Research Article
An Assessment of Atherosclerotic Cardiovascular Disease in Non-alcoholic Fatty Liver Disease Patients with Type 2 Diabetes Mellitus
- Aadil Mahmood Khan, MD 1*
- Hassan Chaudhry, MD 2
- Abimbola Ajibowo, MD 3
- Ogbonnaya Akuma, MD 4
- Chinaza Mercy Akuma, MD 5
- Chengala Ananyaa Gowthavaram, MBBS 6
- Ashwini Mahadevaiah, MBBS 7
- Nafisa Mustafa, MBBS 8
- Oluwabukola Oyeleye Adegbite MD, MPH 9
- Olasunkanmi Kolawole, MD, MPH 10
- Toluwalope Ejiyooye MD, MPH 11
- Bukola Olagbende, MD 12
- Duaa Nasereldin, MBBS 13
1Ganesh Shankar Vidyarthi Memorial (G.S.V.M.) Medical College, Kanpur, Uttar Pradesh, India.
2Medical University of Lublin, Lublin, Poland, European Union.
3Lugansk State Medical University, Ukraine.
4Ebonyi State University, Department of Medicine, Abakaliki, Ebonyi State, Nigeria.
5Nnamdi Azikiwe University, Nigeria.
6Malla Reddy Institute of Medical Sciences, Hyderabad, India.
7JSS University, Mysore.
8National Ribat University, Khartoum, Sudan.
9Texas A&M University, College Station, TX, USA.
10UT Health School of Public Health, Texas, USA.
11Walden University, Minnesota, USA.
12Meharry Medical College, Tennessee, USA.
13Ahfad University for Women, Khartoum, Sudan.
*Corresponding Author: Aadil Mahmood Khan, Ganesh Shankar Vidyarthi Memorial (G.S.V.M.) Medical College, Kanpur, Uttar Pradesh, India.
Citation: Aadil M. Khan, Chaudhry H., Ajibowo A., Akuma O., Chinaza M. Akuma. et al. (2023). An Assessment of Atherosclerotic Cardiovascular Disease in Non-alcoholic Fatty Liver Disease Patients with Type 2 Diabetes Mellitus. Clinical Case Reports and Studies, BRS Publishers. 3(1):1-7. DOI: 10.59657/2837-2565.brs.23.054
Copyright: © 2023 Aadil Mahmood Khan, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 08, 2023 | Accepted: August 03, 2023 | Published: August 10, 2023
Abstract
Background: Non-alcoholic fatty liver disease (NAFLD) is most frequently related to type 2 diabetes (T2DM), which can advance to fibrosis and cirrhosis. Prior research has shown that patients with T2DM with NAFLD have a synergistic increase in the atherosclerosis of the cardiac vasculature. Our study aimed to assess and correlate atherosclerotic heart disease in patients with NAFLD and T2DM.
Materials and methods: An observational cross-sectional study to know cardiovascular atherosclerotic disease in NAFLD patients with T2DM was conducted between December 2019 and October 2021. Subjects included fifty-five T2DM patients screened as prospects for the study, including patients receiving treatment inside the outpatient department (OPD), an affiliated diabetes clinic, and affected individuals admitted to a hospital.
Results: Results showed a moderately positive correlation between an ASCVD risk score and Fibro Scan E results, with the findings being statistically significant. However, there was no significant difference in A.S.C.V.D. Risk score in both fatty and non-fatty liver groups as well as steatosis and non-steatosis groups.
Conclusion: Identifying NAFLD in type II DM patients may facilitate better cardiovascular disease risk estimation with practical management implications. Moreover, identifying people with NAFLD would highlight a subgroup of diabetic patients who may benefit from more intensive preventative treatment and cardio-protective measures to decrease their risk of future CVD.
Keywords: non-alcohol fatty liver disease; ASCVD risk score; fibro scan; type II DM; NAFLD fibrosis score
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a general term used to cover a spectrum of conditions characterized by the evidence of hepatic steatosis on imaging or histology (macro vesicular steatosis). The absence of secondary causes of hepatic steatoses, such as significant alcohol consumption and chronic medication usage, can cause hepatic steatosis or exacerbate a hereditary disorder [1]7/27/2023 10:53:00 AM. The pathology strongly resembles alcohol-induced injury but without substantial alcohol intake. NAFLD can be split between simple steatosis termed non-alcoholic fatty liver (NAFL) to non-alcoholic steatohepatitis (NASH) and can progress to cirrhosis or even hepatocellular carcinoma (HCC) [2-6].
