case report article
Bilateral Pleural Chylothorax from A Blunt Chest Trauma
- Skender Buci *
- G. Bushi
- E. Markeci
Surgery Service, University Hospital of Trauma, Tirana, Albania.
*Corresponding Author: Skender Buci,Surgery Service, University Hospital of Trauma, Tirana, Albania.
Citation: S. Buci, Gj. Bushi, E. Markeci. (2023). Bilateral pleural chylothorax from a blunt chest trauma. Journal of Surgical Case Reports and Reviews. BRS Publishers. 2(2); DOI: 10.59657/2993-1126.brs.23.016
Copyright: 2023 Skender Buci, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 11, 2023 | Accepted: July 24, 2023 | Published: August 21, 2023
Abstract
Introduction: Bilateral traumatic chylothorax is a very rare condition. Approximately80% of chylothorax are unilateral and usually 2/3 of cases on the right side [1]. The chyle leakage shows a milky white appearance, inexhaustible, in a consideration amount.
Purpose: To report the management of bilateral traumatic chylothorax as a very rare condition.
Material and methods: We present a patient with bilateral pleural chylothorax from a blunt chest trauma which is combined with a vertebral thoracal fracture of Th8, Th10.We present the diagnostic basis, treatment and evolution of chilies leakage.
Results: A 36 years old man involved in a car crash. He was hospitalized with a diagnose such as right pleural effusion and thoracal vertebral fractures of the Th8, Th10.2 days after trauma the scan examination showed a large amount of effusion in the right hemithorax and minimal effusion in the left hemithorax. From the drainage tube in the right pleural cavity there was a flow of about 1000ml with a milky appearance. The biochemical analyses of the pleural effusion showed the presence of triglycerides with more than 1.24mmol /l and the cholesterol level with less than 5.18mmol/l which support the diagnosis of chylothorax. Initial treatment was conservative. A zero nutritional regimen was implemented for the first 10 days, being replaced by total parenteral nutrition such as plasma, albumin, electrolytes, vitamins. After that we passed to a fat-free nutritional diet. In the scan examination 6 days after the trauma, there was an increase in the amount of pleural effusion on the left side. A chest tube was performed from which there was 700 ml leakage, which had the appearance of chyle. The biochemical tests confirmed the diagnose of chylothorax. The chest tube of the left pleural cavity was removed after 5 days. The chyle leakage from the right pleural cavity has continued for about 3 weeks in a quantity ranging from 150-300 ml in 24 hours. After this period, approximately for 1 week the chyle leakage was in an amount of less than 1000ml in 24 hours. In the 5th week, the chest tube was removed, since the leaks were reduced to about 20-30 ml in 24 hours. The patient left the hospital after 30 days. The patient was completely recovered.
Conclusions: The case was managed conservatively, based on a bilateral pleural drainage and a diet without fats, which proved to be successful.
Keywords: chylothorax pleural; fluid analysis triglycerides malignancy conservative management
Introduction
Bilateral traumatic chylothorax is a very rare condition, often with potentially serious consequences. Chylothorax is an effusion of chyle in both pleural spaces, as a result of a both pleural spaces, as a result of a damage to the thoracic duct. This lymph is rich in lipids 85% - 92%, triglycerides 6-12 %, phospholipids 1-3 %, cholesterol, electrolytes, proteins, fat-soluble vitamins, lymphocytes and immunoglobulins. The thoracic duct brings in systemic circulation up to 2400 ml of lymph in 24 hours. The initial management of chylothorax is conservative with low-fat diet and chyle drainage through a thoracostomy tube. Conservative management of chylothorax is successful in most cases, it turned out to be the same in our case [2,3,4,5].
Case Presentation
E.K. 36-years old man involved in a car crash. He is given first aid at the scene and brought to SUT for further evolution. After the initial assessment of the clinical condition, radiological and biochemical examinations were performed immediately. The patient is hospitalized with right pleural effusion and vertebral compressive fractures of Th8, Th10.
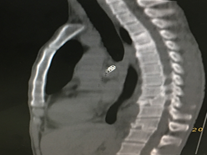
Figure1: Fracture compressive Th8, Th10.
Two days after the trauma, the damage was re-evaluated with a thoracic scanner and this examination revealed a large amount of right pleural effusion and minimal left pleural one. It was decided that it is necessary to remove the right pleural effusion.
