Research Article
Birth Outcomes of Twin’s Pregnancy and Associated Factors in Selected Public Hospitals of Addis Ababa, Ethiopia, 2022
1KEA-MED College of Health Science department of Public Health, Addis Ababa, Ethiopia.
2Department of Public Health, College of Health Science, Debre Berhan University, Debre Berhan, Ethiopia
*Corresponding Author: Chala Getaneh, KEA-MED College of Health Science department of Public Health, Addis Ababa, Ethiopia.
Citation: Getaneh C., Lambebo A., Goshime T., Mezemir Y. (2024). Birth Outcomes of Twin’s Pregnancy and Associated Factors in Selected Public Hospitals of Addis Ababa, Ethiopia, 2022, Journal of Clinical Paediatrics and Child Health Care, BioRes Scientia Publishers. 1(1):1-11. DOI: 10.59657/2997-6111.24.003
Copyright: © 2024 Chala Getaneh, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 12, 2023 | Accepted: January 03, 2024 | Published: February 01, 2024
Abstract
Background: Twin birth is a type of multiple births when the mother gives birth to two offspring from the same pregnancy. The prevalence rates range from less than 8 twin pregnancies per 1,000 births in the East and Southern Asia, India, and Oceania to 17 or more per 1,000 births in Africa. There are factors to increase the negative birth outcome of twin delivery; from these, some of them are associated with increased maternal age, prim parity, low birth weight, chronic disease, low ANC follow-up, and PROM. Adverse birth outcome for twin delivery is a critical health issue in developing countries such as Ethiopia. It resulted in many bad consequences, neonatal and infant morbidity and mortality.
Objective: The objective of this study was to assess birth out come and associated factors of twin’s pregnancy in selected public Hospitals, Addis Ababa, Ethiopia.
Methods: Facility based cross sectional study was conducted on 246 maternal records of twin delivery in selected public hospitals of Addis Ababa to assess birth out come and associated factors of twin’s pregnancy from December, 2020-June, 2021.A pretested questionnaire which will be analyzed by SPSS and result will be reported in tables, bivariate and multivariate regression will be done to show correlations by Crude and adjusted odds ratio. A confidence limit of 95% and p- value less than 0.05 will be used as cut of point to see presence of statistical significance.
Result: The prevalence of adverse birth outcome (Both maternal and fetal) among twin delivery in the three selected public hospitals of Addis Ababa is 234 (95%). majority, 156(63.4%) were in the age group 18-28 years, with the mean age of 29.78 and Standard deviation of±6.53. Most of the mothers 227(92%) were married. Mothers who had Pregnancy induced hypertension (AOR= 10.465, 95% CI (2.922-37.474)), Mothers who had ruptured membrane before the onset of Labor (AOR= 3.577, 95% CI (1.198-10.682)) and Mothers who labor for more than 12 hours were (AOR= 3.324, 95% CI (1.101-10.034)) were significantly associated with adverse maternal birth outcome. While mothers who had ANC follow up at private clinic (AOR= 0.252, 95% CI (0.098-0.649)) and Mothers who live outside Addis Ababa were unlikely to have adverse fetal outcome (AOR= 0.343, 95% CI (0.143-0.826)).
Conclusion: Adverse birth outcome of Twins pregnancy is relatively higher when compared to similar studies conducted in Ethiopia. The health facilities should have effective risk assessment in Antenatal care unit and labor ward. It is also recommended to have guidelines and protocols for the management of twin’s pregnancy. Since the Prevalence of Adverse twin’s Birth outcome is higher greater attention should be given on both Antepartum and Intrapartum care.