NAFLD, obesity, T2DM, dyslipidemia, and insulin resistance, all of which are components of metabolic syndrome, are frequently linked together, strongly supporting the notion that NAFLD is the hepatic manifestation of the syndrome [7]. NAFLD has been reported to range from 15-30% in the general population of different countries and is almost certainly increasing globally [8,9]. Compared with non-diabetic subjects, people with T2DM appear to have an increased risk of developing NAFLD and clearly show a higher risk of developing fibrosis and cirrhosis. T2DM is a long-recognized independent cardiovascular risk factor (CVRF) and a frequent finding in NAFLD [10].
Approximately 60% of T2DM patients have NAFLD [11,12]. Furthermore, patients with T2DM and NAFLD have a higher risk of cardiovascular disease than patients with T2DM alone, suggesting a potential synergistic increase of cardiovascular disease risk in patients affected by both conditions [13,14]. Recent data indicate that the presence of NAFLD in T2DM is strongly linked to increased CVD risk independently of the metabolic syndrome. However, this hypothesis needs verification through more extensive studies. When assessing disease severity and risk of progression to cirrhosis, it is helpful to divide NAFLD into NAFL and NASH via their histologic differences. In NASH, hepatic inflammation is present in contrast to NAFL, which involves only steatosis [15].
A NAFLD Activity Score (NAS) assigns numerical values to different histologic measures of steatosis, inflammation, cell injury, and fibrosis in one approach used to define the extent of the disease's severity. The cumulative score classifies patients as having NAFL, borderline NASH, or fully developed NASH. Commonalities in the pathophysiologic changes between patients with NAFLD and T2DM cause an increase in cardiovascular risk. These changes can include proatherogenic lipid alteration, elevated thrombotic factors, insulin resistance, low-grade inflammation, and changes to the microbiome. With the framework above, this study has examined the CVD risk in NAFLD patients with T2DM.
Materials & Methods
The Department of Medicine at G.S.V.M Medical College tested cardiovascular atherosclerotic disease in NAFLD patients with T2DM from December 2019 to October 2021 using an observational cross-sectional study. Subjects included fifty-five T2DM patients screened as prospects for the study, including patients receiving treatment inside the outpatient department (OPD), an affiliated diabetes clinic, and affected individuals admitted to a hospital. All participants signed informed consent forms, and the G.S.V.M. Medical College Ethics Committee approved the study protocol.
Patient Selection
The study group consisted of patients above the age of 18 years old with T2DM. There were numerous factors we set as exclusionary criteria. These included all any cause of chronic liver disease, including viral infections (i.e., positivity for Hepatitis B/C) other than NAFLD, any history of hepatotoxic drug use (i.e., anti-tubercular treatment), and patients who were classified as significant alcohol consumers based on the recommendation guidelines set forth by the American Association for the Study of Liver Disease (A.A.S.L.D.). In patients without liver disease, the A.A.S.L.D. Recommends that women consume no more than one standard drink per day and that men consume no more than two standard drinks per day, with a standard drink containing 14 grams (g) of ethanol (EtOH) [16].
Moreover, any patients with congestive heart failure (CHF) were also excluded. All patients underwent detailed questioning about their past medical history and social history, as well as a full clinical physical examination. The findings were logged in a specially prepared proforma. All the patients underwent extensive lab testing using both blood and urine analyses. Tests conducted and values obtained included an electrocardiogram (E.C.G.), hemoglobin (Hb), total lung capacity (T.L.C.), diffusion lung capacity (DLC), and erythrocyte sedimentation rate (E.S.R.), urine microscopy, HbA1c, random blood glucose, alanine amino-transferase/aspartate aminotransferase (SGPT/ SGOT) ratio, serum bilirubin (total and differential), kidney function test, total serum protein, albumin, globulin, ultrasonography (U.S.G.) of the whole abdomen, and transient elastography.
Transient Elastography Fibro scan
The severity of NAFLD in patients was assessed using U.S.G. abdomen for confirming fatty liver, and transient elastography controlled attenuation parameter (C.A.P.) value for hepatic steatosis grading and E (kPa) value for liver fibrosis categorization as shown in Table 1 and 2. In addition, N.F.S. was also calculated using age, blood sugar, B.M.I., platelet count, albumin, and AST/ALT ratio for correlation. Diagnostic criteria for T2DM assessment included an HbA1c level >6.5 and two-hour plasma glucose >200mg/dl after 75gm glucose load. Cardiovascular risk was assessed using 10-year A.S.C.V.D., calculated using free online software M.D. Calc.
