Research Article
Analgesia and Anesthesia
1Riggs pharmaceutical, Department of Pharmacy University of Karachi Pakistan.
2Assistant Professor, Department of Microbiology, University of Karachi, Pakistan.
3Head Department of Pharmacology, Fazaia Ruth Pfau Medical College, Shahrahe Faisal Karachi, Pakistan.
*Corresponding Author: Rehan Haider, Riggs pharmaceutical, Department of Pharmacy University of Karachi Pakistan.
Citation: Haider R, Zehra A, Mehdi A. (2024). Analgesia and Anesthesia. Addiction Research and Behavioural Therapies, BioRes Scientia Publishers. 3(1):1-8. DOI: 10.59657/2837-8032.brs.24.012
Copyright: © 2024 Rehan Haider, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 01, 2023 | Accepted: February 20, 2024 | Published: February 26, 2024
Abstract
Analgesia and anesthesia are two critical components of modern medical practice, each serving distinct but interrelated purposes in the management of pain and facilitation of medical procedures. This abstract provides a concise overview of these concepts, their applications, and their significance in health care. Analgesia, the relief of pain without loss of consciousness, plays a pivotal role in improving the quality of life of patients with acute or chronic pain. It encompasses a spectrum of interventions, ranging from over-the-counter pain relievers to powerful prescription medications and Nonpharmacological approaches. Effective analgesia not only alleviates suffering but also enhances patient comfort, promotes faster recovery, and can reduce the risk of chronic pain development. In contrast, anesthesia induces a reversible state of unconsciousness and loss of sensation, which is often necessary for pain-free surgical and medical procedures. Anesthesia can be further categorized into general anesthesia, which affects the entire body, and regional anesthesia, which blocks pain in specific areas of the body. Skillfully administered anesthesia ensures patient safety, comfort, and cooperation during surgical interventions while mitigating physiological responses to stress. Both analgesia and anesthesia have evolved significantly over the years with advances in pharmacology, technology, and medical knowledge. They are integral to various medical disciplines, including surgery, obstetrics, dentistry, and critical care, enabling healthcare professionals to perform procedures that would otherwise be extremely painful or impossible.
Keywords: analgesia; anesthesia; pain relief; consciousness; medical procedures; pharmacology; surgical interventions; patient comfort; regional anesthesia; general anesthesia
Introduction
Pain
The distress and pain girls frequently sustain while they are wrestling through troublesome labor are further described and appear expected in addition to the psychology of humankind's hopeful intelligence to endure some different degrees. Medical men concede the possibility of fighting the super induction of the induced absence of feeling in childbirth for a short time, but our cases will force the use of it upon the declaration. The entire question is whether an individual is momentary. These statements by James Young Simpson in 1847 [1] are still the most suitable, as they encapsulate today's widely grasped view of parturients and most perinatal care providers. First, most of today's laboring mothers are not going to endure harsh pain, and more importantly, they know that it is no longer inevitable.
pain is delimited by an international association for the study of pain as a bad, emotional, auditory and exciting occurrence that guides real or potential fabric damage or expressed in agreements of specific damage.' In informal agreements, pain is what hurts and is an irrelevant attribute for most laborers. Severe pain is average, affecting 60–70% of nulliparous and 35–40% of multi parous laborers. Therefore, many determinants can contribute to pain in labor; a particular etiological disease of the causes of the aforementioned pain is troublesome, but ALL causes of pain must be considered and examined before dullness is administered. While shortening pain, cervical extension, and second-stage labor pain have obvious physiological causes, the footing of harsh pain in some individuals concedes the possibility of restricted labor, before birth position, extreme worry, uterine hyper stimulation, uterine rupture, or extant study of plants; to a degree, fibromyalgia or different tumors, hemorrhoids, adhesions, markings from former abscission, and so on. Harsh pain is mainly a friendly autonomic response and involves tiredness, aridity, squalor, bred essence rate, ancestral pressure, oxygen and hydrogen devouring, diminished blood flow, and oxygen to the covering layer and blastosphere, gasping, and cramps.