Keywords: birth outcomes; twin’s pregnancy; public hospitals; addis ababa
Introduction: Background
Twin birth is a type of multiple births when the mother gives birth to two offspring from the same pregnancy [1]. Twin pregnancy can be either dizygotic or monozygotic. Dizygotic or fraternal twins usually results from the fertilization of two separate ova while monozygotic or identical twin arises from a single fertilized ovum. Dizygotic (Fraternal also known as non-identical twins) develops from two different ova and sperm cells. Dizygotic twins do not share a placenta or amniotic sac, and their faces are not as similar as identical twins’ appearances [1, 2]. Twin pregnancies account for 2 to 4% of the total number of births. Spontaneous twin pregnancy rates vary worldwide. The prevalence rate ranges from less than 8 twin pregnancies per 1,000 births in the East and Southern Asia, India, and Oceania to 17 or more per 1,000 births in Africa [2]. The highest rates of twin pregnancies are found in Nigeria and the lowest rates occur in Japan. This difference is mainly due to dizygotic twin pregnancies, since the prevalence of monozygotic pregnancies is practically constant, ranging from 3.5 to 4 per 1,000 births [4]. Dizygotic twinning is much more common than monozygous splitting of a single oocyte. The frequency of monozygotic twin births is relatively common worldwide, approximately one set per 250 births.[5]. This incidence is generally independent of race, hereditary, age and parity. By contrast the incidence of dizygotic twinning is influenced by race, heredity, maternal age, parity, and fertility treatment [6]. Advanced maternal age has been associated with increased incidence of twinning. When a woman gives birth to twins after the age of 35, there is a higher chance of bearing twins. That is because as the woman gets older, there is a high tendency to release more than one ovum when ovulating due to increased gonadotropins [7]. A dizygotic twin descends from the mother’s side. If a woman has a mother or grandmother who is dizygotic twin, the odds of having dizygotic twin is higher. In addition, a woman who had previous twin’s pregnancy will have greater chance of having twins. This means the reproductive system works well and ovulation is not problematic, so the possibility of producing more than one ovum when ovulating is higher [4,7]. Incidence of twin pregnancy is increasing all over the world because of Assisted Reproductive Technology (ART). Multiple gestation rates are high in assisted reproductive treatment cycles because of the perceived need to stimulate excess follicles and transfer excess embryos to achieve reasonable pregnancy rates [7]. In vitro fertilization (IVF) can lead to a multiple pregnancy if more than one embryo is transferred to the uterus. Identical multiples also may result if the fertilized egg splits after the transfer of embryo.
Methods and Materials
Study design and period: Facility based cross sectional study was conducted to assess birth out come and associated factors of twin pregnancy from April, 2020-June, 2021.
Study area
The study was done in Gandhi memorial hospital, Zewditu memorial hospital and Ras Desta hospital Addis Ababa, Ethiopia, as of 2015 Addis Ababa city had 3.238 million inhabitants with male to female ratio of 0.99.Currently the city Administration has 06 public hospitals, 25 private hospitals, more than 97 health centers and about 500 clinics according to EDHS 2016.Gandhi Memorial Hospital, Zewditu memorial hospital and Ras Desta hospital are some of the hospitals that are capable in providing comprehensive care to pregnant women, labor and delivery services including critical maternal and neonatal care. The hospitals serve 21, 16 and 15 Catchment Health centers respectively.
Population
Source population: The source population of this study was all twin delivery records of selected public hospitals of Addis Ababa with in the period of December, 2020-June, 2021.
Study population: The study population of this study was all twin delivery recorded in delivery record from December, 2020- June, 2021 and fulfilled the eligibility criteria.
Study Participants
Inclusion criteria: All twin delivery records of selected public hospitals of Addis Ababa during the study period that have a gestational age of 28 weeks or more and at least one of the new born weighs 1000 grams or more.
Exclusion criteria: Twin delivery records that have incomplete recorded information on the delivery register was excluded from this study.
Sample size determination and Sampling technique
Sample size required for this study was calculated using formula for a single population proportion by taking proportion rate of 20% of adverse twin birth outcome rate [2,3]. 95% level of significance and 5% margin of error or precision. Sample size was determined using the following formula:
n = (za/2) 2 P (1 – P) = (1.96)2*0.2(1-0.2) = 246
d2 0.052
Where: P=20% (proportion of birth outcome); Zα/2= critical value at 95% confidence level of certainty (1.96); D= the margin of error between the sample and the population or desired precision (5%); n= sample size
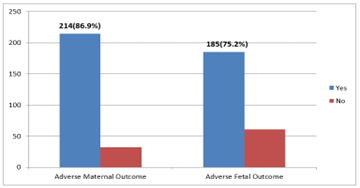
Figure 1: Shows prevalence of adverse birth outcome among women who had Twins delivery in selected public hospitals of Addis Ababa.
Sampling procedure
Under Addis Ababa City administration there are a total of 06 hospitals. Among them Gandhi Memorial Hospital, Zewditu Memorial Hospital and Ras Desta Hospital was selected by purposive sampling method based on their delivery load and the sample size was allocated proportionally based on the average delivery load of the hospitals in the past three months. A total of 11816 deliveries were there at the selected public hospitals during the study period. From the total number of deliveries, 5303 of them were from Gandhi Memorial Hospital; out of which 149 were twin deliveries, 3952 deliveries of them from Ras Desta Hospital; out of which 120 were twin deliveries and the rest 2561 of them from Zewditu Memorial Hospital; out of which 101 are twin deliveries. The sample size is allocated proportionally for each hospital. Twin charts will be selected from each hospital using a simple random sampling method. Since the number of twin deliveries is different for each hospital, proportion for each hospital has been calculated using the formula below.
Proportional for each selected hospital = 
| Total Number of twin deliveries at selected public hospitals = 370 | ||
| GMH = 149 | Ras Desta = 129 | ZMH = 101 |
| Total calculated sample size = 246 | ||
Figure 2: Figure showing sample size procedures for selecting samples for the study from the public hospitals in Addis Ababa, Ethiopia.
