Opinion Article
An Alternative to Current Orthodontic Retention Appliances
- Parmjit Singh *
- Simon Ash
Department of Orthodontics, University of Ulster Faculty of Life and Health Sciences College of Medicine and Dentistry, UK.
*Corresponding Author: Parmjit Singh,Department of Orthodontics, University of Ulster Faculty of Life and Health Sciences College of Medicine and Dentistry, UK.
Citation: P. Singh, S. Ash. (2024). An Alternative to Current Orthodontic Retention Appliances. Dentistry and Oral Health Care, Biores Scientia Publishers 3(1):1-6. DOI: 10.59657/2993-0863.brs.24.025
Copyright: © 2024 Parmjit Singh, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 23, 2023 | Accepted: December 05, 2023 | Published: January 05, 2024
Abstract
There are considerable challenges in relation to post-treatment orthodontic retention. Acrylic and vacuum-formed thermoplastic devices along with fixed bonded retainers are routinely proposed at the end of a course of treatment but these are not without their limitations. This brings into question the current strategies in use today and the need for an ideal long-term retainer that can be used for a ‘lifetime’. Cast chrome cobalt removable devices are presented as a possible solution. These are both robust and able to withstand the test of time.
Keywords: chrome cobalt; economics of orthodontic delivery systems; retention; retainers; stability
Introduction
Teeth move throughout life. As early as the 1900s, the ‘father of modern orthodontics’ stated that post-treatment challenges can be more demanding than the initial interventional treatment itself [1]. Soon after, Oppenheim was clear that the retention phase was not just a problem but was the problem of the entire orthodontic treatment process and stated, “retention is the most difficult problem in orthodontia; in fact, it is the problem” [2]. All patients present with their teeth in a unique position of dynamic balance [3]. This may not be aesthetically or functionally ideal but nevertheless these positions are stable at a given moment in time. Tooth movement occurs not only in individuals who have completed a course of orthodontic treatment but also in those who have naturally aligned teeth. Any changes, whether deliberately introduced or otherwise, will alter the state of balance and may lead to further tooth movement. If changes to tooth positions are not desired, then teeth need to be maintained in that position artificially for as long as the host wants to keep their teeth in their current positions. Management approaches focused on delivering a course of orthodontic treatment and limited aftercare, often for no more than a few years of follow-up [4], need to be revisited. Lifelong solutions need to be explored to ensure long-term stability of tooth positions.
Current trends
The current recommendation is retention for life following orthodontic treatment [5], and in the absence of this, the patient would need to accept a degree of relapse as well as the changes that occur with the passage of time. The degree of relapse can be highly variable, with few predictors of which cases will largely remain stable and which will undergo significant changes [6]. Retention appliances can be considered as removable or fixed. Vacuum-formed thermoplastic retainers or Hawley acrylic and stainless-steel removable retainers are normally prescribed for indefinite nocturnal wear following active orthodontic treatment. Fixed lingual /palatal retainers, also referred to as bonded retainers, are adhered to the inner surfaces of anterior teeth in one or both dental arches and are intended to remain indefinitely. During the pre-treatment consent stages, patients are advised of the likelihood of orthodontic post-treatment relapse and the need for a commitment to indefinite retention for life or until such time as they are prepared to accept unplanned tooth movements that may include some relapse [7]. Once active treatment and a limited period of supervised retention are concluded, orthodontists, having completed their duty of care discharge the patient to the referring dentist or general dental practitioner [8]. Rarely does the orthodontist offer indefinite lifetime supervision of their treated patients and replacement or repair of worn-out retainers. General dental practitioners, though committed to provide for the patient’s dental needs, are often reluctant to assume the responsibility for long-term supervising of the treated patient [9]. This may be due to the dentist’s contention that since they have not prescribed or supplied the retainers, they are not in a position to assume a duty of care for them [10]. Another possible explanation is that retainers are beyond the skill set of the dentist. Patients can then be left to their own devices to find a dentist to manage their retention and oral devices. Without regular professional supervision and inspection, patients will only seek further treatment once they notice tooth movement and relapse with a sizable proportion of adult patients then seeking treatment for a second time [11]. The consensus of clinical experience supported by research has shown that once aligned, teeth may be maintained with regular removable retainer wear indefinitely, with attempts being made to widely disseminate this information to orthodontic patients [12].