Obviously, for many individuals, the aforementioned belongings are unacceptable, and for a few, the possibility may be severe. While many authors distinguish between physiologic and healing pain of some kind in the individual, if harsh enough to surpass the person’s beginning of tolerance, it results in the sensitively intervened answers filed above. Pain relief is quickly possible in terms of income. Most mothers desire control when they are in labor, but many cannot realize this if or when they cannot deal with harsh pain. For most wives, the event, type, and severity of pain in labor are variable. Thus, it is wise to warn all anticipating founders to maintain an open mind about pain and its relaxation and to accept the benefits, difficulties, benefits, and risks of all methods of induced sleep available. In at-risk pregnancies, be they on account of before birth, obstetric or motherly determinants, dullness, or anesthesia is, in most cases, necessary and repeatedly urged. If specific risk determinants increase the hazards of any sleep-inducing or numbing drug process, Conferences accompanying anesthetists throughout gestation are prudent.
Obstetric analgesia and anesthesia
The ideal painkiller method in labor
1: Provide swift, effective, and reliable pain aids for all stages.
2: Not compromising maternal plant structure or usual activity.
3not compromise before birth, the essential study of animals or happiness.
4not hamper the rational processes of labor.
5: Be responsive enough to convert to anesthesia for critical active transmittal or added invasion, for instance, manual removal of the covering layer.
Meeting the aforementioned ideal would leave the mom awake, alert, comfortable, and able to void, close in on, and, if wanted, even ambling throughout labor. Unfortunately, the aforementioned ethics are exceptionally common in cure; except for the past twenty or so years of age, the incidence of depressed-dose neuraxial induced sleep and analgesia (epidural and linked) sleep-inducing or numbing drug-epidural (CSE) has almost been realized.
There were two plans for obstetric dullness.
1: Reduction of the understanding of pain, that is, decline of the brain’s idea of, and the body and mind’s answer to reduce pain—that is, reduce the belongings of pain.
2. Reduction of the broadcast of pain, that is, a decline in the ability of the nerves to conduct pain. Three ways of implementing these game plans are attainable: psychological methods, to a degree, a positive stance, fetal instruction, preparation (material and mental entertainment), and daze, which are beneficial to many mothers for temperate and moderately harsh pain.
Physical systems involve massage and entertainment techniques and transcutaneous energetic nerve provocation (TENS), but like the subjective methods filed above, they often forsake when pain surpasses one’s beginning of fortitude. Pharmacological techniques concede to the possibility of being fundamental or territorial local Systemic drugs are persuasive as they are for shock. post-operative or different harsh pain positions, but in pregnant, they may have the disadvantage of moving utero placental ancestry flow and the blastosphere, either straightforwardly or obliquely.
Nevertheless, some vaporous drugs have specific as inhaled anesthetics, and sevoflurane has intensely rapid operation, removal, and slightest absorption and aggregation, which creates a bureaucracy ideal for sporadic use ‘accompanying contractions.’ As accompanying all fundamental, centrally acting drugs, nevertheless, reactions such as dizziness, sickness in the stomach, and lethargy limit their efficiency. Parenterally executed analgesics have been a favorite in obstetrics for many decades, but the same warnings have been administered. Older opiates such as anesthetics and pethidine (meperidine) are troublesome to titrate to effect; are mostly likely intramuscularly, developing in variable incorporation and productiveness, accompanied by extended or poorly timed use, expand in the unborn young and influence before birth happiness and neonatal cardiorespiratory physiology. This is specifically valid for pethidine and its allure basic metabolite, not pethidine when used during the entire labor period. However, two opioids, fentanyl, and remifentanil, which are forceful, short-acting, and swiftly redistributed and metabolized, are the most productive and safe, if likely similarly certified directions and monitoring.
