Research Article
Atypical Radiological Findings in Colloid Cyst of Third Ventricle- Rare Findings in Rare Tumor
- Rajat Verma *
Department of Neurosurgery, Kings George Medical University, Uttar Pradesh, Lucknow, India.
*Corresponding Author: Rajat Verma, Department of Neurosurgery, Kings George Medical University, Uttar Pradesh, Lucknow, India.
Citation: V. Rajat. (2024). Atypical Radiological Findings in Colloid Cyst of Third Ventricle- Rare Findings in Rare Tumor. Scientific Research and Reports, BioRes Scientia Publishers. 1(4):1-8. DOI: 10.59657/2996-8550.brs.24.020
Copyright: © 2024 Rajat Verma, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 26, 2024 | Accepted: September 06, 2024 | Published: September 13, 2024
Abstract
Introduction: Colloid cysts of the third ventricle, characterized by their rarity, demand an in-depth understanding of their imaging characteristics to ensure accurate diagnosis and optimal surgical management. With an annual incidence of merely 3 cases per million individuals, these tumors represent a mere 2% of primary brain tumors.
Materials and Methods: This retrospective study involved a meticulous analysis of 47 patients diagnosed with colloid cysts at PGIMER, Chandigarh, over the past 10 years. Surgical intervention, through either endoscopic or microsurgical excision, was performed in all cases. The study focused on evaluating preoperative imaging modalities, including non-contrast computed tomography (NCCT) head and magnetic resonance imaging (MRI).
Results: The analysis revealed that the size of colloid cysts in 91.5% of cases fell within the range of 1 to 3 cm, with a mean diameter of 17.55±8.32 mm. Notably, three cases presented with giant cysts exceeding 3 cm in diameter. On NCCT head, the cysts exhibited hyper density in 85.11% of cases, hypodensity in 4.25%, and is density in 10.64%. T1-weighted MRI sequences demonstrated hyperintensity in 42.55% of cases, hypo intensity in 31.92%, and is intensity in 25.53%. T2-weighted sequences revealed hyperintensity in 57.45%, hypo intensity in 38.30%, and is intensity in 4.25% of cases. Peripheral contrast enhancement was observed in 8.51% of cysts, and two cases exhibited intracity hemorrhage, one of which involved a giant cyst. Furthermore, one cyst presented with an intramural nodule.
Conclusion: This study sheds light on atypical imaging findings associated with colloid cysts, encompassing giant cysts, peripheral contrast enhancement, intracity hemorrhage, and intramural nodules. A nuanced understanding of these variations is imperative for precise diagnosis and meticulous surgical planning in the management of colloid cysts of the third ventricle.
Keywords: colloid cyst; imaging; atypical; radiology; rare brain tumours
Introduction
A colloid cyst, characterized as a benign, epithelial-lined structure containing mucin, typically resides in the anterosuperior part of the third ventricle roof, just posterior to the foramen of Monro. These rare intracranial masses occur at a rate of 3 individuals per million per year, constituting approximately 2% (with a range of 0.5 to 3%) of all primary brain tumors and 15 to 20% of all intraventricular masses [1,2-5]. Predominantly identified in the 30-60 years age group2, with a peak incidence in middle age (30-50 years), these cysts are seldom encountered in the pediatric age group, being particularly rare in infancy and childhood [6,7]. A mere 37 cases had been documented until 1994 [8]. Colloid cysts are either incidentally discovered in asymptomatic patients during imaging or present with features indicative of raised intracranial pressure in symptomatic patients. In rare instances, they have been associated with sudden death [9]. Typically ranging from 1 to 3 cm in size, giant colloid cysts (>3cm) are infrequently observed. These cysts are characterized by a mixed array of goblet and epithelial cells that secrete proteinaceous mucinous material, influencing the imaging characteristics of the cyst. Additionally, cyst cavities may contain blood degradation products and cholesterol crystals. Histologically, the fibrous walls are lined by simple or pseudostratified epithelial cells, which may be flattened cuboidal or low columnar, resting on a thin capsule of collagen and fibroblasts [10]. Rarely, the cyst wall may exhibit thickening, vascularity, and organization into an organized hematoma of varying ages. The contents of the cyst typically appear greenish and vary in viscosity.
