Readiness Practices Among Pregnant Adolescents in Bangkok. Adolesc Health Med Ther, 11:1-8.
Publisher | Google Scholor - Asrat T, Baraki N, Assefa N, Alemkere G. (2019). Birth Preparedness among Women Who Gave Birth in the Last Twelve Months in Jardega Jarte District, Western Ethiopia. J Pregnancy.
Publisher | Google Scholor - Ijang YP, Nambile S, Cumber N, Nkfusai CN, Venyuy MA, Bede F, et al. (2019). Awareness and practice of birth preparedness and complication readiness among pregnant women in the Bamenda Health District, Cameroon. BMC Pregnancy Childbirth, 19:371.
Publisher | Google Scholor