Small venous boluses of fentanyl (20–25 µg) grant permission to likely in the second stage of labor to lessen pain and assist the parent to cooperate. This is particularly beneficial when impulsive childbirth is possible, and there is no evidence of epidural or additional induced sleep. Neonatal despair is uncommon, but if it does happen, it is quickly turned into a single dose of naloxone into the umbilical rope vein. Ketamine is a forceful non-opioid pain reliever that, in limited intermittent endovenous doses (3–5 mg), is excessively useful for temporary, late-second-stage analgesia in selected victims. Both fentanyl and remifentanil may be self-executed by patient-controlled induced sleep (PCA) designs. Remifentanil is exceptionally promising in these circumstances, but there have been few reserved tests to date. Most anesthetists would recommend a PCA rule accompanying either of these powers when neuraxial-induced sleep is contraindicated, provided that accompanying midwives are prepared to project this type of analgesia.
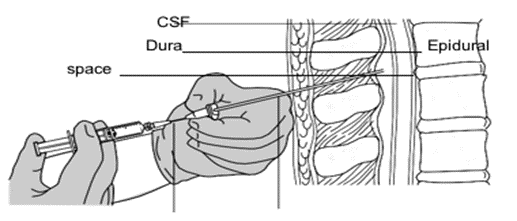
Regional, most usually neuraxial, induced absence of feeling has severely changed healing and public stances toward obstetric-induced absence of feeling and pain remedies since the 1980s. Although lumbar epidurals have exited the criteria of neuraxial technique since the late 1960s, the classic notes of Wang [2] and Behar [3], which demonstrated the sleep-inducer conduct of neuraxial opioids, unlocked an extraordinary study of epidural and sleep-inducer barrier When Intraspinal opioids are linked to local sleep-inducing or numbing drugs. (LAs), Their operation is cooperative, enabling lower measurement of the two drugs together provide neural blockade of variable force [4]. These techniques, still widely referred to as ‘epidurals,’ involve constant subarachnoid (sleep-inducing or numbing drug) stimulation. anesthesia (CSA), epidurals, and specifically depressed-measure CSE is most suitable for labor analgesia in the vast adulthood of parturients and is fast and dependably changeable to anesthesia for influential transmittal or additional obstetric or surgical intervention [4]. CSE, and less often CSA, principally has another in one's place, the use of a sole-shot. sleep-induced sleep for influential transmittance in most obstetric areas of the UK [5, 6]. Similarly, depressed-dose CSE is fast becoming the chosen choice of neuraxial dullness for labor [7]. Caudal epidural block, which is valuable for a few gynecological procedures, is exceptionally secondhand in obstetrics and is not urged. A transvaginal pudendal block is occasionally used for a ‘lift-out’ gripper or ventouse transfer. However, the failure rate is high (30%), LA doses are extreme, which may cause acute toxicity, and there is a risk of needles entering the before-birth head. In rare situations in which the obstetrician is the sole controller or does not have expert anesthesia duties feasible, a depressed-prescription single ammunition sleep-inducing or numbing drug sleep-inducing or numbing drug at L3-4 or L4-5 is arguably the best-induced sleep for influential vaginal transfer or repair of vaginal or perineal trauma. The lowest type of CSE secondhand for induced sleep is the tease-through-needle method is illustrated in Figure 1.
Figure 1: Needle-through-needle CSE technique.