On all modalities, a colloid cyst appears as a rounded, well-demarcated lesion at the foramen of Monro, ranging from a few millimeters to 3-4 cm [5]. Magnetic Resonance Imaging (MRI) surpasses CT in fully characterizing the lesion. On CT scans, colloid cysts manifest as well-delineated, rounded lesions on the roof of the third ventricle, usually unilocular and hyperdense, with is dense and hypodense cysts being uncommon [4]. On MRI, a colloid cyst typically appears hyperintense on T1 and isointense on T2, often exhibiting peripheral rim enhancement. T1-weighted sequences may display variable signals, with approximately 50% showing a high signal, while the remainder are hypointense or isointense to adjacent brain tissue [11,12]. Gadolinium-enhanced T1 sequences may rarely demonstrate thin rim enhancement, typically representing the enhancement of adjacent and stretched septal veins [5]. On T2 sequences, colloid cysts exhibit variability, with mostly low T2/T2* signals related to the thick "motor oil" consistency of the fluid [11,13,14]. Some may display low central T2 and high peripheral T2 signals [13]. Additional findings from MRI include ventricle size, the presence of cavum septum pellucidum et verge, abnormal vascular structures (DVA), and the location of internal cerebral veins. Hemorrhage within the cyst and intramural nodules are uncommon occurrences. In our study, we present four cases of peripheral contrast enhancement, three cases of giant colloid cysts, two instances of intracity hemorrhage, and one case of an intramural nodule, contributing valuable insights into the diverse manifestations of this rare pathology.
Materials and methods
The study encompassed 47 patients who were diagnosed with and underwent surgical intervention for colloid cysts of the third ventricle within the past 10 years at the Department of Neurosurgery, PGIMER Chandigarh. Informed written consent was diligently obtained from all subjects after a detailed explanation of the study. Pre-operative data and intraoperative details were meticulously extracted from patient case sheets and cross-verified with the patients' medical histories. Postoperatively, patients were systematically evaluated on an outpatient basis with the use of questionnaires focusing on symptomatology and quality of life. A minimum follow-up period of 6 months was adhered to. Pre- and post-operative imaging data were scrutinized comprehensively, and the radiological outcomes of the surgical procedures were analyzed by comparing the pre- and post-operative images. Here in this article, we have meticulously studied the atypical radiological presentations of these patients individually.
Results
Of the 47 patients, a notable subset of 9 individuals exhibited atypical radiological findings in their imaging studies. Among these, 4 patients displayed peripheral contrast enhancement in contrast-enhanced MRI (CE MRI), indicating a distinctive feature in the postoperative imaging. Three patients presented with colloid cysts exceeding 3 cm in size, deviating from the typical range. Additionally, 2 patients manifested evidence of hemorrhage within the colloid cyst, while 1 patient exhibited the presence of an intramural nodule. Furthermore, a giant cyst within this subset exhibited intracity hemorrhage. We have summarized these findings in group based on individual atypical radiological finding. Only 4 out of 47 patients showed peripheral contrast enhancement (table no. 1). This suggests that colloid cyst usually do not show contrast uptake, moreover presence of only peripheral uptake may be due to capsule vascularity and most of times confused with stretched septal veins. All 4 patients were males.
Table 1: showing comparison of relevent variables between 4 patients showing peripheral contrast enhancement.
