Research Article
Age and Gender Specific Features of the Spinal Canal in the Ukrainian Population
1.Department of Anatomy and Genetics, COM Alfaisal University, Saudi Arabia.
2.Anatomy Department, Luhansk State Medical University, Ukraine.
*Corresponding Author: Volodymyr Mavrych, Department of Anatomy and Genetics, COM Alfaisal University, Saudi Arabia.
Citation: O Bolgova, A Eryomin, V Mavrych. (2023). Age and Gender-specific Features of the Spinal Canal in the Ukrainian Population. International Clinical and Medical Case Reports, BioRes Scientia Publishers. 3(1):1-10. DOI: 10.59657/2993-0227.brs.24.030
Copyright: © 2024 S. Volodymyr Mavrych, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 19, 2023 | Accepted: January 04, 2024 | Published: January 25, 2024
Abstract
Advancements in medical technology and broader examinations of distinct populations yield an increasingly comprehensive understanding of the human spinal anatomy. Studies on the lumbar canal dimensions have uncovered intriguing and crucial findings relevant to clinical procedures and population health. This study aimed to provide an extensive, accurate database of the spinal canal size, focusing on age-related changes and gender-related differences in the Ukrainian population. Spinal canal dimensions of lumbar vertebrae from 211 individuals (0-90 years old) were measured. ANOVA and independent samples t-tests were utilized for statistical analysis of the collected data. Our data indicate that the transverse diameter of the spinal canal the most significantly increases in the first year of the postnatal life by 31% and the anterior-posterior diameter by 13.9% in the teenager group (by the age of 16). After this age, we did not find significant changes in the spinal canal sizes. In all age groups, spinal canal transverse diameter increased in the caudal direction (maximum at L5 level), and the smallest anterior-posterior diameter was on L3 level, increasing up to L1 and down to L5 levels. Vertebral foramina significantly varied in shape depending on the age group: in newborns, it has a drop shape; in children with a broad longitudinal diameter, it takes the form of an oval; and in teenagers, it takes the shape of a triangle. In conclusion, this study contributes to the comprehension of the features unique to the human spinal canal by providing a comprehensive database of spinal canal dimensions in the Ukrainian population in relation to age and gender, comparing this information with the architecture of the spinal canal in different ethnic groups, which is important in improving methods for identifying and managing disorders specific to the lumbar area that differ among various racial and ethnic groups.
Keywords: Ukrainian population; lumbar vertebrae; spinal canal; vertebral dimensions; lumbar spine
Introduction
Spinal stenosis compresses nerve roots, leading to symptoms such as pain, numbness, and weakness, primarily affecting the cervical and lumbar regions. The condition is mainly linked to aging and can recover without surgery, but in some cases, it can result in herniated discs or nerve root compression [1]. Lumbar spinal stenosis is often due to degenerative disc disease, with increasing age and muscle fat infiltration correlating with lumbar spinal canal volume [2]. It has been suggested that it be reconsidered as a syndrome with developmental roots rather than a degenerative condition [3, 4]. Machine learning techniques have found multifactorial lumbar spine characteristics to predict symptomatic degenerative lumbar spinal stenosis [5]. Lumbar spinal canal stenosis, a leading cause of lower back pain, is usually characterized by decreased spinal canal and vertebral body dimensions [6]. A study showed that canal dimensions and canal-body ratio are smaller in elderly male patients [7]. A morphometric analysis found gender to be a significant determinant of lumbar vertebral dimensions [8]. Another study revealed alterations in canal dimensions due to the upright position of the spine, making imaging studies capturing weight-bearing changes valuable for understanding lower back pain causes [9]. The latest research findings delve into the effectiveness of different surgical approaches, including Anterior Lumbar Interbody Fusion, which showed improvements in clinical and radiological parameters [10]. Research highlights the learning necessity of endoscopic decompression for lumbar canal stenosis, with decreasing operative time and intraoperative complication rates [11]. Disc herniation in adolescents requiring surgical treatment has been linked to smaller dimension of spinal canal [12]. These studies depict how patient-specific anatomy and the surgeon's expertise play significant roles in determining the best operative approach and predicting the outcomes.