Table 1: Steatosis grade distribution of patients(n=55).
| Steatosis Grading E(CAP) | ||||
| Steatosis Grade (CAP value) | # of Patients | 95% CI | Reference Values | Severityof steatosis |
| S0 | 24(43.6%) | 30.6%-57.6% | <237> | Nosteatosis |
| S1 | 11(20.0%) | 10.9%- 33.4% | 237-259(5-33%) | Mildsteatosis |
| S2 | 9 (16.4%) | 8.2%- 29.3% | 259-291(33-66%) | Moderate steatosis |
| S3 | 11(20.0%) | 10.9%- 33.4% | >291 (less than 66 %) | Severe steatosis |
Table 2: Fibrosis grade distribution of patients (n=55).
| Fibrosis Grading E(kPa) | ||||
| Classification | # of Patients | 95% CI | Reference Values | Severity of fibrosis |
| F0 | 15 (27.3%) | 16.5% - 41.2% | < 5.5 | No fibrosis |
| F1 | 19 (34.5%) | 22.6% - 48.7% | 5.5-8 | Mild fibrosis |
| F2 | 9 (16.4%) | 8.2% - 29.3% | 8-10 (33-66%) | Moderate fibrosis |
| F3 | 7 (12.7%) | 5.7% - 25.1% | > 10-16(<66> | Severe fibrosis |
| F4 | 5 (9.1%) | 3.4% - 20.7% | >16 | Cirrhosis |
Data Analysis
Statistical analysis was accomplished using Statistical Package for Social Survey version 28 (S.P.S.S. Inc., Chicago, IL). The data obtained were analyzed using the chi-square test, Kruskal Wallis test, and Fisher exact test. A p-value <0>
Results
Demographic Characteristics
The mean age of all patients was 55.24±10.09 years (Range 35-78 years). The maximum number of patients were from the 51-60 age group (32.7%, n=18), and the minimum number of patients were from the 71-80 age group (3.6%, n= 2). Majority of patients were female (52.7%, n= 29).
Physical Examination Characteristics
The mean height (cm), weight (kg), waist-to-hip ratio (WHR) and BMI (kg/m²) of patients were 157.60±8.28, 61.78±12.12, 1.00±0.10 and 24.69±4.21 respectively. The distribution of BMI of patients were as follows: 3 (5.5%) of the patients had BMI of of less than 18.5 kg/m2, 12 (21.8%) had BMI of 18.5-22.9 kg/m2, 14 (25.5%) had BMI of 23.0-24.9 kg/m2, 20 (36.4%) had BMI of 25.0-29.9 kg/m2, 4 (7.3%) had BMI of 30.0-34.9 kg/m2 and 2 (3.6%) had BMI of 35.0-39.9 kg/m2.
The mean systolic blood pressure (S.B.P.) and diastolic blood pressure (DBP) were 132.76±16.44 mmHg and 76.18±11.63 mmHg.
Glucose and HbA1c levels
The mean postprandial blood sugar was 229.25±71.69 mg/dL, the mean fasting blood glucose was 147.15±40.15 mg/dL, and the mean HbA1c was 9.05±2.81%.
A.S.C.V.D. risk score & Assessments
The mean A.S.C.V.D. Risk score was 11.16±11.58. In males, the mean was 14.11±13.54, and in females, it was 8.52±8.93. Forty-two (76.4%) of the patients had fatty liver, and thirteen (23.6%) had no fatty liver, as shown in Table 3. The mean A.S.C.V.D. risk score in the fatty liver group was 10.43±11.25, and the mean A.S.C.V.D. risk score in patients without fatty liver was 13.53±12.78. There was no statistically significant difference between the groups regarding A.S.C.V.D. risk scores (W = 234.000, p = 0.446) or association (Point-Biserial Correlation of 0.11), as shown in Figure 1.
Figure 1: Strength of Association betweenASCVD & Fatty Liver (Point-Biserial Correlation= 0.11).