Data collection Procedures and tools
Data were collected by reviewing the charts of twin’s delivery during the data collection period. The data collectors were midwives from Gandhi Memorial Hospital, Zewditu Memorial Hospital and Ras Desta Hospital. Structured checklist was developed after reviewing relevant literatures. The checklist was designed to obtain relevant information on the predictor variables such as demographic, obstetric, maternal complication, intervention, and component of modified WHO Partograph. The conditions of the baby such as Apgar score was assessed and Apgar score of 7 was considered as satisfactory [2,3]. The questionnaire was developed in English and later translated in to Amharic, the local language of the city and consistency and accuracy check was done to ensure proper and correct translation of the questions by back translation to English.
Study variables
Dependent variables: Birth outcome of Twins pregnancy
Independent variables
Maternal Demographic Factors-Age, religion, marital status and residence.
Obstetric Factors- includes gravidity, parity, Number of prior twins’ pregnancy.
Ante partum related Factors-includes number of ANC visits Obstetric and Medical complications during labor.
Intrapartum related Factors- mode of delivery, gestational age at onset of labour, Apgar score, Birth weight and sex of the new born.
Operational definitions
Twins birth: a type of multiple births when the mother gives birth to two offspring from the same pregnancy (1).
Birth outcome: Includes both maternal and fetal outcome [2,5].
Normal maternal outcome: mothers who had normal birth outcome without complications like hypertension, preterm delivery, traumatized labour/tear, C/S delivery, ICU admission, Polyhydraminos, hypothyroidisms and maternal death [2,5].
Adverse maternal birth outcome: mothers who had at least one of the following complications like preterm deliveries, PIH, birth injury/tear, C/S delivery, instrumental delivery, ICU admission, Polyhydraminos, hypothyroidisms, maternal death [2,5].
Normal Fetal outcome: fetal/neonatal outcomes without the following complications (preterm, RDS, LBW, macrosomia, poor Apgar score, birth injury, birth defect, IUFD, still birth, admission to the neonatal intensive care unit [2,5].
Adverse fetal outcome: refers to neonates who had at least one of the following adverse complications (preterm, RDS, LBW, macrosomia, poor Apgar score, birth injury, birth defect, IUFD, still birth, admission to the neonatal intensive care unit.
Good Apgar score: refers to when Apgar score is greater than seven at 5min of birth [10].
Poor Apgar score: refers to when Apgar score is less than seven at 5min of birth [10].
Data entry and analysis
After data collection, each questionnaire was checked for completeness based on the code given during data collection. The collected data was entered to Epi Data 4.2 software which secured further data quality by reducing errors made while data entry. Then entered data was transported to SPSS version 25.0 for data analysis. Descriptive statistics like frequency tables, graphs and descriptive summaries was used to describe the independent variables. Those factors found with their P value less than 0.20 in the bi-variable logistic regression model were fitted in to the multivariable logistic regression model to control the effect of confounding variables. Multivariable analysis using standard logistic regression technique was done to evaluate the independent effect of each covariate on birth outcome of twin’s pregnancy. A confidence limit of 95% and p- value less than 0.05 was used as a cut of point to see presence of statistical significance. To control the effect of confounding variables stepwise multiple logistic regression analysis was done. The Hosmer- Lemeshow statistic had significant value of 0.65 which shows that the model was fit.
Result
Socio-Demographic Characteristics
There was a total of 11,816 deliveries in Gandhi Memorial Hospital, Zewditu Memorial Hospital and Ras Desta Hospital from December 2020- June 2021.Out of those deliveries 370 of them were twin deliveries. Among the total twin deliveries 246 maternal charts that had complete records were reviewed in the study. Majority, 156(63.4%) were in the age group 18-28 years, with the mean age of 27.3 and Standard deviation of±4.29. Most of the mothers 227(92%) were married. From the total records one quarter (25%) resides in rural area.
Table 1: Frequency distribution of participant Socio-demographic variables in Selected public hospitals of Addis Ababa, Ethiopia, 2022 (n=246).
| Variable | Category | Frequency | Percent (%) |
| Sex of fetus | Male and Male | 82 | 33.3% |
| Female and Female | 75 | 30.5% | |
| Male and Female | 89 | 36.2% | |
| Age in year | 18-28 | 156 | 63.4% |
| 29-39 | 86 | 35% | |
| 40-50 | 4 | 1.6% | |
| Marital status | Single | 15 | 6% |
| Married | 227 | 92.2% | |
| Divorced | 04 | 1.8% | |
| Residence | Addis Ababa | 184 | 74.8% |
| Outside Addis Ababa | 62 | 25.2% |
Obstetric Variables
In this study 174(70.7%) of the mothers were Multi gravid and 93 (37.8%) of the mothers were Nulliparous. All of the mothers (246) in this study had no prior history of twin’s pregnancy while 32 (13%) have prior history of twin’s pregnancy.