| Patient name | A | B | C | D |
| Age in years | 29 | 50 | 33 | 33 |
| Approach | Endoscopy | Endoscopy | Microsurgery | Microsurgery |
| NCCT head density | Hyperdense | Hyperdense | Hyperdense | Isodose |
| T1 MRI intensity | Isointense | Isointense | Isointense | Hypointense |
| T2 MRI intensity | Hyperintense | Hyperintense | Hyperintense | Hyperintense |
| Cyst size (mm) | 15 | 28 | 10 | 22 |
| Follow up (months) | 20 | 36 | 11 | 32 |
| Ventriculomegaly (post op) | Absent | Absent | Absent | Absent |
| Residual lesion | Absent | Present | Absent | Absent |
| OT time (mins) | 120 | 180 | 120 | 240 |
| Hospital stays (days) | 2 | 4 | 3 | 4 |
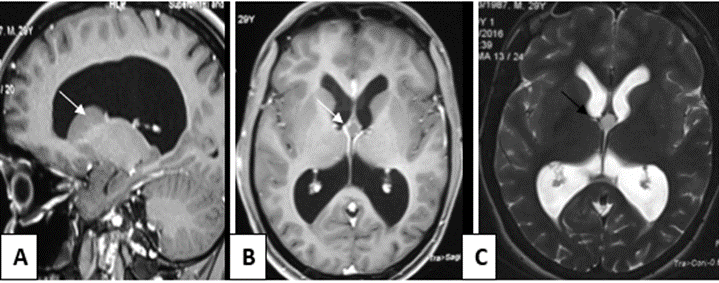
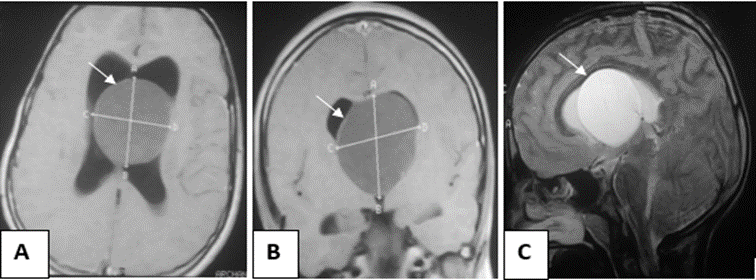
Patient A, 29 yr. male presented with complains of headache, nausea & vomiting. Papilledema was present on examination. On imaging cyst was hyperdense on CT, isointense on T1 and hyperintense on T2 weighted MRI (Figure1). Cyst size was 15mm. and ventriculomegaly was present. Gross Total Endoscopic resection of the cyst was done. Follow up at 20 months showed complete resolution of all symptoms without any ventriculomegaly and residual lesion.
Figure 1: T1 weighted precontrast sagittal(A), postcontrast axial (B) & T2 weighted axial (C) MR images of colloid cyst (arrows) of third ventricle of patient A.
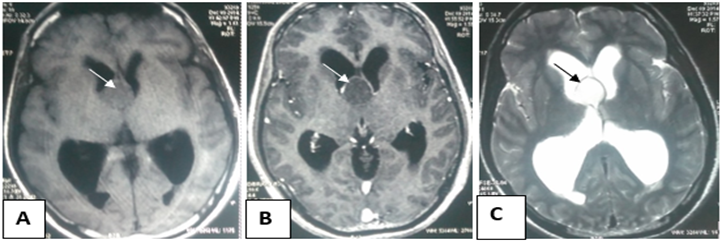
Patient B, 50 yr. male presented with complains of headache, cognitive defects, gait disturbances & altered sensorium. Papilledema was present. On imaging cyst was hyperdense on CT, isointense on T1 and hyperintense on T2 weighted MRI (Figure no. 2). Cyst size was 28mm. and ventriculomegaly was present. Subtotal endoscopic resection of the cyst was done. Follow up at 36 months showed complete resolution of all symptoms without any ventriculomegaly but residual lesion was present.
Figure 2: T1 weighted precontrast (A), postcontrast (B) & T2 weighted (C) axial MR images of colloid cyst (arrows) of third ventricle of patient B.
Patient C, 33 yr. male presented with complains of headache, nausea & vomiting. On imaging cyst was hyperdense on CT, isointense on T1 and hyperintense on T2 weighted MRI (Figure no. 3). Cyst size was 10mm. and ventriculomegaly was present. Gross Total Microsurgical resection of the cyst was done. Follow up at 11 months showed complete resolution of all symptoms without any ventriculomegaly and residual lesion.
Figure 3: T1 weighted precontrast (A), postcontrast (B) & T2 weighted (C) axial MR images of colloid cyst (arrows) of third ventricle of patient C.
Patient D, 33 yr. male presented with complains of headache, nausea, vomiting, cognitive defects, gait disturbances & altered sensorium. Papilledema was present. On imaging cyst was isodense on CT, hypointense on T1 and hyperintense on T2 weighted MRI (Figure no. 4). Cyst size was 22mm. and ventriculomegaly was present. Patient required VP shunt before surgery to relieve hydrocephalus. Gross Total Microsurgical resection of the cyst was done. Follow up at 32 months showed complete resolution of all symptoms without any ventriculomegaly and residual lesion.
Figure 4: T1 weighted precontrast (A), postcontrast (B) & T2 weighted (C) axial MR images of colloid cyst (arrows) of third ventricle of patient D.