Surgical management has evolved with minimally invasive techniques like complete endoscopic decompression surgery, showing benefits over traditional decompression [13]. Tandem spinal stenosis has shown quality-of-life improvements after surgical interventions [14]. The choice of procedures relies heavily on detailed radiographic findings [15]. Advancements in medical technology and broader examinations of distinct populations yield an increasingly comprehensive understanding of the human spinal anatomy. Studies focusing on the lumbar canal dimensions have uncovered intriguing and crucial findings relevant to clinical procedures and population health. A study conducted in 2021 investigated the evolution of lumbar canal dimensions across generations and the impact of ethnicities on these measurements. This retrospective review utilized computed tomography reconstructions from two demographic cohorts: older group and younger group. The dimensions measured included the cross-sectional area and anterior-posterior diameter of the lumbar bony canal. The analysis of 918 patients showed that the older generation had significantly larger diameters across all lumbar levels than the younger generation. Furthermore, considerable differences surfaced in the cross-sectional area and anterior-posterior diameter among various ethnicities. These results indicate that comprehensive studies on typical anatomical dimensions within specific geographical populations are crucial, and they elucidate significant interethnic differences in spinal dimensions [16]. In the clinical world, an accurate understanding of anatomical lumbar dimensions is particularly essential in performing infant lumbar punctures. To this end, a prospective observational study was conducted 2022 using point-of-care ultrasound. The influence of posture on lumbar dimensions was investigated, examining whether the seated position significantly impacts lumbar dimensions in infants aged 12 months or younger compared to the lateral decubitus position. Despite prior data suggesting the supremacy of seated position measurements in lumbar punctures for preterm neonates, older children, and adults, the study found no substantial difference between the two positions [17]. Another study delved into early life development and growth of the lumbar spinal canal, evaluating 715 lumbar vertebrae from a collection of skeletons. This study stressed that growth potential concerning the midsagittal diameter and cross-sectional area significantly diminishes during infancy [18]. A comprehensive study reviewed skeletal samples from a cemetery, finding that growth timelines for different diameters of the lumbar vertebral canal varied. This research determined that the midsagittal diameter in children reached adult size by ages 3-5 years, while the interpedicular diameter expanded gradually, completing its development around 17 years of age [19]. The other study, combining data from over a thousand patients, also concluded that spinal canal development is completed by age 17. This study observed considerable variability in spinal canal size during development and determined that the cross-sectional area and depth were smallest at L3, subsequently enlarging cranially and caudally [20]. Delving deeper into the development of paediatric lumbar vertebral structures, a 2021 retrospective study analysed CT scans of 102 skeletal samples aged between 1 and 19 years. Sexual dimorphism and variations across different vertebral levels were noted as significant considerations [21]. A comprehensive investigation in 2014 studied vertebrae from 212 individuals across an extensive age spectrum to provide a broad database on vertebral body size. Findings suggested that while the vertebral body size remained independent of sex, it was strongly correlated with age, with two primary growth peaks: first in children aged 1-7 years and then in teenagers aged 13-16 years [22]. Two comparative studies on Indian and Pakistani populations substantiate the demographic variability in spinal dimensions. Indian research involving 302 patients and Pakistani research on 49 patients discovered that dimensions of the vertebrae and the bony spinal canal were generally more prominent in males [23,24]. Finally, two retrospective studies conducted in Western Switzerland started addressing the need for comprehensive data for this region. One study involved 254 patients born between 1940-1949 and 1970-1979, while the other involved 1050 subjects from three different ethnic groups. Despite an overall increase in body height across generations, a decrease in osseous lumbar spinal canal dimensions was recorded. The results suggested that while perinatal factors might contribute, cervical and lumbar bony spinal canals were smaller in the younger cohorts [25,26]. A detailed understanding of the lumbar vertebral canal and the vertebral body's morphometric characteristics is essential for clinical and bio-archaeological investigations due to its implications for spinal health, surgery, and device development.
However, establishing comprehensive growth standards for these vertebral components remains a significant objective, given discrepancies in the literature and a need for more sufficient data on their entire developmental timeline. This study aimed to provide an extensive, accurate database of the spinal canal size, focusing on age-related changes and gender-related differences in the Ukrainian population.
Materials and Methods
This study utilized a collection of 211 regular lumbar spine specimens gathered from diseased residents of Luhansk City in Ukraine. The study was approved by the Bioethics Committee of Luhansk State Medical University (3/10112005) and the MPH of Ukraine (2000/20.23.23). Lumbar vertebrae (L1 - L5)from 106 male and 105 female individuals spanning an age range from 0 to 88 years, with an average age of 40-year-old were measured. All specimens were sourced from deceased individuals who experienced trauma, poisoning, asphyxia, or sudden death due to vascular disorders without spinal damage recorded and were subdivided into 11 age groups (Table. 1).