Table 1: Low-dose CSE compared with epidural and S-S spinal.
| S-S spinal∗ | Epidural | CSE | |
| Onset of action(min) | Fast (1–5) | Slow (10–20) | Fast (1–5) |
| Median pain | 0 | 0–3 | 0 |
| score 60–90 min | |||
| Total drugs dose | Low | High | Low |
| Observable leg | 100 | 5–50 | 0–40 |
Table 2: Requirements for safe ‘walking epidurals’ in labour Cooperative, understanding parturient.
| weakness (%)† | |||
| Post-dural puncture | 1–2 | 0.3–1.0 | 0.2–0.7 headache (%) |
| Hypotension (%)† | 20–80 | 5–10 | 5–10 |
| Failure (i.e., GA is | 1.7–6.0 | 2–6 | 0.3–0.7 required) (%) † |
| Pruritus (%) † | 50–80 | 20–80 | 20–80 |
| Duration (min) | 60–240 | ∞ | ∞ |
Presenting part of fetus engaged and well applied to cervix Minimal or no motor and pronociceptive block No postural hypotension Continuous fetal monitoring (CTG), when indicated Suitable conditions: good epidural catheter fixation; attending midwife; disconnect (bung) IV line; no shoes; safe, even floor without cables, steps, mats, etc. The process comprises a depressed-lot intrathecal needle of LA, usually bupivacaine (2–2.5 mg) plus fentanyl (15–25 mcg), followed by the insertion of an epidural catheter was used for continuous induced sleep or induced absence of feeling, if necessary. For anesthesia, the subarachnoid application is suitably raised. Compared with distinct-discharge inventors must have a neuraxial block administered all the while laboring because if the need for interference arises, the epidural catheter may be fast ‘surpassed-up’ to support appropriate anesthesia.
For assisting childbirth, maternal ‘capacities’ are If necessary, the top-up block may be tailored to determine the visual barrier of sacral dermatomes and up to the T10 level while maintaining engine capacity in the abdominal muscles. Bearing down can begin before, occurring after with shortenings. For surgical fetus delivery, the epidural is surpassed. with dosage sufficient to provide relaxation of intestinal powers, and a visual block of the dermatomes to T4. One disadvantage of neuraxial-induced sleep for influential transmittal is that the anesthesia does not supply tocolysis, even though this may have achieved accompanying drip glyceryl trinitrate or added drugs Because harsh pain increases the sympathetic pitch, accompanying an effect on a rise in blood pressure, oxygen use, and redistribution of cardiac production developing in reduced utero placental perfusion, many at-risk pregnant women can benefit from the optimum dullness for all of the labor. Pre-eclampsia, other hypertensive states, and additional cardio-respiring disorders are good indications for neuraxial analgesia in labor, even though severe pain is missing. In extreme-risk patients, neuraxial-induced sleep for medical procedures, or active Delivery is frequently used as the method of choice. Low-shot CSE can provide obvious Hemodynamics balance in parturients, accompanying severe aortic or mitral blockage, opposing cardiomyopathy, and pulmonary hypertension caused by elective Caesarean section [16]. Such subjects require expert crew administration beginning early in gestation. Because motherly and before-birth morbidity and death.
Table 3: Contraindications to neuraxial blockade Absolute.
| Patient refusal | Raised intracranial pressure Infection: systemic and localized Uncorrected hypovolemia |
| Relative | Coagulopathy, anticoagulant therapy Spinal/neurological pathology, abnormality Some complex cardiovascular and other conditions Inadequately skilled management team Urgency (Degree of urgency) |
In the aforementioned cases, early consultation with a cardiologist and an anesthetist is authoritative for fear that management plans may be consented to, for ongoing listening and care, and electoral or dangerous transfer. Any Anesthesia in the aforementioned subjects is conceivably hazardous and causes neuraxial methods to concede the possibility of failure, another plan must be planned for, with all appropriate facilities and careers.
Informed consent for anesthetic procedure
Through the 1990s, in developed countries, the number of girls taking a sleep-inducing or numbing drug process in union with a gestational age increased to 60% [17] following the increasing recognition of, and demand for, neuraxially induced sleep—earlier founders, corpulence, increased Caesarean childbirth rates, artificial pollination processes, and so forth. Because ALL expectant founders concede the possibility that they demand an induced absence of feeling or induced sleep, appropriate news on all facets of pain, induced absence of feeling, and induced sleep must be likely to affect all daughters in the antenatal period. When tension, fear, or unwillingness is signified, a conference accompanying the obstetric anesthetist should be organized throughout gestation. Such pre-instruction is required to prevent troubles in obtaining cognizant consent when induced sleep is required or desired, particularly in demanding or dangerous positions and when the mother is experiencing harsh pain [18].