Table 2: showing comparison of relevent variables between 3 giant cyst patients.
| Patient name | E | F | G |
| Age in years | 12 | 26 | 38 |
| Approach | Endoscopy | Endoscopy | Microsurgery |
| NCCT head density | Hyperdense | Hypodense | Hyperdense |
| T1 MRI intensity | Hypointense | Hypointense | Hyperintense |
| T2 MRI intensity | Hyperintense | Hyperintense | Hypointense |
| Cyst size (mm) | 57 | 35 | 32 |
| Follow up (months) | 36 | 13 | 49 |
| Ventriculomegaly (post op) | Absent | Absent | Absent |
| Residual lesion | Absent | Absent | Present |
| OT time (mins) | 180 | 150 | 300 |
| Hospital stays (days) | 6 | 3 | 3 |
3 out of 47 (table no. 2) patients had giant colloid cysts (cyst diameter >30 mm.).
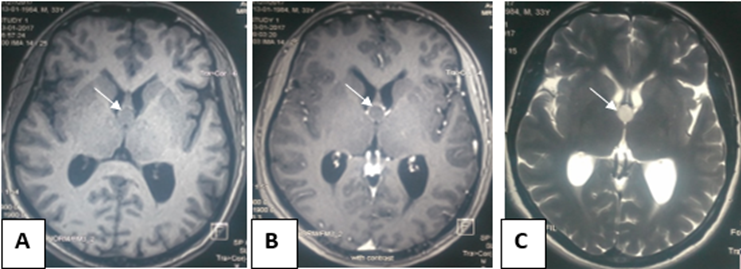
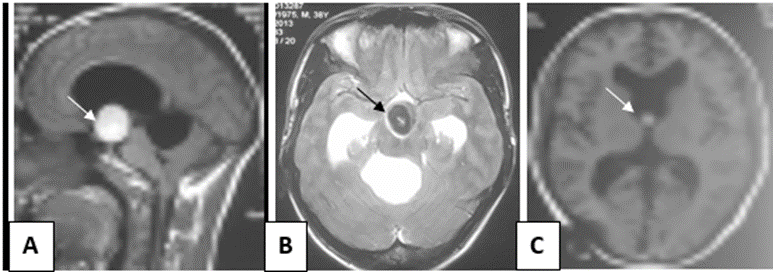
Patient E, 12 yr. male presented with complains of headache, nausea, vomiting. Bilateral papilledema was present on eye examination. On imaging cyst was hyperdense on CT, hypointense on T1 and hyperintense on T2 weighted MRI (Figure no. 5). Cyst size was 57mm. and ventriculomegaly was present. Gross Total Endoscopic resection of the cyst was done. Follow up at 36 months showed complete resolution of all symptoms without any ventriculomegaly and residual lesion.
Figure 5: T1 weighted axial (A), coronal (B) & T2 weighted sagittal (C) MR images of giant colloid cyst (arrows) of third ventricle (maximum diameter 57mm.) in patient E.
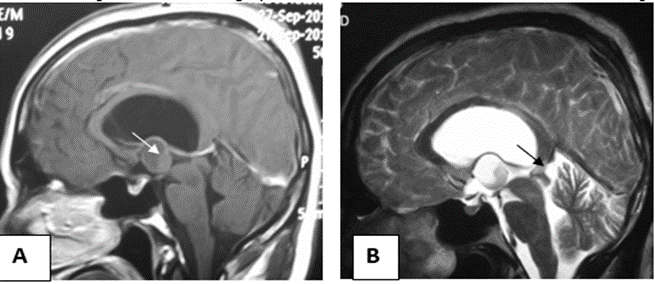
Patient F, 26 yr. male presented with complains of headache and visual disturbances. Bilateral papilledema was present on eye examination. Visual acuity was FC2 in both eyes. Planter reflex was absent. On imaging cyst was hypodense on CT, hypointense on T1 and hyperintense on T2 weighted MRI. Cyst size was 35mm. and ventriculomegaly was present. Endoscopic resection of the cyst was done. Follow up at 13 months showed complete resolution of all symptoms except visual disturbances. Papilledema was absent on follow up. Visual acuity was 6/9 in both eyes. Ventriculomegaly and residual lesion were absent on follow up imaging. Mr G, 38 yr. male presented with complains of headache, nausea, vomiting. Bilateral papilledema was present on eye examination. On imaging cyst was hyperdense on CT, hyperintense on T1 and hypointense on T2 weighted MRI (Figure no. 6). Cyst size was 32mm, intracity hemorrhage & ventriculomegaly were present on MR imaging. Hemorrhage appeared bright on T1 and dark on T2 showing early subacute duration (4-7 days) after bleeding. Patient required VP shunt before surgery to relieve hydrocephalus. Microsurgical resection of the cyst was done. Follow up at 49 months showed complete resolution of most of the symptoms without any ventriculomegaly. Patient had poor cognitive outcome after surgery as he developed subjective memory disturbances after microsurgery. Objective assessment with PGIMER recent memory scale revealed a score of 5/5 but the patient subjectively complained of forgetting events of recent past. Residual lesion was present on follow up imaging.