Table 1: Number of Specimens of the Lumbar Spine Through Different Age Groups
| Age group number | Year-old | Males (n) | Females (n) |
| 1 | 0 | 11 | 12 |
| 2 | 0-1 | 7 | 5 |
| 3 | 1-3 | 5 | 4 |
| 4 | 3-7 | 3 | 4 |
| 5 | 8-12 | 4 | 3 |
| 6 | 13-16 | 5 | 3 |
| 7 | 17-20 | 7 | 6 |
| 8 | 21-35 | 18 | 15 |
| 9 | 36-60 | 21 | 17 |
| 10 | 61-74 | 14 | 22 |
| 11 | 75-90 | 11 | 15 |
| Total | 106 | 105 |
Direct measurements of anterior-posterior and transverse diameter of vertebral foramina were taken from each vertebra utilizing a digital caliper. The distance between the vertebral body's posterior border and the vertebral lamina's inner surface at the midline was defined as the anterior-posterior diameter of the spinal canal. The transverse diameter of the spinal canal was measured as the distance between the vertebral pedicles. Repeatability of measurements: to assess measurement errors for intra-reliability tests, four specimens were randomly selected, and all parameters from their 20 lumbar vertebrae (L1-L5) were measured on two consecutive days by the same observer under similar experimental conditions. For inter-reliability tests, two investigators undertook three sets of measurements from 20 third lumbar vertebrae. Descriptive statistics were calculated for all measurements. The rate of spinal canal growth was calculated as a % difference from a previous age group for both dimensions. TIBCO Statistica® software's analysis of variance (ANOVA) was used to determine the relationship between the dimensions of the spinal canal and age. The data between the male and female groups were compared using an independent samples t-test. A p-value of less than 0.05 was employed as the criterion for statistical significance.
Results
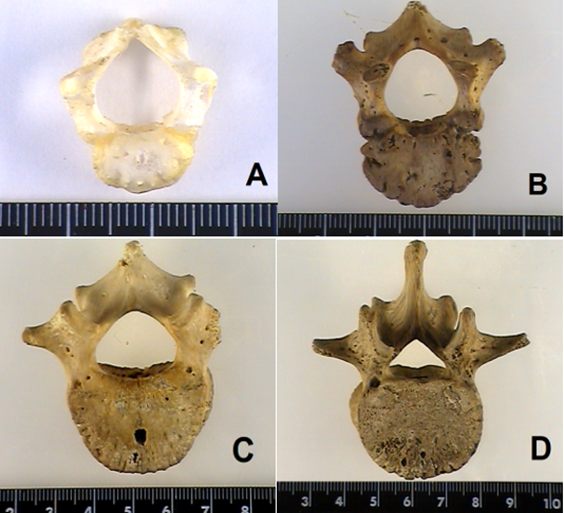
The shape of the lumbar vertebral foramina was different across the age groups: from the drop shape of a vertebral foramen in new-borns (Figure. 1A) to an oval shape in children with a broad longitudinal diameter (Figure. 1B), it becomes a triangle in teenagers (Figure. 1D). The shape of the lumbar vertebral foramen has a significant anatomical variation among adults.
Figure 1: Photos of the third lumbar vertebra (superior view) from the different age groups: A - 1st age group, B - 3rd group, C - 4th group, and D - 6th group. The scale at the bottom is calibrated in cm and mm.