Table 2: Frequency distribution of participants Obstetric variables in Selected public hospitals of Addis Ababa, Ethiopia, 2022 (n=246).
| Variable | Category | Frequency | Percent (%) |
| Gravidity | Primigravida | 72 | 29.3% |
| Multi gravid | 174 | 70.7% | |
| Parity | Nulliparous | 93 | 37.8% |
| Primiparous | 74 | 30.1% | |
| Multiparous | 79 | 32.1% |
Ante-partum related variables
About 232 (94.3%) mothers in this study had ANC follow up. Among the mothers who had ANC follow up 154 (62.6%) of the mothers had ANC follow up in the respective public Hospitals and 121 (52.1%) Start their ANC follow up in less than three months of gestation. Among the mothers in this study 101 (41.1%) had prior obstetric complication while 10(4.1%) had prior medical history before delivery.
Table 3: Frequency distribution of participants Antepartum variables in Selected public hospitals of Addis Ababa, Ethiopia, 2022 (n=246).
| Variable | Category | Frequency | Percent (%) |
| ANC follow up | Yes | 232 | 94.3% |
| No | 14 | 5.7% | |
| Place of ANC visit | Health Center | 71 | 30.6% |
| Private Hospital | 07 | 3% | |
| Governmental Hospital | 154 | 66.4% | |
| GA at first ANC visit | < 3> | 121 | 52.1% |
| >3 months | 111 | 47.9% |
Prevalence of adverse Birth outcome
Among the 246 participants 214 (86.9%) have adverse maternal birth outcome while 32 (13.1%) have good maternal outcome while out of 246, 185(75.2%) have adverse fetal birth outcome while 61(24.8%) has good fetal birth outcome.
Table 4: Frequency distribution of participants Intrapartum variables in Selected public hospitals of Addis Ababa, Ethiopia, 2021 (n=246).
| Variable | Category | Frequency | Percent (%) |
| First twin fetal presentation | Cephalic | 164 | 66.7% |
| Breech | 80 | 32.5% | |
| Others | 02 | 0.8% | |
| GA during labor | 28-32 | 33 | 13.4% |
| 33-37 | 72 | 29.3% | |
| >37 | 141 | 57.3% | |
| Membrane status | Intact | 143 | 58.1% |
| Ruptured | 103 | 41.9% | |
| Duration of labor | < 12> | 184 | 74.8% |
| >12 hours | 62 | 25.2% | |
| Partograph Utilization | Yes | 56 | 22.8% |
| No | 129 | 52.4% | |
| Not applicable | 61 | 24.8% | |
| Mode of delivery | SVD | 101 | 41.1% |
| C/S | 139 | 56.5% | |
| Both | 06 | 2.4% | |
| Delivery Outcome | Both alive | 226 | 91.9% |
| One still born and one alive | 14 | 5.7% | |
| Both still born | 06 | 2.4% | |
| Birth weight | Both NBW | 68 | 27.6% |
| Both LBW | 133 | 54.1% | |
| One NBW and LBW | 45 | 18.3% |
Factors associated with Adverse Birth Outcome
Bi-variable analysis result showed that Maternal age, Marital status, Gravidity, Parity, Presence of ANC follow up, Place of ANC visit, Number of ANC visit, Obstetric complication before delivery, Membrane status and GA during labor, Duration of labor were significantly associated with adverse maternal birth outcome while Age of the mother, Marital status, Residence Gravidity, Parity, Prior abortion, Place of ANC visit, Number of ANC visit, GA during labor were significantly associated with adverse fetal birth outcome.
Table 5: Patterns of Adverse birth out come in selected public hospitals of Addis Ababa, Ethiopia 2022 (n=246)
| Adverse Maternal Birth out come | |||
| Variable | Category | Frequency | Percent |
| Preterm Delivery | Yes | 105 | 42.60% |
| NO | 141 | 57.40% | |
| C/S + Instrumental delivery | Yes | 145 | 58.95% |
| NO | 101 | 41.05% | |
| Oligohydraminos + Polyhydraminos | Yes | 14 | 5.70% |
| NO | 232 | 94.30% | |
| Maternal Admission to ICU | Yes | 6 | 2.40% |
| NO | 240 | 97.60% | |
| Adverse Fetal Birth out come | |||
| Variables | Category | Frequency | Percent |
| Preterm | Yes | 105 | 42.60% |
| NO | 141 | 57.40% | |
| Low birth weight | Yes | 178 | 72.40% |
| NO | 68 | 27.60% | |
| Poor APGAR score | Yes | 39 | 15.80% |
| NO | 207 | 84.10% | |
| Still birth | Yes | 20 | 8.20% |
| NO | 226 | 91.80% | |
| Birth Defect | Yes | 2 | 0.80% |
| No | 244 | 99.20% | |
| Neonatal Admission to NICU | Yes | 146 | 60.80% |
| NO | 94 | 39.20% | |
In multivariable analysis Obstetric complication before delivery, Membrane status during labor and Duration of labor were identified to be significantly associated with adverse maternal birth outcome while Marital status and GA during Labor were significantly associated with Adverse fetal birth outcome. Mothers who had Pregnancy induced hypertension were (AOR= 10.465,95% CI (2.922-37.474)) ten times more likely to develop adverse Maternal birth outcome compared to mothers who had no Pregnancy induced hypertension. Mothers who had ruptured membrane before the onset of Labor were three times more likely to develop adverse maternal birth outcome as compared to mothers who had intact membrane before onset of labor. (AOR= 3.577, 95% CI (1.198-10.682)). Mothers who labor for more than 12 hours were (AOR= 3.324, 95% CI (1.101-10.034)) more likely to develop adverse maternal birth outcome. Mothers who had ANC follow up at private clinic were less likely to have adverse fetal birth outcome than that of mothers who had ANC follow up at Health center and Governmental hospital. (AOR= 0.252, 95% CI (0.098-0.649)). Mothers who live outside Addis Ababa were unlikely to have adverse fetal out come as compared to mothers who resides in Addis Ababa. (AOR= 0.343, 95% CI (0.143-0.826)).