Current appliances and their limitations
Plastic, thermoplastic and acrylic as used in dentistry have historically been convenient, readily available, and inexpensive in the short-term. They should continue to be considered for short to medium term use due to their fragility, weakness in thin section, difficulty in cleaning, plaque accumulation, retention of oral microflora and other shortfalls [13]. Stainless steel bows and retention cribs included into acrylic devices such as in the Hawley or Begg retainers are also subject to distortion and work hardening fracture [14]. The acrylic and stainless steel is liable to fracture at the plastic metal interface. Over time the physical nature of the plastics and acrylic, when exposed to the oral environment, degrade, become brittle and are liable to fracture. It is of note that dental laboratories take no responsibility for HTM 01-05 sterilising of manufactured devices leaving this task to the clinicians [15]. Due to the nature of the fabrication materials, dentists are only able to disinfect these appliances before use. Vacuum-formed thermoplastic aligners, as well as 3D printed aligners are increasingly popular as the appliance of choice amongst orthodontists, dentists, and their patients [16]. They have a valuable role in achieving desired outcomes within defined time scales. These devices or subsequently made vacuum-formed retainers or those that are 3D printed are unsuitable as long-term retainers. Where arch expansion has occurred, the inherent transverse flexibility of the vacuum thermoformed retainers limits their ability in maintaining arch width expansion. However, there is emerging evidence that modifications to a vacuum-formed retainer may offer some benefit to cases where expansion has taken place, at least in the short-term [17]. Fixed bonded retainers are adhered to the inner surfaces of the anterior teeth only (with a few exceptions) and therefore have no contact with or influence over the alignment of teeth in the buccal segments. The placing of these retainers is challenging, technique sensitive [18, 19], and is rarely taught in the undergraduate curriculum. “Daisy chaining” a group of teeth together introduces plaque and calculus traps around the teeth and retainer wires [20]. Plaque will still accumulate with the well-established adverse effects on the gingival tissues and supporting dental structures, even with fastidious cleaning regimen with water picks, interdental cleaners floss, oral disinfectants, and brushing. In addition, distorted fixed bonded retainer wire may inadvertently introduce unwanted tooth movements [21]. Sharp uncovered wires may cause soft tissue irritation and trauma and repairs of one or more fractured elements of the fixed bonded retainer can be challenging. Whether one ascribes to the philosophy of occlusion, occlusal balancing, and functional dynamic occlusion or not, there is little doubt that the forces of occlusion are enormous and are potentially very destructive especially where these forces are directed to one or a few teeth. Having undertaken extensive and expensive orthodontics it would seem logical to institute long-term measures to protect the end results from relapse and damage by jaw parafunction. Vacuum-formed thermoplastic retainers and bite guard occlusal splints are often provided for risk patients, but these suffer from the limitations related to retainers already described. As the acrylic or thermoplastic material wears or partially disintegrates with use, adverse tooth movement and eruptions can occur. A short-term remedy may have long-term adverse undesirable consequences for the patient.
Possible solutions for long-term retention
There are several options available for long-term retention strategies, however, all of these rely on a high level of patient compliance with the retention protocol. Continuing with the status quo cannot be ignored given that this has been taking place for many decades. The limitations of this model have already been described. A subscription model where patient’s pay a monthly fee to the dentist or orthodontist, in return for a regular inspection of their fixed bonded retainers and replacement of their removable retainers. Already, the direct-to-consumer aligner company Smile Direct Club offers automated replacement of removable retainers for a set fee every six months (www.smiledirectclub.co.uk/en-gb/) [22]. Whilst such a model may already exist in some practices as well, it has the limitation that as more and more patient’s finish treatment and subscribe, a larger proportion of clinical time may be taken up by retainer review and replacement appointments. The use a near ideal appliance to act as a removable retainer. Ideal properties of an appliance for long-term intra-oral use Whilst an ideal appliance may not exist, one that fulfils as many of the following requirements would be desirable. Accessible to and manufactured by most dental laboratories. Robust and strong in thin section so that it does not distort or wear with long-term use. Nonporous and discourage the ingress of oral micro flora. Biocompatible with the oral environment, not leach or degrade with time and have a proven long-term safety record for use in the mouth. Compatible with dental tissues and dental restorative materials, prosthesis, or other elements in the oral cavity. Achieve the desired management objectives, that is, long-term post-treatment retention; provide inter-occlusal barrier to protect the teeth in the presence of jaw parafunction; distribution of occlusal loading forces down the long axis of the teeth; spread the occlusal biting forces evenly over the dentition. Tooth borne and kept free of the tooth supporting tissues as far as possible. Sterilisable in line with current best practice prior to delivery to the patient (Health Technical Memorandum 01-05, 2021) [15]. Tolerate minor chairside adjustments. Minimal encroachment upon tongue space. Minimal interference with speech and oral function. Allow normal unimpeded saliva flow around the device and within the mouth. Easily removed by the wearer for cosmetic reasons and ease of cleaning of the teeth, oral tissues, and the device itself. Easy to clean using domestic materials and be domestic dishwasher proof. Minimal maintenance and infrequent replacement. Inexpensive over the lifetime of the appliance. Minimal or no risk to the patient’s health and wellbeing. A comfortable, pleasant patient experience.