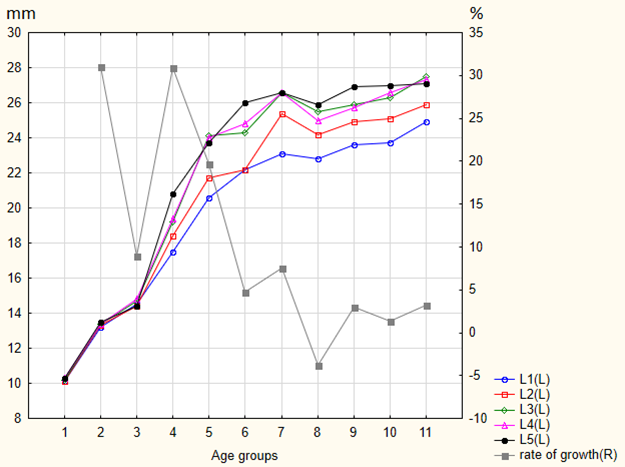
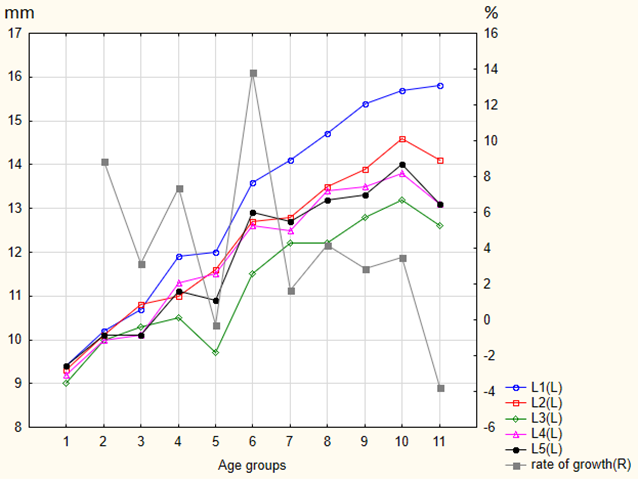
Direct measurements of anterior-posterior and transverse diameter of vertebral foramina were taken from 1055 vertebrae. There was good interobserver and interobserver reliability for all measurements. For interobserver reliability, the intraclass correlation coefficients ranged from 0.95-0.97, while for interobserver reliability, they ranged from 0.82 to 0.88. Validity was also very high (r=0.91; P lessthen 0.001). Tables 2 and 3 summarize data for transverse and anterior-posterior diameters of the lumbar spinal canal on L1-L5 levels for persons of different age groups. In new-borns, on average, the lumbar spinal canal (L1-L5) transverse and anterior-posterior diameters were 10.1 mm - 10.3 mm and 9.0 mm - 9.4 mm. In the first year of life, the transverse diameter increases by an average of 31.0% among the different lumbar vertebrae and the sagittal diameter - by 8.9%. During the first seven years of life (age groups 3 and 4), the dimensions of the vertebral foramina expand rapidly (31%) with the growth of the vertebrae. By this age, the average sizes of the transverse diameter are 17.5 mm - 20.8 mm, increasing from L1 to L5 (Figure. 2). Anterior-posterior diameter in the same age groups increases by 7.36% and is smallest one on the L3 level -10.5±1.6 mm, increasing up 11.9±1.1 mm at L1 level and down 11.1±1.4 mm at L5 (Figure. 3). Interestingly enough, that is the only age when data analysis shows statistically significant gender difference at L2 level: 12.4±1.0 mm in males and 9.9±0.4 mm females (Table. 3).
Figure 2: Transverse spinal canal diameter (mm) for different age groups and growth rate (%).
Figure 3: Anterior-posterior spinal canal diameter (mm) for different age groups and growth rate (%).
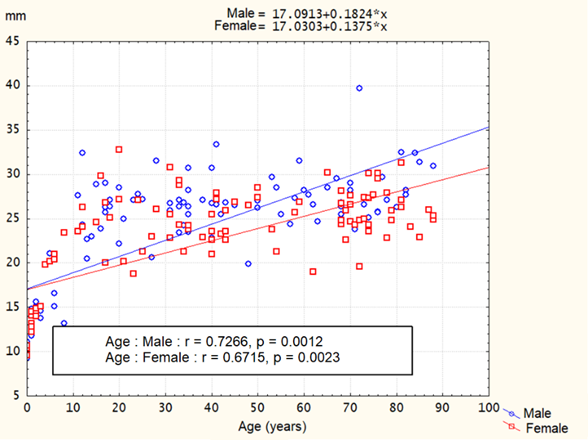
The second significant increase in the size of the spinal canal due to the rapid growth of the vertebral column was found in teenagers (age groups 5-6). The spinal canal's transverse diameter was 22.2mm-26.0mm, increasing from L1 to L5, with a growth rate of 4.78%-19.7%. Anterior-posterior diameter in the same age groups increased by 13.9% and was 11.5mm-13.6mm. In the following age groups, the increase in the size of the vertebral foramina was insignificant. The average sizes of the transverse diameter were 23.7mm-27.0mm, and for anterior-posterior diameter, they were 12.6mm-15.8mm. Further analysis indicated a strong correlation between the sizes of the spinal canal and age: r=0.67, r=0.72, (p less then 0.05) for males and r=0.48, r=0.67, (p less then 0.05) for females. The linear regression formulas for L3 transverse diameter were:
TRD for males = 17.0913 + 0.1824*X
TRD for females = 17.0303 + 0.1375*X,
where TRD is the transverse diameter of the L3 vertebral foramen in mm, and X is the age in years (Fig. 4).