Table 6: Factors associated with Adverse birth out come in selected public hospitals of Addis Ababa, Ethiopia 2022 (n=246).
| Variables | Category | Adverse maternal birth outcome | COR (95%CI) | AOR (95%CI) | P- Value | |
| Yes | NO | |||||
| Marital Status of mother | Single | 17 | 2 | 2.488 [0.587-10.538] | 1 | 1 |
| Married | 195 | 28 | 0.772[0.112-5.319] | 0.793 | ||
| Widowed | 2 | 2 | 721 | 0 | ||
| Age | 18-28 | 137 | 19 | 1.107[0.547-2.242] | 1 | 1 |
| 29-39 | 73 | 13 | 0.528[0.151-1.852] | 0.319 | ||
| 40-50 | 4 | 0 | 0 | 0.999 | ||
| Gravidity | PG | 66 | 6 | 1.932[0.759-4.197] | 1 | 1 |
| MG | 148 | 26 | 5.240[0.707-38.8] | 0.105 | ||
| Parity | NP | 84 | 9 | 1.425 [0.907-2.238] | 1 | 1 |
| PP | 65 | 9 | 1.497[0.255-8.791] | 0.655 | ||
| MP | 65 | 14 | 1.544 [0.238-10.05] | 0.648 | ||
| Presence of ANC | Yes | 202 | 12 | 1.122 [0.239-5.262] | 1 | 1 |
| No | 30 | 2 | 0.165 [0.016-1.742] | 0.134 | ||
| Place of ANC | H.C | 64 | 7 | 1.183 [0.812-1.726] | 1 | 1 |
| Private Hospital | 7 | 0 | 0.446 [0.112-1.766] | 0.25 | ||
| Governmental Hospital | 131 | 23 | 0 | 0.998 | ||
| Month of ANC First | < 3> | 101 | 20 | 0.633 [0.343-1.168] | 1 | 1 |
| >3monthes | 101 | 10 | 0.983[0.315-3.069] | 0.977 | ||
| Number of ANC visit | 45352 | 28 | 3 | 1.176 [0.646-2.139] | 1 | 1 |
| 45447 | 156 | 23 | 0.114[0.011-1.204] | 0.071 | ||
| >7 | 18 | 4 | 0.567[0.126-2.551] | 0.459 | ||
| PIH | Yes | 116 | 27 | 10.465[2.922-37.474] | 0.00** | |
| No | 96 | 5 | ||||
| Membrane Status | Intact | 130 | 13 | 2.262 [1.061-4.822] | 1 | 1 |
| Ruptured | 84 | 19 | 3.577[1.198-10.682] | 0.022** | ||
| Duration of labor | <12> | 118 | 21 | 0.515 [0.296-0.897] | 1 | 1 |
| >12 hours | 35 | 11 | 3.324 [1.101-10.034] | 0.033** | ||
| NA | 61 | 0 | ||||
| Adverse fetal birth out come | ||||||
| Variables | Category | Adverse maternal birth outcome | COR (95%CI) | AOR (95%CI) | P- Value | |
| Yes | NO | |||||
| Marital Status of mother | Single | 17 | 2 | 2.916[0.900-9.455] | 1 | 1 |
| Married | 166 | 57 | 0 | 0.999 | ||
| Widowed | 2 | 2 | 0 | 0.999 | ||
| Prior Abortion | Yes | 29 | 3 | 1.107[0.547-2.242] | 1 | 1 |
| No | 156 | 50 | 0 | 0.999 | ||
| Gravidity | PG | 59 | 13 | 1.729[0.870-3.435] | 1 | 1 |
| MG | 126 | 48 | 0 | 0.999 | ||
| Parity | NP | 77 | 16 | 1.482 [1.042-2.109] | 1 | 1 |
| PP | 54 | 20 | 4.09E+08 | 0.999 | ||
| MP | 54 | 25 | 1.320 [0.588-2.963] | 0.5 | ||
| Place of ANC | H.C | 60 | 11 | 1.839 [1.299-2.606] | 1 | 1 |
| Private Hospital | 7 | 0 | 0.252 [0.098-0.649] | 0.004** | ||
| Governmental Hospital | 104 | 50 | 0 | 0.998 | ||
| Month of ANC First | < 3> | 85 | 36 | 1.061 | 1 | 1 |
| >3monthes | 86 | 25 | [0.650-1.730] | 1.403[0.69-2.856] | 0.355 | |
| Number of ANC visit | 45352 | 26 | 5 | 1.711 [1.026-2.851] | 1 | 1 |
| 45447 | 128 | 51 | 1.220[0.234-6.367] | 0.813 | ||
| >7 | 17 | 5 | 1.873[0.595-5.898] | 0.283 | ||
| Residence | Addis Ababa | 141 | 43 | 1.341[0.703-2.559] | 1 | 1 |
| Outside Addis Ababa | 44 | 18 | 0.343 [0.143-0.826] | 0.017** | ||
P less than 0.05, AOR, adjusted odds ratio; COR, crude odd ratio; CI, confidence interval; PROM, premature rupture of membranes; PIH, Pregnancy Induced Hypertension.
Discussion