General Anesthesia
‘If we manage to encourage anesthesia outside misfortune of knowledge, most would regard it as an even better advance’, mentioned James Young Simpson soon after a motherly sleep-inducing or numbing drug demise in the early days of toxin-induced absence of feeling in 1847 [1]. In 2000, the National Sentinel Caesarean section audit reported that common induced sleep (GA) was secondhand in less than 30% of Caesarean deliveries, and most of these were dangerous [19]. GA is used for only 5% of all Caesarean deliveries at Queen Charlotte’s Hospital, London. Moreover, GA remnants the induced absence of a feeling of choice for abandoned neuraxial blocks, positions when territorial anesthesia is contraindicated, and additional abscission in gestation and puerperium, as shown below. Indeed, the ‘better advance’ predicted by Simpson, may be visualized in the obvious reduction in motherly humanness, as neuraxial-induced sleep has superseded GA all the while in ancient times (50 years ago). GA in pregnancy is deliberate and far more dangerous than for a sane society, accompanied by airway troubles, abandoned intubation, pulmonary goals about the stomach cargos, and their sequelae accounting for the plurality of oblivion. However, the second Confidential Maternal Mortality Reports 1952 regularly suggested that most of the direct sleep-inducing or numbing drug extinction from GA, whatever the cause, manage have been obviated, accompanying better ideas middle from two points: obstetricians and anesthetists. As stated above, ALL gravidae are potential candidates for anesthesia.
This is frequently necessary during crises. As anticipating founders are a ‘captive’ population accompanying balanced antenatal care and review, it is authoritative that sleep-inducing or numbing drug risk determinants be identified, and an appropriate sleep-inducing or numbing drug conference organized early in pregnancy. ‘At-risk’ Gravidae should include all those with specific risk determinants. Despite skilled care, there may be no obstetric problems before birth or healing obstacles. The major anesthetic risk determinants are listed in Table 3 however, this list is not inclusive. In many cases, clinical judgment rules out the need for antenatal-induced sleep conferences. Because ALL parturient are in danger of pulmonary aspiration about the stomach details, the protective opposite of an acid and/or H-2 Blocking premedication is a standard practice before two territories and GA. General-induced sleep is regularly used for crises and medical procedures when the neuraxial block is contraindicated. However, in many laboratories, the prospect of active or assisted transfer may be expected, and an important GA is avoided by bearing neuraxial dullness previously in a seated position, which may be used to encourage the induced absence of feeling fast when required. Many anesthetists will approve a blend of common and neuraxially induced sleep for Caesarean hysterectomy and other difficult incisions, permissive the parent to be awake for transmission and before enduring the GA to balance the operation. An epidural catheter was placed before the second hand for post-influentially induced sleep. Similarly, for fetal abscission or additional medical procedures before birth, combined GA and block are repeated secondhand. Such blend supplies optimal tocolysis accompanying explosive sleep-inducing or numbing drug powers, such as isoflurane.