Table 2: Transverse Diameter of Spinal Canal (Mm) for Different Age Groups
| Age group (number) years | Sex | L1 Mean ± SD | L2 Mean ± SD | L3 Mean ± SD | L4 Mean ± SD | L5 Mean ± SD |
| (1) 0 | M | 10.3±0.4 | 10.2±0.6 | 10.2±0.6 | 10.4±0.3 | 10.3±0.7 |
| F | 9.9±0.8 | 10.0±0.4 | 10.1±0.4 | 10.2±0.3 | 10.3±0.2 | |
| M+F | 10.1±0.7 | 10.1±0.5 | 10.2±0.5 | 10.3±0.3 | 10.3±0.7 | |
| (2) 0-1 | M | 13.2±1.2 | 13.2±0.5 | 13.4±1.1 | 13.5±0.9 | 13.3±0.8 |
| F | 13.2±0.9 | 13.4±0.9 | 13.4±0.9 | 13.4±1.1 | 13.7±1.4 | |
| M+F | 13.2±1.0 | 13.3±0.7 | 13.4±1.0 | 13.4±0.9 | 13.5±5.2 | |
| (3) 1-3 | M | 14.5±0.4 | 14.6±0.6 | 14.7±0.7 | 14.9±0.6 | 14.5±0.8 |
| F | 14.7±0.5 | 14.2±0.4 | 14.7±0.5 | 14.6±0.4 | 14.3±0.6 | |
| M+F | 14.5±0.5 | 14.4±0.6 | 14.7±0.6 | 14.8±0.5 | 14.4±0.7 | |
| (4) 3-7. | M | 17.6±3.3 | 16.5±3.1 | 17.6±3.1 | 17.8±2.7 | 18.6±2.8 |
| F | 17.4±0.8 | 19.9±0.6 | 20.4±0.5 | 20.5±2.4 | 22.4±0.4 | |
| M+F | 17.5±2.0 | 18.4±2.6 | 19.2±2.4 | 19.4±2.7 | 20.8±2.6 | |
| (5) 8-12 | M | 20.0±5.3 | 21.5±6.0 | 24.4±8.2 | 24.0±6.7 | 23.7±6.5 |
| F | 21.6±0.6 | 22.2±1.3 | 23.5±0.1 | 24.1±0.5 | 23.5±1.3 | |
| M+F | 20.6±4.2 | 21.7±4.7 | 24.1±6.3 | 24.0±5.2 | 23.7±5.1 | |
| (6) 13-16 | M | 22.3±1.6 | 21.9±3.4 | 23.8±3.1 | 24.1±2.8 | 26.1±4.6 |
| F | 22.2±1.7 | 22.8±3.6 | 25.0±1.2 | 25.9±1.8 | 25.9±2.5 | |
| M+F | 22.2±1.5 | 22.2±3.2 | 24.3±2.5 | 24.8±2.5 | 26.0±3.7 | |
| (7) 17-20 | M | 22.6±1.9 | 25.1±1.3 | 26.3±2.1 | 26.0±0.8 | 26.9±2.1 |
| F | 23.7±2.4 | 25.8±3.5 | 27.0±4.3 | 27.3±2.8 | 26.3±2.1 | |
| M+F | 23.1±2.1 | 25.4±2.4 | 26.6±3.1 | 26.6±2.0 | 26.6±2.0 | |
| (8) 21-35 | M | 23.7±2.8 | 24.5±2.1 | 26.4±2.5 | 25.7±2.5 | 26.7±2.5 |
| F | 21.7±3.2 | 23.8±3.1 | 24.5±3.5 | 24.2±3.4 | 25±4.6 | |
| M+F | 22.8±3.1 | 24.2±2.6 | 25.5±3.1 | 25.0±3.0 | 25.9±3.7 | |
| (9) 36-60 | M | 24.8±2.9 | 26.0±3.0 | 26.9±3.1 | 26.8±3.0 | 28.0±3.5 |
| F | 22.1±2.7 | 23.5±3.1 | 24.7±2.4 | 24.3±2.7 | 25.4±2.4 | |