The Finding of this study showed that 86.9% of the participants have adverse maternal outcome while 75.2% of the Participants have adverse fetal birth outcome. Preterm delivery (42.6%), C/S and Instrumental delivery (58.95%), Oligohydraminos and Polyhydraminos (5.7%), Low Birth weight (72.4%), Poor Apgar score (15.8%), Still birth (8.2%), Birth defect (0.8%), Admission to MICU and NICU (2.4% and 60.8% respectively) were accounted for adverse birth outcome. Among the Factors Presence of Pregnancy induced Hypertension, Membrane status and Duration of Labor were significantly associated with adverse maternal birth outcome while Place of ANC visit and Residence of the mother were significantly associated with adverse fetal birth outcome. The prevalence of adverse birth outcome of this study is higher when compared to study done in Hosanna (24.5%) and Gondar (32.6%) [26,27]. The reason for the difference in this finding was the type of participants of which all participants of the selected public hospitals of Addis Ababa were referral hospitals so majority of the cases were referrals from health centers and clinics. In this study mothers who had Pregnancy Induced Hypertension were 10 times more likely to have adverse maternal birth outcome when compared to mothers who do not have Hypertension. This is in line with the researches done in Dessie and Gondar [26]. The reason for this might be due to the fact that complications of hypertension during pregnancy can cause impaired placentation and Placental ischemia.
In the study Mothers who had ruptured membrane before the onset of Labor (Premature rupture of membrane (PROM)) were three times more likely to develop adverse maternal birth outcome as compared to mothers who had intact membrane before onset of labor. The finding is in agreement with a case control study done in western Ethiopia to assess adverse birth outcome [26]. The reason for this might be due to the fact premature rupture of membrane leads to Umbilical cord prolapse, Placental abruption and uterine contraction as amniotic fluid contains prostaglandin which in turn may result adverse birth outcome. Mothers who had ANC follow up in private hospitals were 0.75 times less likely to get adverse fetal birth outcome as compared with mothers who had ANC follow up in the three public hospitals and health centers. This may be attributed to the quality of care in the private hospital. This might be due to the fact that good counseling given during the ANC follow-up helps the mother to get information on diet, danger signs of pregnancy and pregnancy related complications. The result of the study is in agreement with the study done in Oromia region on adverse birth out come and associated factors among mothers who delivered in Bale Zone Hospital [20].
In this study Mothers who live outside Addis Ababa were unlikely to have adverse fetal outcome, this is different from the study which is done in Butajira hospitals that mothers who live in rural residence were nearly three times more likely to encounter adverse birth outcome as compared with those who lives in urban residence [20]. The possible cause for this difference is that most of the catchment Health centers of the three public hospitals are from Addis Ababa; only few are from neighboring Oromia region. So, the difference is because of most of the participants of the study are from Addis Ababa.
Strength and Limitation
Strength of the Study
- The Study has a comprehensible Operational definition of adverse birth outcome of twin’s pregnancy that operationalize adverse birth outcome as adverse maternal and adverse fetal birth outcome.
- The checklist used to assess was Pre tested in a similar setting and a necessary modification was made to minimize the difficulty during data collection.
Limitation of the study
- Since the data were secondary data some variables that couldn’t be found on the maternal chart were omitted from the Questionnaire.
- No temporal relationship is found in this Study.