A possible solution
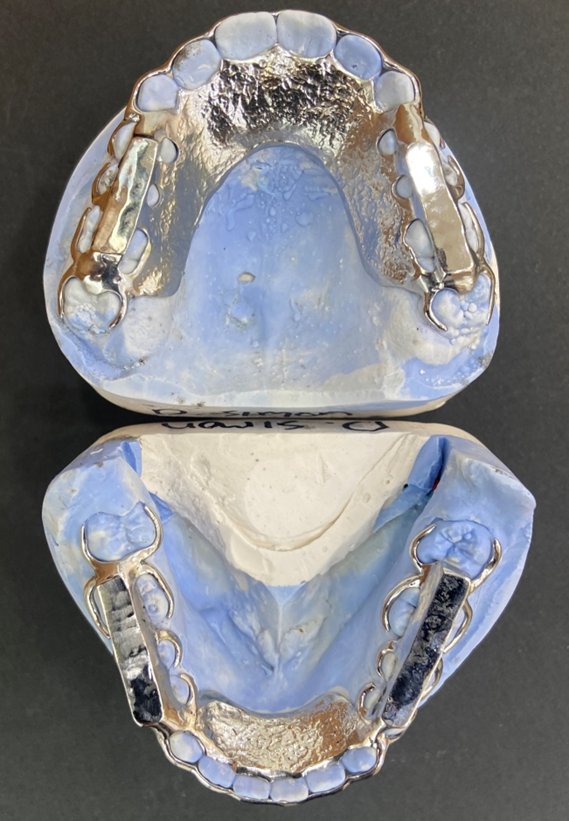
Nearly all the above requirements can be fulfilled by chrome cobalt removable retainers. These have been described along with their possible role in the retention regimen [13], although the design has since been modified. Chrome cobalt is a well-established dental material familiar to many dental laboratories, is robust and strong, can be sterilised, is nonporous and biocompatible as well as being compatible with many other dental materials. All standing teeth are included in the design so that no tooth is left uncontrolled. Close fitting labial bows are placed on the labial surfaces of anterior teeth with a reciprocating lingual bar or lingual plate in the lower jaw. In the upper jaw the close-fitting labial bow is reciprocated by the palatal plate (Figure 1a).
Figure 1a: Close fitting labial bows with reciprocating lingual/palatal plates. Note every posterior tooth has been clasped and there are circumferential clasps around the terminal molars teeth to retain arch length.
Wherever possible the buccal teeth are clasped and are reciprocated by the lingual or palatal plates or clasps. Circumferential clasps are placed where possible around the terminal molars or teeth to retain arch length. The buccal occlusal surfaces have continuous chrome bite plates which are occlusally balanced against the opposing appliance (Figure 1b).
Figure 1b: The buccal occlusal surfaces have continuous chrome bite plates and clasps on every posterior tooth.
The aim is to protect the cusps and crowns of teeth and distribute occlusal loads across the dental arch. By virtue of this design, the teeth are encased in the chrome cobalt skeleton limiting their potential movement and there is minimal soft tissue support for the appliance. For the wearer, there is minimal encroachment upon tongue space so speech in minimally effected, saliva flow is unimpeded, the appliance can be easily removed and inserted, and cleaning can extend to the appliance being placed in a dishwasher (Figures 2a-e).
Figures 2a-e: Appliance in situ showing labial bows and lingual/palatal plates. Note minimal encroachment upon tongue and the chrome bite plates which are occlusally balanced against the opposing appliance.
There is minimal maintenance of the appliance, and its long-lasting nature makes it inexpensive over the lifetime of the appliance.
Practical considerations
The clinical records should ideally include a facebow transfer registration so that the chrome technician can mount the work on a semi adjustable articulator to establish occlusal balancing.
The frequency of nocturnal retention is unique to the individual with significant variability form one person to another. In response to the usual question “how many nights or how often do I need to wear the retainers?” the advice might be to gradually reduce the frequency of wear until the retainers feel unusually tight and then increase the frequency again until the retainers can be inserted without causing any discomfort. This has the advantage of transferring responsibility for wear to the patient. The limitations of the appliance must be acknowledged. It is essential that the chrome cobalt devices be constructed at the same time and be worn as a pair or if only one is worn then it must be opposed by protective device in the opposing jaw as chrome cobalt may in the presence of jaw parafunction or bruxism cause damage to unprotected enamel. Given the rigidity of the appliance, if some tooth movement occurs then the appliance can stop fitting and chrome cobalt is a hard material that can only be minimally adjusted. However, if the teeth move significantly and the chrome retainers fail to fit, then aligners can be used to re-establish alignment before returning to the chrome retainers. Similarly, given the longevity of the appliance, the wearer may have dental restorative work undertaken and the appliance would need to be checked to ensure any restoration has not unseated the appliance. Patients must ensure that they take their retainers with them on dental visits as any alteration in the dental anatomy will inhibit the seating of the rigid metal retainers. The appliance may also need to be remade should there be the eruption of further teeth, for example, third molars or there being major restorative work undertaken.