Figure 6: T1 weighted sagittal (A) & T2 weighted axial(B) MR images showing intracystic hemorrhage within the giant colloid cyst (arrows) of third ventricle in patient G. Follow up T1 weighted axial MR image (C) showing residual lesion in same patient.
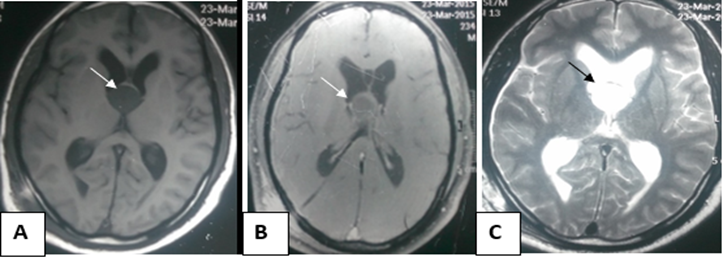
Patient H, 50 yr. male presented with complains of headache, nausea and vomiting. Papilledema was present on fundus examination. On imaging cyst was hyperdense on CT, hypointense on T1 and hyperintense on T2 weighted MRI (Figure no. 7). Blood within the cyst appeared as ill defined, heterogenous content within the cyst with variable intensity in different areas (due to the fact that different areas of clot are in different stages of degeneration) aligning towards the most dependent part of cyst (posterior wall in supine position). Hemorrhage present within the cyst was bright on T1 and dark on T2 showing early subacute phase of blood degeneration. Cyst size was 22mm. and ventriculomegaly was present. Endoscopic resection of the cyst was done. Follow up at 50 months showed complete resolution of all symptoms. Papilledema was absent on follow up. Ventriculomegaly and residual lesion were absent on follow up imaging.
Figure 7: T1 (A) & T2 (B) weighted sagittal MR images showing hemorrhage (arrows) within the colloid cyst of third ventricle in patient H. Note that the blood is hyperintense on T1 and hypointense on T2 suggesting early subacute period (4-7 days) after bleeding event. Blood is aligned more towards the posterior wall than the floor of cyst (dependent part in supine position).
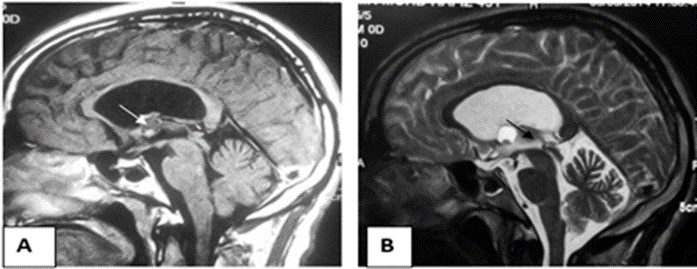
Intramural nodule was found in a single patient I, 45 yr. male who presented with headache, nausea and vomiting. Papilledema was absent on fundus examination. On imaging cyst was hyperdense on CT, hypointense on T1 and hyperintense on T2 weighted MRI (Figure no. 8). Cyst size was 20mm. and ventriculomegaly was present. Besides this, an intramural nodule was seen within the cyst. The nodule appeared as a well-defined round lesion at the floor of cyst which was fixed in its position in all the sections of imaging unlike hemorrhage which aligns itself on the dependent part of cyst. Nodule was hyperintense on T1 and hypointense on T2. Gross Total Endoscopic resection of the cyst was done. Follow up at 44 months showed complete resolution of all symptoms without any ventriculomegaly and residual lesion in imaging. However, the patient developed minimal subjective visual disturbances after surgery. Follow up examination however showed no gross deterioration in visual acuity and no papilledema.