Conclusion
Twin pregnancy is increasing worldwide as a result of an increment in artificial fertilization. Adverse birth outcome of Twins pregnancy is relatively higher when compared to similar studies conducted in Ethiopia. Preterm Labor (42.6%), C/S and Instrumental delivery (58.95%), Oligohydraminos+ Polyhydraminos (5.7%), and Maternal admission to MICU were identified as maternal outcome. Preterm neonate (42.6%), low birth weight (72.4%), Poor APGAR score (15.8%), still birth (8.2%), Birth defect (0.8%) was identified as fetal outcome.
Membrane Status (PROM), Duration of Labor, Pregnancy Induced Hypertension was significantly associated with maternal outcome and Place of ANC visit and Residence of the mother were significantly associated with Fetal outcome.
Conclusion
Twin pregnancy is increasing worldwide as a result of an increment in artificial fertilization. Adverse birth outcome of Twins pregnancy is relatively higher when compared to similar studies conducted in Ethiopia. Preterm Labor (42.6%), C/S and Instrumental delivery (58.95%), Oligohydraminos+ Polyhydraminos (5.7%), and Maternal admission to MICU were identified as maternal outcome. Preterm neonate (42.6%), low birth weight (72.4%), Poor APGAR score (15.8%), still birth (8.2%), Birth defect (0.8%) was identified as fetal outcome.
Membrane Status (PROM), Duration of Labor, Pregnancy Induced Hypertension was significantly associated with maternal outcome and Place of ANC visit and Residence of the mother were significantly associated with Fetal outcome.
Abbreviations
AA: Addis Ababa; APH: Ante partum Hemorrhage; ANC: Ante natal care;
CS: Caesarean section;
CI: Confidence Interval;
EDHS: Ethiopian Demographic and Health survey;
ETB: Ethiopian Birr; FHB: Fetal heart beat;
GMH: Gandhi Memorial Hospital;
LBW: Low birth weight; OR: odds ratio;
PIH: Pregnancy induced Hypertension;
PROM: Premature rapture of membrane;
SVD: Spontaneous vertex delivery; WHO: World Health Organization
ART: Assisted Reproductive Technology; IVF: In vitro fertilization
Declarations
Ethical approval and consent to participate: The ethical clearance was obtained from Institutional Review Board of KEA-MED University college and official letters was submitted to each respective health facility. After explaining the objectives of the study, informed written consent was obtained from all mothers, and anonymity and confidentiality of the data were kept. Respondents have the right not to participate or withdraw from the study at any stage, and all study methods were performed in accordance with the Declaration of Helsinki.
Consent for publication: Not applicable.
Availability of data and materials: The data used to support the findings of this study are available from the corresponding author upon request
Competing interests: The authors declare that they have no conflicts of interest
Funding: Not applicable.
Author contributions
C.G; Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, writing – original draft A.L; Conceptualization, Formal analysis, Methodology, Resources, Software, Visualization, Writing and original draft D, C, Conceptualization, Formal analysis, Methodology, Software, Supervision, Writing, review & editing.
Acknowledgements: The authors would like to express their gratitude to respective health facility, data collectors, supervisors and study participants for their diligence and dedication in the collecting and inputting high quality data used in the study.
References
- Abebaw N, Abdu M, Girma N. (2021). Assessments of Birth Outcome of Twin Delivery and Associated Factors among Newborns in Dessie Referral Hospital, Dessie, Ethiopia, 2019. Vol. 2021, Obstetrics and Gynecology International. Hindawi Limited.
Publisher | Google Scholor - Tilahun T. (2015). Incidence and Risk Factors of Twin Pregnancy at Jimma University Specialized Hospital, Southwest Ethiopia. Epidemiol Open Access, 5(02).
Publisher | Google Scholor - Smits J, Monden C. (2011). Twinning across the developing world. PLoS One, 6(9):8-10.
Publisher | Google Scholor - Santana DS, Surita FG, Cecatti JG. (2018). Multiple pregnancy: Epidemiology and association with maternal and perinatal morbidity. Rev Bras Ginecol e Obstet, 40(9):554-562.
Publisher | Google Scholor - K. S, M. H. JA. (2019). Twin pregnancy, the study of maternal and perinatal outcome: what being a twin is like? Int J Reprod Contraception, Obstet Gynecol, 8(11):4457.
Publisher | Google Scholor - Rezavand N, Veisi F, Malek-khosravi S, Zangeneh M, Kohzadi M. (2014). Assessment of frequency of twin pregnancy and neonatal outcome in deliveries of Mo’tazedi Hospital, Kermanshah in 2004-2007. J Obstet Gynecol India, 64(1):19-22.
Publisher | Google Scholor - Bortolus R, Parazzini F, Chatenoud L, Benzi G, Bianchi MM, Marini A. (1999). The epidemiology of multiple births. Hum Reprod Update, 5(2):179-187.