Table 3: Comparison of the 4 subgroups of the different steatosis grades in terms ofASCVD risk score (n=55).
| Comparison Between Steatosis Grades in Terms of ASCVD | ||||||
| ASCVD Risk Score | Steatosis Grade | Kruskal Wallis Test | ||||
| S0 | S1 | S2 | S3 | χ2 | p value | |
| Mean (SD) | 10.32 (10.96) | 11.81(12.97) | 19.28 (14.25) | 5.72 (4.81) | 6.874 | 0.076 |
| Median (IQR) | 7.85 (2.3-14.88) | 5 (2.85-15.55) | 12.2 (10.5-30.3) | 4.1 (1.75-7.7) | ||
| Range | 0.8 - 45.6 | 0.9 - 42.7 | 2.7 - 46 | 1.2 - 14.4 | ||
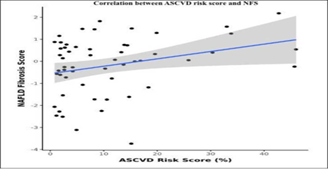
The mean N.F.S. was -0.18 ± 1.30. There was a weak positive correlation between A.S.C.V.D. Risk Score and N.F.S. (ρ = 0.27, p = 0.047), as shown in Figure 2.
Figure 2: Correlation betweenASCVD risk score and NFS (n = 55).
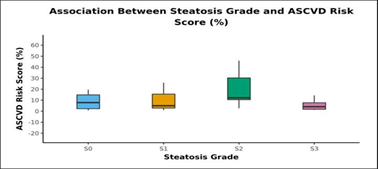
The mean of FibroScan (C.A.P.) was 245.82±50.89. Twenty-four (43.6%) of the patients had steatosis grade S0, 11 (20.0%) of the patients had steatosis grade S1, 9(16.4%) of the patients had steatosis grade S2 and 11 (20.0%) of the patients had steatosis grade S3 as shown in Table 1.
The mean A.S.C.V.D. risk scores in S0, S1, S2, and S3 were 10.32±10.96, 11.81±12.97, 19.28±14.25, and 5.72 ±4.8, respectively, as shown in Table 4. There was no statistically significant difference between the groups regarding the A.S.C.V.D. risk score for the steatosis grade (χ2=6.874, p=0.076). Figure 3 shows the association between steatosis grade and A.S.C.V.D. Risk score.
Table 4: Post-Hocpairwise tests for Kruskal-Wallis test performed using Dunn Test method with Sidak correction.
| Pairwise Comparison | |
| Pairwise Comparison of Subcategories of Steatosis Grade | Adjusted P Value |
| S0 - S1 | 1 |
| S0 - S2 | 0.292 |
| S1 - S2 | 0.583 |
| S0 - S3 | 0.819 |
| S1 - S3 | 0.814 |
| S2 - S3 | 0.055 |
Figure 3: Strength of Association (Kendall's Tau) = 0.01
The mean Fibro Scan (kPa) was 9.05±7.24. Fifteen (27.3%) of the patients had a Fibrosis Grade of F0, 19 (34.5%) of the patients had a Fibrosis Grade of F1, 9 (16.4%) of the patients had a Fibrosis Grade of F2, 7 (12.7%) of the patients had Fibrosis Grade of F3 and 5 (9.1%) of the patients had Fibrosis Grade of F4 as shown in Table 2. There was a moderate positive correlation between A.S.C.V.D. risk score and FibroScan (kPa), and this correlation was statistically significant (ρ = 0.47, p = = less than 0.001), as shown in Figure 4.
Figure 4: Correlation between ASCVD risk score and Fibroscan: E (KPa) (n=55).
Discussion
Given the strong association between NAFLD and T2DM, assessing the two conditions' independent cardiovascular effects remains challenging. To summarize, our study implemented the use of fifty-five patients, all with known cases of T2DM for at least five years. These patients were evaluated and investigated for NAFLD using a USG of the abdomen, NFS, and FibroScan results. ASCVD was calculated and analyzed for association with NAFLD.
Previous studies have shown that NAFLD could be an independent cardiovascular disease risk factor. Examples are as follows:
Targher et al. screened 2839 diabetic patients and found NAFLD patients had remarkably (p<.001) higher rates for the gender-adjusted prevalence of coronary (26.6 vs. 18.31%), cerebrovascular (20% vs. 13.3%), and peripheral vascular disease than their counterparts without NAFLD (15.4 vs. 10%) [2].
Kalra et al. (2013) conducted a study to determine frequency and risk factors in Type II DM patients. Out of 924 patients (335 females/569 males) in the age group of 15-85 years were identified as having NAFLD. There was no significant difference in ASCVD scores in fatty and non-fatty liver groups [17].