Figure 8: T1 (A) & T2 (B) weighted sagittal MR images showing intramural within the colloid cyst of third ventricle in patient I. It appears as well defined, round mass stuck to the floor of cyst. Nodule is hyperintense on T1 & hypointense on T2 weighted MRI suggesting much higher protein content and viscosity than the cyst.
Discussion
Contrast enhancement is predominantly associated with inflammatory and malignant lesions, making its occurrence in benign tumors like colloid cysts relatively rare. In our study, only 8.51% (4 cases) of the cysts exhibited peripheral contrast enhancement. Notably, all patients demonstrated a positive clinical outcome, marked by an improvement in symptomatology. Regarding radiological outcomes (in terms of presence of residual lesions), 75% of patients with contrast-enhancing cysts displayed a favorable outcome. In contrast, patients without contrast enhancement showed favorable outcomes in 76.74% (33 out of 43) of cases, and the difference was statistically insignificant (p value 0.93). A study conducted by Neva Coce et al [15]. in 2011 emphasized the rarity of cysts larger than 3 cm, and intracystic hemorrhage in giant colloid cysts had been reported in only three cases to date. Despite larger cyst sizes (greater than 30mm), a good radiological outcome was achieved in 66.67% (2 out of 3) of patients, compared to 77.27% (34 out of 44) with smaller cysts, and the difference was not statistically significant (p value- 0.56). Diyora et al [16]. in 2013 conducted a literature review and identified only six cases of hemorrhagic colloid cysts. One case involved a 35-year-old female with acute hemorrhage within the cyst, prompting emergency ventriculostomy and endoscopic subtotal resection. Another case involved a 9-year-old female with sudden neurological deterioration, leading to emergency ventriculostomy, craniotomy, and cyst resection. The remaining four cases were post-mortem proven. Subsequently, he also reported a case of a 20-year-old female with progressive symptoms, including headaches, nausea, memory disturbances, seizures, gait disturbances, bilateral papilledema, and a positive Babinski sign. On contrast CT, cyst was isodense, showed intracystic hemorrhage without any contrast enhancement (table no.3). On MR it was hyperintense on T1 and hypointense on T2. The patient underwent transcallosal resection, revealing intracystic hemorrhage intraoperatively. Follow-up revealed complete resolution of seizures and memory function. Tamura et al [17]. in 2013 reported a case of a 43-year-old male with a previously diagnosed small colloid cyst, presenting with sudden-onset headache and ventriculomegaly. The imaging showed a hyperdense mass in the third ventricle with bilateral intraventricular hemorrhage. The MRI demonstrated a hemorrhagic cystic lesion that was hyperintense on T1 and hypointense on T2 without contrast enhancement. Endoscopic subtotal resection was performed due to highly viscous cyst contents and a thick capsule, resulting in a successful clinical outcome (table no.3).
Table 3: showing comparison of relevent variables between 3 studies.
| Study | Diyora et al 2013 | Our study | Tamura et al 2013 | Our study |
| Age in years | 20 | 38 | 43 | 50 |
| Approach | Microsurgery | Microsurgery | Endoscopy | Endoscopy |
| NCCT head density | Isodense | Hyperdense | Hyperdense | Hyperdense |
| T1 MRI intensity | Hyperintense | Hyperintense | Hyperintense | Hypointense |
| T2 MRI intensity | Hypointense | Hypointense | Hypointense | Hyperintense |
| Contrast enhancement | Absent | Absent | Absent | Absent |
These studies collectively underscore the rare nature of certain radiological features in colloid cysts, emphasizing the need for a nuanced understanding for improved clinical and radiological management.
Conclusion
The colloid cyst is a rare intracranial tumor, with an incidence as low as 3 per million per year. Notably, existing studies in the literature predominantly focus on comparing surgical techniques or exploring clinical outcomes. However, scant attention has been given to the radiological outcome, particularly with regard to rare radiological findings. In our comprehensive study, we meticulously examined these atypical radiological features and have concluded that while these findings may not significantly alter the clinicoradiological outcome, they can pose a diagnostic challenge for neuroradiologists. We anticipate that our study will serve as a valuable resource, aiding neuroradiologists in navigating the diagnostic complexities associated with this infrequent tumor, characterized by a spectrum of uncommon radiological presentations.