Publisher | Google Scholor - Minakami H, Sayama M, Honma Y, Matsubara S, Koike T, Sato I, et al. (1998). Lower risks of adverse outcome in twins conceived by artificial reproductive techniques compared with spontaneously conceived twins. Hum Reprod, 13(7):2005-2008.
Publisher | Google Scholor - Ayza A, Tilahun T, Bedada D. (2019). Magnitude and Obstetric Complications of Twin Deliveries at Nekemte Referral Hospital, Western Ethiopia: Facility-based Case Control Study. Biol Med, 11(1).
Publisher | Google Scholor - Esteves-Pereira AP, da Cunha AJLA, Nakamura-Pereira M, Moreira ME, Domingues RM soares madeira, Viellas EF, et al. (2021). Twin pregnancy and perinatal outcomes: Data from ‘Birth in Brazil Study.’ PLoS One, 16(1).
Publisher | Google Scholor - Dudenhausen JW, Maier RF. (2010). Perinatale probleme von mehrlingen. Dtsch Arztebl, 107(38):663-668.
Publisher | Google Scholor - Akaba GO, Agida TE, Onafowokan O, Offiong RA, Adewole ND. (2013). Review of twin pregnancies in a tertiary hospital in Abuja, Nigeria. J Heal Popul Nutr, 31(2):272-277.
Publisher | Google Scholor - Santana DS, Silveira C, Costa ML, Souza RT, Surita FG, Souza JP, et al. (2018). Perinatal outcomes in twin pregnancies complicated by maternal morbidity: Evidence from the WHO Multicountry Survey on Maternal and Newborn Health. BMC Pregnancy Childbirth, 18(1).
Publisher | Google Scholor - Fekadu GA, Getahun FA, Kidanie SA. (2018). Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: Further analysis of the 2016 Demographic and Health Survey. bioRxiv.
Publisher | Google Scholor - Hoffmann E, Oldenburg A, Rode L, Tabor A, Rasmussen S, Skibsted L. (2012). Twin births: Cesarean section or vaginal delivery? Acta Obstet Gynecol Scand, 91(4):463-469.
Publisher | Google Scholor - Obiechina NJ, Okolie VE, Eleje GU, Okechukwu ZC, Anemeje OA. (2011). Twin versus singleton pregnancies: The incidence, pregnancy complications, and obstetric outcomes in a Nigerian tertiary hospital. Int J Womens Health, 3(1):227-230.
Publisher | Google Scholor - Vogel JP, Torloni MR, Seuc A, Betrán AP, Widmer M, Souza JP, et al. (2013). Maternal and Perinatal Outcomes of Twin Pregnancy in 23 Low- and Middle-Income Countries. PLoS One, 8(8).
Publisher | Google Scholor - Tsegaye B, Kassa A. (2018). Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health, 15(1):1-11.
Publisher | Google Scholor - Haftu A. (2017). Assessment of Magnitude and Associated Factors of Adverse Birth Outcomes among Deliveries at Suhul Hospital Shire, Tigray, Ethiopia from September, 2015 to February, 2016. Biomed J Sci Tech Res, 1(7).
Publisher | Google Scholor - Degno S, Lencha B, Aman R, Atlaw D, Mekonnen A, Woldeyohannes D, et al. (2021). Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. J Int Med Res, 49(5).
Publisher | Google Scholor - Abadiga M, Mosisa G, Tsegaye R, Oluma A, Abdisa E, Bekele T. (2022). Determinants of adverse birth outcomes among women delivered in public hospitals of Ethiopia, 1-17.
Publisher | Google Scholor - Abdo RA. (2019). Prevalence and Associated Factors of Adverse Birth Outcome Among Deliveries at Butajira Hospital, Southern Ethiopia. J Gynecol Womens Heal, 15(4):1-8.
Publisher | Google Scholor - Abebaw N, Abdu M, Girma N. (2021). Assessments of Birth Outcome of Twin Delivery and Associated Factors among Newborns in Dessie Referral Hospital, Dessie, Ethiopia, 2019. Obstet Gynecol Int.
Publisher | Google Scholor - Indra, N. U, Bendigeri M. (2017). A study on clinical outcome of obstructed labour. Int J Reprod Contraception, Obstet Gynecol, 6(2):439.
Publisher | Google Scholor - Eshetu B, Sintayehu Y, Mekonnen B, Daba W. (2019). Birth Outcomes among Diabetic Mothers Who Delivered in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Adv Med, 1-6.
Publisher | Google Scholor - Adane A. (2014). adverse birth outcomes among deliveries in Gondar university hospital, 1-8.
Publisher | Google Scholor - RA A, TB E. (2016). Prevalence and associated Factors of Adverse Birth Outcomes among Women Attended Maternity Ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia. J Women’s Heal Care, 5(4):3-7.
Publisher | Google Scholor