Modern GA drugs do not increase the risk of uterine atony post-childbirth, but uterine color should be closely monitored and appropriate oxytocin administered as needed. Acute Tocolytic drugs are examined outside, but during active transfusion and fetal medical procedures, the anesthetist concedes that severe tocolysis may be required. Arguably, changeable anesthetic drugs are ultimately productive acute Tocolytic drugs reviewed abroad, but throughout the operative transfer and before birth surgery, the anesthetist grants proper permission to provide severe tocolysis. Arguably, changeable sleep-inducing or numbing drugs are the most persuasive severe tocolytics; however, by definition, they encourage ignorance and, accordingly, a generally induced absence of feeling. Endogenous alternatives are accessible and may be used for locally induced sleep; however, they must be used with caution and appropriate monitoring. A cardiovascular collapse occurred. As defined above, GA and Optimized tocolysis are frequently a favorite for complex medical procedures. involving uterine manipulations and some multiple pregnancy deliveries, for instance, combined or mono-amniotic twins, In New, obstetric procedures involve anesthesia. processes in most of the patients. Close participation, conference and planning, and the slightest use of the accepted induced absence of feeling, particularly in emergency positions, have remarkably shortened maternal and perinatal humanness and depression and will stretch to do so. All expectant inventors. grant permission, demand analgesia, or induced absence of feeling, so risk determinants must beg and acted upon antenatally to uphold the influential record of security of induced absence of feeling in obstetrics.
Research Method
Study Design
This multi-uniform dispassionate trial was conducted in the U.S. Department of Veterans Affairs (VA) Cooperative Studies Program to evaluate the impact of intraoperative epidural sleep and medical checkup epidural-induced sleep distinguished from general sleep uniqueness and medical checkup intrinsic opioid dullness. This study aimed to investigate the effects of medications on perioperative effects and medical check-up pain administration.
Patient Population
A total of 1,021 patients with four larger intra-abdominal movements (intra-abdominal aortic, stomach, biliary, or colon) were included in the study. The election was randomized with inmates filling a place in either group.
Interventions
Group 1: Comprehensive anesthesia and examination of dullness accompanying parenteral opioids.
Group 2: Received epidural plus light comprehensive sleep and postoperative epidural opiate.
Data Collection
Patients were listened to for miscellaneous limits, including death and main obstacles, all the while and until 30 days after the medical procedure. Additionally, postoperative pain levels, time to walk, and time of nursing home stay were recorded.
Results
Overall, there was no meaningful distinction in the occurrence of extinction and important complications between the two groups. However, for cases meeting with intestinal aortic surgery, the skill was a notable distinctness. In group 2 (epidural plus light inexact sleep and epidural narcotic), the incidence of oblivion and main difficulties was considerably lower (22%), compared to group 1 (general sleep and parenteral opioids, 37%). This dissimilarity generally stopped alternatives in the incidence of new heart attacks, strokes, and respiratory deficiency. Group 2 sufferers took significantly less pain reliever but stated better pain relaxation compared to group 1 patients. Among aortic resection victims in Camp 2, endotracheal intubation was 13 hours shorter, and the surgical intensive care stay was 3.5 hours shorter.
Conclusions
Implications of the Study
The study's results highlight that the impact of sleep-inducer and examination painkiller methods on perioperative effects varies contingent upon the type of movement acted upon. Overall, epidural-induced sleep supports superior postoperative pain relief. For sufferers withstanding intestinal aortic movements, the use of epidural anesthesia and epidural-induced absence of feeling considerably upgraded the overall consequences, including reduced intubation opportunities and a surgically exhaustive care stay. These judgments join the accompanying previously stated benefits of epidural sleep in the way that better abolition of surgical stress, beneficial effects on medical checkup nitrogen balance, more fixed cardiovascular Hemodynamics, lowered ancestry deficit, upgraded peripheral vascular distribution, and improved examination pain control.
Discussion
In the "Discussion" division, you would define and discuss the associations of your judgments in more detail. You can again equate your results to existing drama and address potential restraints of the study.
Please note that the real content and analyses inside each section rest on your distinguishing research verdicts and methods. This outline provides a foundation for your long student essay by establishing the facts provided in your research summary.