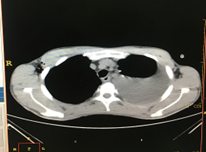
Figure 2: Bilateral pleural effusion (minimal on the left).
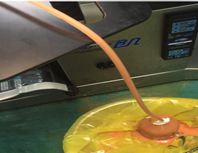
Figure 3: The view of the pleural effusion.
Biochemical analysis of the pleural effusion has confirmed the presence of triglycerides of more than 1,24 mmol/l and a cholesterol level of less than 5,18mmol/l. At first the patient was treated conservatively, albumin, then he started eating a fat-free diet. Evaluation with CT, 6 days after the trauma has confirmed an increase in the amount of the left pleural effusion.
Figure 4: The left pleural effusion.
A thoracostomy tube is placed on the left pleural cavity from which chyle flowed about 700 ml. After 5 days, the tube was removed as flow of chyle was exhausted. From the right pleural cavity, chyle persisted for about 3 weeks, in an amount that varied from 150-300 ml in 24 hours. After this period, for about a week, the flow was in an amount of at least 100 ml in 24 hours. On the 5th week, the leaks are reduced to about 20-30 ml ne 24 hours at this time, the right pleural drainage tube was removed. The patient leaves the hospital fully recovered on the 30th day. There was no recurrence of chyle leakage.
Discussion
Chylothorax is caused by the damage of the thoracic duct along its path through the posterior mediastinum, resulting in drainage of the chyle into one or both pleural cavities. Chylothorax is a rare complication in thoracic surgery and chest trauma which can lead to a serious illness and can even be fatal. It is essential to be alert for chylothorax in a blunt chest trauma which is combined with a vertebral thoracic fracture of 8Th,10Th, a cervico-thora cal or rétropéritonéal intervention. It Is confirme by the analyses of pleural effusion [6-8]. Traumatic chylothorax usually appears with a latent period of two to ten days, but up to 25 days have been described. Approximately, it appears in an average of 7 days [9]. In the blunt chest trauma, the most common place of damage to the thoracic duct is in the area of the 9Th and 10 Th. thoracic vertebrae [9]. In our case, a fracture of the 8Th and 10Th thoracic vertebrae was found. Van Pernis concluded that the thoracic duct is a duplicated structure from Th12 to Th8 in the 40% of the patients [10]. The diagnosis of chylothorax is mainly based on the values of triglycerides and cholesterol which are found in the pleural effusion. The diagnosis is determined by chest CT and by the presence of triglycerides in the biochemical analyses of the pleural effusion. The presence of triglycerides with more than 1,24 mmol/l and cholesterol with less than 5,18 mmol / l in the pleural effusion support the diagnosis of chylothorax [7]. Lymphangiography and lymphoscintigraphy which are rarely performed, are useful to evaluate the location of the leak, to define the permeability of the thoracic duct, and to differentiate a partial or complete rupture of the duct [11]. Lymphoscintigraphy has the advantage of being fast minimal invasive and has few negative effects. The differential diagnosis of chylothorax mainly includes pseudo chylothorax and empyema. Pseudo chylothorax is characterised by the presence of a high amount of cholesterol (>5,18mmol /l) and a triglycerides level of less than 1,24mmol/lather most common cause of pseudo chylothorax are chronic exudates (tubercular pleurisy) [6,12]. Management strategies for chylothorax have undergone a significant innovation since the time of Rd. Bartlett’s description in the 17 the century. [13-16]. If the clinical condition allow initially conservative treatment should be preferred even in a chylothorax as a result of a chest trauma [8,13,[17]. Conservative treatment is based on pleural drainage and a fat-free diet and appropriate etiological management. In case of failure, the closing of the thoracic lymphatic duct with a surgical technique or with interventional radiology should be considered. In our case, conservative treatment was performed which consist in total parenteral nutrition and bilateral pleural drainage. This tactic has been successful according to some reports, including in our case [18-21]. In our patient, the chyle leakage was exhausted in the 5 th week after a conservative treatment only. The rate of success of conservative treatment is very variable and depends on the main causes, however, a flow more than 1000-1500 ml/24 hours is impossible to be resolve without a further intervention [3]. Chemical pleurodesis can be used as an alternative if it is necessary [12]. Surgical treatment has been, for many years, the only option after the failure of conservative treatment. The ligation of the right thoracic duct (between the 8Th and 10Th) is the most commonly used as a surgical treatment, especially in the traumatic chylothorax. In general, the main difficulty is the identification of the thoracic duct and its outflow. The swallowing of the butter or cream, as well as injecting of the blue methylene before the intervention can help to localise the leakage. Up to 50% of the patients may die from complications of untreated chylothorax [12], [13].