Toung et al. conducted a cross-sectional design in T2DM adults. In this study, liver steatosis and fibrosis were assessed by Fibro Scan. NAFLD was diagnosed if CAP > 233 dB/m (steatosis > 5%). They found that 307 T2DM patients qualified for the study's criteria. The prevalence of NAFLD in T2DM patients based on Fibro Scan was 73.3%. Both mild, moderate, and severe steatosis rates were 20.5%, 21.8%, and 30.9%, respectively. The prevalence of significant fibrosis (≥ F2), advanced fibrosis (≥ F3), and cirrhosis (F4) was 13.0%, 5.9%, and 3.6%, respectively. They concluded that their study supports screening for NAFLD and evaluating the severity of liver fibrosis in T2DM patients [18]. The mean Fibro Scan CAP of our study population was 245.82 ± 50.89. 24 (43.6%) of the participants had Steatosis Grade: S0. 11 (20.0%) of the participants had Steatosis Grade: S1. 9 (16.4%) of the participants had Steatosis Grade: S2. 11 (20.0%) of the participants had Steatosis Grade: S3.
There was a significant difference between the two groups in Fibro scan CAP (W = 383.500, p = 0.029), with the median Fibro scan CAP being highest in the fatty liver group. The strength of association was correlated using a Point-Biserial Correlation of 0.3, showing a medium effect size. However, there was no significant difference between the groups regarding ASCVD Risk Score (%) (W = 374.500, p = 1.000).
There was a moderate positive correlation between ASCVD Risk Score (%) and Fibro scan: E (KPa), and this correlation was statistically significant (rho = 0.47, p = less than 0.001). For every 1 unit increase in ASCVD Risk Score (%), the Fibro scan: E (KPa) increases by 0.19 units. Conversely, for every 1 unit increase in Fibroscan: E (KPa), the ASCVD Risk Score (%) increases by 0.48 units.
Golabi et al. studied the correlation between cardiovascular risk and NAFLD in patients with T2DM. Among 1,262 subjects with NAFLD (47.9% men; 41.2% white; mean age of 56.3 years), the high risk for cardiovascular disease was 55.9%, and 4.8% had advanced fibrosis. After a median follow-up of 17.7 years, 482 subjects (38.2%) died of prevalent causes, of whom 382 (79.3%) had a high risk for cardiovascular disease. The unadjusted overall and cardiac-specific mortality were higher for patients with NAFLD who had an increased risk for cardiovascular disease than subjects with NAFLD with a low risk for cardiovascular disease (57.3% vs. 16.8% for overall mortality; 16.4% vs. 3.5% for cardiovascular mortality). After controlling for risk factors associated with mortality, a higher risk for cardiovascular disease was associated with a 42% higher overall mortality rate (adjusted HR [aHR] of 1.42; 95% confidence interval [CI], 1.05-1.91) and twice the risk of cardiovascular mortality (aHR, 2.02; 95% CI, 1.12-3.65). Adjusted population attributable fractions (PAFs) were 11.4% for overall mortality and 44.9% for cardiovascular mortality [19]. The mean ASCVD Risk Score (%) was 11.16 ± 11.58. The mean (SD) of ASCVD Risk Score (%) in the male subject group was 14.11 (13.54). The mean (SD) of ASCVD Risk Score (%) in the female group was 8.52 (8.93). There was a moderately positive correlation between Fibro Scan E (KPa) and ASCVD Risk Score (%), and this correlation was statistically significant (rho = 0.47, p = less than 0.001).
In summary, NAFLD is highly prevalent, with a proportion of these patients developing liver disease so timely screening with Transient elastography using Fibro Scan with C.A.P. can assess both liver steatosis and fibrosis simultaneously, which can halt further complications from developing. On the other hand, NAFLD patients succumb to death most commonly due to cardiovascular complications and predictive models, such as A.S.C.V.D. risk score can provide an easy tool to identify patients with NAFLD who are at the greatest risk for CVD NAFLD act as a marker for CVD, and early interventions for it can improve long-term cardiovascular outcomes. Overall, this work can have a significant impact on clinical and public health. However, further research is needed to validate these findings. Although meaningful conclusions may be drawn from this study, a significant limitation of our study is the small sample size, and future studies should be carried out using larger patient populations. In addition, in our study, we did not perform a histopathological examination for confirmation of non-alcoholic steatohepatitis and A.S.C.V.D. risk score is a reliable assessment tool, but its generalizability and applicability in our study of patients are debatable.