Interpretation of Findings
The study's judgments are of meaningful dispassionate significance as they clear up the impact of different sleep and induced sleep methods on perioperative consequences and medical checkup pain management in victims withstanding main intraabdominal movements. The debate over these findings revolves around various indispensable contents:
Variability in Perioperative Outcomes
The results stress the instability in perioperative outcomes contingent upon the type of surgical process. While there was no important distinctness in the incidence of end-of-life and bigger obstacles in the middle of two study groups across all types of operations, a notable irregularity was noticed in subjects going through intestinal aortic surgery. This subgroup, enhanced considerably by the linked use of epidural sleep and examination epidural analgesia, experiences a lower occurrence of antagonistic occurrences. This verdict underscores the significance of adjusting sleep-inducing and painkiller blueprints to specific surgical frameworks. Benefits of Epidural Analgesia: One of the key takeaways from this study is the logical predominance of epidural-induced absence of feeling in providing persuasive medical checkup pain relief. Patients in the group taking epidural sleep and medical checkup epidural drugs stated better pain control despite taking less pain reliever. This desire for the mean delivery of pain aid through epidural administration concedes the possibility of offering benefits over fundamental opioid-based approaches while accompanying premature research emphasizes the benefits of epidural-induced sleep in various surgical backgrounds.
Enhanced Recovery: In addition to revised pain administration, victims in the group experiencing abdominal aortic abscission, epidural sleep, and dullness experienced considerably smaller endotracheal intubation opportunities and decreased stays in surgical exhaustive care. These outcomes are indicative of reinforced medical checkup improvement, weakened complications, and more effective means of exercise. The benefits noticed concerning this approach in distinguishing patient culture underline the potential for fuller application in optimizing surgical care.
Existing Literature and Clinical Relevance: The verdicts bestowed present agree with prior studies reporting the benefits of epidural sleep and induced absence of feeling in the way that better stress abolition, improved examination nitrogen balance, fixed cardiovascular Hemodynamics, lowered ancestry misfortune, and enhanced minor vascular distribution However, it is important to note that the associations between these benefits and the overall consequences for surgical patients have been a subject of debate in the article. Our study, with its allure of the best sample size and reserved variables, contributes valuable evidence to this continuous consideration. Limitations and Future Research: While this study determines valuable observations, it is essential to accept allure restraints, containing the devoted effort to something specific types of intraabdominal movements and the forbiddance of certain patient populations. Future research will aim to explore the relevance of these verdicts to a fuller range of surgical processes and patient counts. Additionally, factors such as the American Society of Anesthesiologists (ASA) tangible rank categorization, age, neuter, and Goldman Risk Index should be thought out in further surveys to better control for potentially confusing variables.
Conclusion
This study shows that the choice of sleep-inducer and painkiller techniques can have an important effect on perioperative effects and examination pain administration. Epidural sleep and analgesia, when used sensibly, offer benefits in certain surgical circumstances, specifically in abdominal aortic sections. These judgments influence our understanding of optimizing surgical care and emphasize the significance of adjusting anesthesia and induced sleep policies to individual patient needs and surgical processes. Future research endeavors concede the possibility of counting on these results to further purify and expand our information in this detracting region of perioperative care.
Declarations
Acknowledgment
The completion of this research project would not have been possible without the contributions and support of many individuals and organizations. We are deeply grateful to all those who played a role in the success of this project I would also like to thank My Mentor [Dr. Naweed Imam Syed Prof. Department of Cell Biology at the University of Calgary and Dr. Sadaf Ahmed Head of the Psychophysiology Research Lab University of Karachi, their invaluable input and support throughout the research process. Their insights and expertise were instrumental in shaping the direction of this project.
Declaration of Interest
I at this moment declare that I have no pecuniary or other personal interest, direct or indirect, in any matter that raises or may raise a conflict with my duties as a manager of my office Management.
Conflicts of Interest
The author declare that they have no conflict of interest.
Financial support and sponsorship.
No Funding was received to assist with the preparation of this manuscript.
References
- Simpson JY. (1847). Notes on Chloroform.
Publisher | Google Scholor - Wang JK, Nauss LA and Thomas JE. (1979). Pain remedy by intrathecally used narcotic in a guy. Anesthesiology, 50:149-151.