Conclusion
Bilateral traumatic chylothorax remains a very rare complication of chest trauma. The initial treatment is conservative which consist of a drainage thoracostomy tube and a free-fat diet. For many years surgical treatment has been the only option after conservative treatment.
References
- Maldonado F, Cartin-Ceba R, Hawkins FJ, et al. (2010). Medical and surgical management of chylothorax and associated outcomes. Am J Med Sci, 339(4):314-318.
Publisher | Google Scholor - M. Beghetti, G. La Scala, D. Belli, et al. (2000). Etiology and management of pediatric chylothorax J Pediatrics, 136(5):653-658.
Publisher | Google Scholor - M. Soto-Martinez, J. (2009). MassieChylothorax: diagnosis and management in children Paediatr Respir Rev, 10(4):199-207.
Publisher | Google Scholor - J.D. (2014). TutorChylothorax in infants and children Pediatrics, 133(4):722-733
Publisher | Google Scholor - N. Karaoğlanoğlu, A. Eroğlu, A. (1999). BaşoğluIsolated chylothorax after penetrating traumaActa Chir Hung, 38(1):67-69.
Publisher | Google Scholor - EE McGrath Z Blades PB.Anderson Chylothorax. (2010). Aetiology, diagnosis and therapeutic options. Respir Med, 104:1-8.
Publisher | Google Scholor - HH Schild CP Strassburg AWelz J.Kalff. (2013). Treatment options in patients with chylothorax.Deutsches Arzteblatt International, 110:819-826.
Publisher | Google Scholor - DX Yu XX Ma Q Wang Y Zhang CF.Li. (2013). Morphological changes of the thoracic duct and accessory lymphatic channels in patients with chylothorax: Detection with unenhanced magnetic resonance imaging. Eur Radiol, (23).
Publisher | Google Scholor - P.S. (1958). Thorne Traumatic chylothorax Tubercle, 39(1):29-34.
Publisher | Google Scholor - Van Pernis PA. (1949). Variation of the thoracic duct. Surgery, 26:308-312.
Publisher | Google Scholor - Bender B, Murthy V, Chamberlain RS. (2015). The changing management of chylothorax in the modern era. Eur J Cardiothorac Surg epub ahead of print.
Publisher | Google Scholor - Schild HH,Strassburg CP,Welz A,Kalff J.(2013). Treatment options in patients with chylotorax. Deutsches Arzteblatt International, 110:819-826.
Publisher | Google Scholor - Schild HH, Pieper C. (2019). [Chylothorax: Current Therapeutic Options]. Zentralbl Chir.
Publisher | Google Scholor - Zhang C, Xi MY, Zeng J, Li Y, Yu C. (2019). Prognostic Impact of Postoperative Complications on Overall Survival in 287 Patients with Oral Cancer: A Retrospective Single-Institution Study. J. Oral Maxillofac. Surg.
Publisher | Google Scholor - Iio K, Soneda K, Shimotakahara A, Hataya H, Kono T. (2019). Effective method of evaluating infantile chylothorax. Pediatr Int, 61(2):203-205.
Publisher | Google Scholor - Hayashi K, Hanaoka J, Ohshio Y, Igarashi T. Chylothorax secondary to a pleuroperitoneal communication and chylous ascites after pancreatic.
Publisher | Google Scholor - de Beer HG, Mol MJ, Janssen JP. (2000). Chylothorax.Neth J Med, 56:25-31.
Publisher | Google Scholor - M. Beghetti, G. La Scala, D. Belli, et al. (2000). Etiology and management of pediatric chylothorax J Pediatrics, 136(5):653-658.
Publisher | Google Scholor - M. Soto-Martinez, J. (2009). Massie Chylothorax: diagnosis and management in children Paediatr Respir Rev, 10(4):199-207.
Publisher | Google Scholor - J.D. (2014). Tutor Chylothorax in infants and children Pediatrics, 133(4):722-733.
Publisher | Google Scholor - N. Karaoğlanoğlu, A. Eroğlu, A. (1999). BaşoğluIsolated chylothorax after penetrating trauma Acta Chir Hung, 38(1):67-66.
Publisher | Google Scholor