Conclusion
Existing retainers, both removable and fixed bonded are not without their limitations, particularly in the long-term. Chrome cobalt retainers, that can be constructed to snugly control every tooth are a possible option that overcomes many of the limitations of retainers that are currently in widespread use.
Declaration
Acknowledgements
None
Declaration of Interests
Simon Ash is the inventor of cast chrome cobalt retainers manufactured by Som Nowell Limited. This is one of several dental companies that manufacture cast chrome cobalt appliances. He is no longer a director or employee of Som Nowell Limited.
References
- Bayazit EÖ, Başeren M, Meral E. (2023). Clinical comparison of different glass ionomer-based restoratives and a bulk-fill resin composite in Class I cavities: A 48-month randomized split-mouth controlled trial. Journal of dentistry, 131:104473.
Publisher | Google Scholor - Pratap B, Gupta RK, Bhardwaj B, Nag M. (2019). Resin based restorative dental materials: Characteristics and future perspectives. Japanese Dental Science Review, 55(1):126-138.
Publisher | Google Scholor - Borgia E, Baron R, Borgia JL. (2017). Quality and Survival of Direct Light-Activated Composite Resin Restorations in Posterior Teeth: A 5- to 20-Year Retrospective Longitudinal Study. Journalof Prosthodontics, 28(1):195-203.
Publisher | Google Scholor - ManhartJ. (2015). Cusp replacement with an extensive posterior direct restoration using a nanohybrid bulk-fill ormocer. International Dentistry – African Edition, 9(3):6-16.
Publisher | Google Scholor - KoubiSA, Brouillet JL, Pignoly C. (2005). Restaurations esthétiques postérieures en technique directe. EMC-Odontologie, 1(4):340-347.
Publisher | Google Scholor - Coelho A, Amaro I, Rascão B, Marcelino I, Paula A, Saraiva J, Spagnuolo G, Ferreira MM, Marto CM, Carrilho E. (2020). Effect of cavity disinfectants on dentin bond strength and clinical success of composite restorations—a systematic review of in vitro, in situ and clinical studies. International Journal of Molecular Sciences, 22(1):1-27.
Publisher | Google Scholor - Fibryanto E, Suprastiwi E, MeidyawatiR, Gunawan HA, Herda E. (2019). The Effect of Sodium Hypochlorite Irrigation on Dentin’s Collagen and Shear Bond Strength of Composite Resin to Dentin. Journal of International Dental & Medical Research, 12:111-116.
Publisher | Google Scholor - RandolphLD, PalinWM, Leprince JG. (2018). Composition of dental resin-based composites for direct restorations. Dental Composite Materials for Direct Restorations, 11-24.
Publisher | Google Scholor - Veloso SRM, Lemos CAA, De Moraes SLD, Do Egito Vasconcelos BC, Pellizzer EP, De Melo Monteiro G. (2019). Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clinical oral investigations, 23:221-233.
Publisher | Google Scholor - Meerbeek B, Yoshihara K, Van Landuyt K, Yoshida Y, Peumans M. (2020). From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J Adhes Dent, 22(1):7‑34.
Publisher | Google Scholor - Chandrasekhar V, RudrapatiL, Badami V, Badami V, Tummala M. Incremental techniques in direct composite restoration. Journal of conservative dentistry, 20(6):386.
Publisher | Google Scholor - Nikfarjam F, Beyer K, König A, Hofmann M, Butting M, Valesky E, Kippenberger S, Kaufmann R, Heidemann D, Bernd A, Zoller NN. (2016). Influence of Bio dentine®-a dentine substitute-on collagen type I synthesis in pulp fibroblasts in vitro, 11(12):1‑20.
Publisher | Google Scholor - AromaaMK. ,Vallittu PK. (2018). Delayed post-curing stage and oxygen inhibition of free-radical polymerization of Di methacrylate resin. Dental Materials, 34(9):1247-1252.
Publisher | Google Scholor - Rathi SD, Nik hade P, Chandak M,Motwani N, Rathi C, Chandak M. (2020). Microleakage in composite resin restoration-a review article. J Evol Med Dent. Sci, 9:1006-1011.
Publisher | Google Scholor