Declarations
Conflict of interest statement
Conflict of Interest: None.
Disclosure of funding statement
Disclosure of Funding: None.
Availability of data and materials
Data can be accessed from record section of the institute.
Ethical Approval
The study was approved by ethics committee of institute. Data was gathered from the case sheets of patients containing preoperative clinical details, intraoperative surgical details and necessary postoperative details. Even after giving consent, subjects had the right to opt out from study at any point of time. Great care was taken about the patient privacy and information obtained in course of study, including personal identity was kept strictly confidential. Great caution was exercised to ensure that the subjects were not exposed to any added risk of suffering any harm, irreversible adverse effect while being part of the study.
Consent
A written informed consent was taken from each patient parents/legal guardian before including in study population. Those not giving consent were excluded.
References
- Hernesniemi J, Leivo S. (1996). Management outcome in third ventricular colloid cysts in a defined population: a series of 40 patients treated mainly by transcortical microsurgery. Surg Neurol, 45(1):2-14.
Publisher | Google Scholor - Lawrence JE, Nadarajah R, Treger TD, et al. (2015). Neuropsychiatric manifestations of colloid cysts: a review of literature. Psychiatry Danub, 27(1): S315-5320.
Publisher | Google Scholor - Osborn AG, Preece MT. (2006). Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology, 239(3):650-664.
Publisher | Google Scholor - Waggenspack GA, Guinto FC. (1989). MR and CT of masses of the anterosuperior third ventricle. AJR Am J Roentgenol, 152(3):609-614.
Publisher | Google Scholor - Kornienko VN, Pronin IN. (2008). Diagnostic Neuroradiology. Springer Verlag, 464-465.
Publisher | Google Scholor - Bigner DD, McLendon RE, Bruner JM. (1998). Russell and Rubinstein's Pathology of Tumors of the Nervous System. 6th ed. London: Hodder Headline Group, 338-342.
Publisher | Google Scholor - Zulch KJ. (1986). Brain Tumors, Their Biology and Pathology. 3rd ed. Berlin: Springer-Verlag, 519.
Publisher | Google Scholor - MacDonald RL, Humphreys RP, Rutka JT, Kestle JRW. (1994). Colloid cysts in children. Pediatr Neurosurg, 20(3):169-177.
Publisher | Google Scholor - Demirci S, Dogan KH, Erkol Z, et al. (2009). Sudden death due to a colloid cyst of the third ventricle: report of three cases with a special sign at autopsy. Forensic Sci Int, 189(1-3): E33-E36.
Publisher | Google Scholor - Symss NP, Ramamurti R. (2012). Colloid cyst of third ventricle. In: Textbook of Contemporary Neurosurgery by Vincent A Thamburaj, 80:1141-9.
Publisher | Google Scholor - Maeder PP, Holtas SL, Basibuyuk LN, et al. (1990). Colloid cysts of the third ventricle: correlation of MR and CT findings with histology and chemical analysis. AJNR Am J Neuroradiol, 11(3):575-581.
Publisher | Google Scholor - Bergsneider M. (2007). Complete microsurgical resection of colloid cysts with a dual port endoscopic technique. Neurosurgery, 60(4):613-618.
Publisher | Google Scholor - Armao D, Castillo M, Chen H, et al. (2000). Colloid cyst of the third ventricle: imaging-pathologic correlation. AJNR Am J Neuroradiol, 21(8):1470-1407.
Publisher | Google Scholor - El Khoury C, Brugières P, Decq P, et al. Colloid cysts of the third ventricle: Are MR imaging patterns predictive of difficulty with percutaneous treatment? AJNR Am J Neuroradiol, 21(3):489-492.
Publisher | Google Scholor - Coce N, et al. (2012). Large Hemorrhagic Colloid Cyst in a 35-Year-Old Male. Turkish Neurosurgery, 22(6):783-784.
Publisher | Google Scholor - Diyora B, Nayak N, Kukreja S, et al. (2013). Hemorrhagic colloid cyst: Case report and review of the literature. Asian J Neurosurg, 8(3):162.
Publisher | Google Scholor - Tamura Y, Uesugi T, Tucker A, et al. (2013). Hemorrhagic colloid cyst with intraventricular extension. J Neurosurg. 2013;118(3):498-501.
Publisher | Google Scholor