Publisher | Google Scholor - Behar M, Magora F, Olshwang D., & Davidson JT. (1979). Epidural opiate in situations of pain. Lancet, 1:527-529.
Publisher | Google Scholor - Campbell DC, Camann WC, & Datta S. (1995). The addition of bupivacaine to sufentanil for labor analgesia. Anesth Analg, 81:305-309.
Publisher | Google Scholor - Crowhurst JA & Birnbach D (2000) Low-dose neuraxial block: course towards the new serenity. (Editorial). Anesth Analg, 90:24.
Publisher | Google Scholor - Rawal N, Van Zundert A, Holmström B, & Crowhurst J. (1997). Combined sleep-inducing or numbing drug-epidural method. Reg Anesth, 22:406-423.
Publisher | Google Scholor - Ranasinghe JS, Steadman J, Toyama T, and Lai M. (2003). Combined sleep-inducer Epidural-induced absence of feeling is better than sleep-inducer or epidural unique for Caesarean transfer. Br J Anaesth, 91:299-300.
Publisher | Google Scholor - Plaat F, Alsaud S, Crowhurst JA., and others (1996) Selective tactile barrier accompanying depressed-dose-linked sleep-inducing or numbing drug or epidural (CSE) admits safe ambulation in labor. A ship study Int J Obstet Anaesth, 5(3):220.
Publisher | Google Scholor - Collis RE, Baxandall ML, Srikantha rajah ID, and others (1993) Combined sleep-inducing or numbing drug epidural dullness accompanying capability to walk during the whole of labor. Lancet, 341:767-768.
Publisher | Google Scholor - Rawal N. (1995). European styles in the use of linked sleep-inducing or numbing drug epidural method: a 17-nation survey. Reg Anesth, 20(2S):162.
Publisher | Google Scholor - ‘COMET’ students that study together in the UK (2001) Effect of reduced-application movable against usual epidural methods in the fashion of transfer: a randomized, reserved trial. Lancet, 358:19-23.
Publisher | Google Scholor - Vercauteren MP, Coppejans HC, Hoffman VH, and others (2000) Prevention of hypotension by a distinct 5-mg prescription of ephedrine during narrow-measurement sleep-inducer sleep in prehydrated surgical fetus delivery and childbirth. cases Anesth Analg, 90:324-327.
Publisher | Google Scholor - Ong BY, Cohen MM, Esmail A, and others. (1987). Paresthesias and engine dysfunction, subsequently labor, and transfer. Anesth Analg, 66:18-22.
Publisher | Google Scholor - Holdcroft A, Gibberd FB., Hargrove RL., and others. (1995). Neurological problems guide pregnancy. Br J Anaesth, 75:522-526.
Publisher | Google Scholor - Wong CA, Scavone BM, Dugan S and others. (2003). Incidence of postpartum lumbosacral backbone and lower limit nerve harm. Obstet Gynecol, 101:279-298.
Publisher | Google Scholor - Hamlyn L, Plaat F, Stocks G, & Crowhurst JA. (2005). Low-lot linked sleep-inducing or numbing drug-epidural-induced sleep for surgical fetus delivery and transmission of extreme-risk cardiac affliction parturients. Int J Obstet Anesth, 14:355-361.
Publisher | Google Scholor - Crowhurst JA. (1992). Epidurals in obstetrics: by what reliability? (Editorial). Med J Aust, 157(4):220-22.
Publisher | Google Scholor - Crowhurst JA & Plaat F. (2001). Pain relief in labor and the anesthetist. In: MacLean AB, Stones RW, & Thornton S (eds.) Pain in Obstetrics and Gynecology London. RCOG Press, 356-357.
Publisher | Google Scholor - Thomas J and Paranjothy S. (2001). The National Sentinel Caesarean Section Audit Report. London: RCOG Press.
Publisher | Google Scholor