Conclusion
Our study revealed the Prevalence of fatty liver on abdominal U.S.G. in 72% of the patients (42/55). However, there was no significant difference in A.S.C.V.D. Risk score in both fatty and non-fatty liver groups. Additionally, N.F.S. correlated significantly with the A.S.C.V.D. risk score. There was no significant difference between A.S.C.V.D. Risk score in the steatosis and non-steatosis groups. There was a moderate positive correlation between A.S.C.V.D. the risk score and FibroScan E, and this correlation was statistically significant. However, these results suggest that identifying NAFLD in T2DM may help CVD risk prognosis and thus, have substantial management implications. Identifying people with NAFLD would highlight a subgroup of diabetic patients who may benefit from more intensive preventative treatment and cardio-protective measures to decrease their risk of future CVD.
Acknowledgement
This inclusion aims to respectively document and provides full credit for the contributions of the first and second authors, whose efforts are comparable in conducting this publication.
References
- Kudaravalli P, John S. Nonalcoholic Fatty Liver. In: StatPearls Treasure Island (FL): StatPearls Publishing.
Publisher | Google Scholor - Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L. (2007). Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 30(5):1212-1218.
Publisher | Google Scholor - Angulo P. (2002). Nonalcoholic fatty liver disease. N Engl J Med., 346(16):1221-1231.
Publisher | Google Scholor - McCullough AJ. (2006). Pathophysiology of Nonalcoholic Steatohepatitis. J Clin Gastroenterol. 40(1):S17-S29.
Publisher | Google Scholor - Marchesini G, Marzocchi R, Agostini F, Bugianesi E. (2005). Nonalcoholic fatty liver disease and the metabolic syndrome. Curr Opin Lipidol. 16(4):421-427.
Publisher | Google Scholor - Day CP. (2006). Non-alcoholic fatty liver disease: current concepts and management strategies. Clin Med (Lond). 6(1):19-25.
Publisher | Google Scholor - Clark JM, Brancati FL, Diehl AM. (2003). The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol, 98(5):960-967.
Publisher | Google Scholor - Bedogni, G., Miglioli, L., Masutti, F., Tiribelli, C., Marchesini, G. et al. (2005). Prevalence of and risk factors for non-alcoholic fatty liver disease: The Dionysus nutrition and liver study. Hepatology, 42:44-52.
Publisher | Google Scholor - Browning, J.D., Szczepaniak, L.S., Dobbins, R., Nuremberg, P., Horton, J.D., et al. (2004), Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology, 40:1387-1395.
Publisher | Google Scholor - Caussy, C., Aubin, A. & Loomba, R. (2021). The Relationship Between Type 2 Diabetes, NAFLD, and Cardiovascular Risk. Curr Diab Rep 21:15
Publisher | Google Scholor - Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N. et al. (2019). The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol., 71(4):793-801.
Publisher | Google Scholor - Doycheva I, Cui J, Nguyen P, Costa EA, Hooker J. et al. (2015). Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther., 43(1):83-95.
Publisher | Google Scholor - Zhou YY, Zhou XD, Wu SJ, Hu XQ, Tang B. et al. (2008). Synergistic increase in cardiovascular risk in diabetes mellitus with nonalcoholic fatty liver disease: a meta-analysis. Eur J Gastroenterol Hepatol. 30(6):631-636.
Publisher | Google Scholor - Targher G, Lonardo A, Byrne CD. (2018). Nonalcoholic fatty liver disease and chronic vascular complications of diabetes mellitus. Nat Rev Endocrinol. 14(2):99-114.
Publisher | Google Scholor - Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ. (2005). Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology, 41(6):1313-1321.
Publisher | Google Scholor - Lucey MR, Im GY, Mellinger JL, Szabo G, Crabb DW. (2020). Introducing the 2019 American Association for the Study of Liver Diseases Guidance on Alcohol-Associated Liver Disease. Liver Transpl., 26(1):14-16.
Publisher | Google Scholor - Kalra S, Vithalani M, Gulati G, Kulkarni CM, Kadam Y, et al. (2023). Study of prevalence of nonalcoholic fatty liver disease (NAFLD) in type 2 diabetes patients in India (SPRINT). J Assoc Physicians India, 61(7):448-453.
Publisher | Google Scholor - Tuong TTK, Tran DK, Phu PQT, Hong TND, Dinh TC, Chu DT. (2020). Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan. Diagnostics (Basel). 10(3):159.
Publisher | Google Scholor - Golabi, P., Fukui, N., Paik, J., Sayiner, M., Mishra, A., & Younossi, Z. M. (2019). Mortality Risk Detected by Atherosclerotic Cardiovascular Disease Score in Patients with Non-alcoholic Fatty Liver Disease. Hepatology communications, 3(8):1050-1060.
Publisher | Google Scholor