| M+F | 23.6±3.1 | 24.9±3.3 | 25.9±3.0 | 25.7±3.1 | 26.9±3.3 | |
| (10) 60-74 | M | 25.2±3.8 | 26.5±3.9 | 27.7±3.8 | 27.7±3.8 | 27.7±4.6 |
| F | 22.8±2.6 | 24.1±2.7 | 25.4±2.8 | 25.8±3.2 | 26.5±2.6 | |
| M+F | 23.7±3.3 | 25.1±3.4 | 26.3±3.4 | 26.6±3.5 | 27.0±3.5 | |
| (11) 75-90 | M | 25.3±2.2 | 26.8±1.9 | 28.9±2.6 | 28.5±3.2 | 28.9±3.3 |
| F | 24.6±3.0 | 25.2±2.9 | 26.4±2.5 | 26.5±2.5 | 25.7±2.0 | |
| M+F | 24.9±2.7 | 25.9±2.6 | 27.5±2.8 | 27.3±2.9 | 27.1±3.0 |
Table 3: Anterior-Posterior Diameter of Spinal Canal (Mm) For Different Age Groups
| Age group (number) years | Sex | L1 Mean ± SD | L2 Mean ± SD | L3 Mean ± SD | L4 Mean ± SD | L5 Mean ± SD |
| (1) 0 | M | 9.6±0.5 | 9.4±0.3 | 9.2±0.3 | 9.3±0.4 | 9.4±0.4 |
| F | 9.2±0.4 | 9.1±0.2 | 8.9±0.3 | 9.0±0.2 | 9.4±0.8 | |
| M+F | 9.4±0.4 | 9.3±0.3 | 9.0±0.4 | 9.2±0.3 | 9.4±0.6 | |
| (2) 0-1 | M | 10.2±0.4 | 10.1±0.3 | 9.9±0.2 | 9.9±0.4 | 10.1±0.7 |
| F | 10.2±0.3 | 10.1±0.2 | 10.2±0.7 | 10.1±0.6 | 10.2±0.7 | |
| M+F | 10.2±0.4 | 10.1±0.3 | 10.0±0.5 | 10.0±0.5 | 10.1±0.7 | |
| (3) 1-3 | M | 10.9±0.4 | 10.6±0.9 | 10.2±0.7 | 10.0±0.5 | 9.9±0.7 |
| F | 10.5±0.7 | 11.0±0.6 | 10.5±0.1 | 10.2±1.1 | 10.2±0.3 | |
| M+F | 10.7±0.5 | 10.8±0.7 | 10.3±0.5 | 10.1±0.8 | 10.1±0.6 | |
| (4) 3-7. | M | 12.8±0.7 | 12.4±1.0* | 11.8±1.8 | 12.1±1.6 | 12.4±1.2 |
| F | 11.2±0.6 | 9.9±0.4 | 9.5±0.3 | 10.6±0.6 | 10.2±0.4 | |
| M+F | 11.9±1.1 | 11.0±1.5 | 10.5±1.6 | 11.3±1.3 | 11.1±1.4 | |
| (5) 8-12 | M | 12.3±3.0 | 12.5±4.2 | 9.7±1.6 | 11.9±3.1 | 11.1±1.3 |
| F | 11.3±0.6 | 9.7±1.8 | 9.7±0.8 | 10.7±0.8 | 10.6±0.5 | |
| M+F | 12.0±2.4 | 11.6±3.7 | 9.7±1.3 | 11.5±2.5 | 10.9±1.1 | |
| (6) 13-16 | M | 13.3±0.6 | 12.4±1.0 | 11.1±1.1 | 12.3±0.5 | 11.9±0.7 |
| F | 14.1±0.9 | 13.3±2.0 | 12.2±1.2 | 13.1±1.5 | 14.5±3.2 | |
| M+F | 13.6±0.8 | 12.7±1.4 | 11.5±1.2 | 12.6±1.0 | 12.9±2.2 | |
| (7) 17-20 | M | 14.1±1.8 | 12.8±1.1 | 11.8±1.1 | 12.4±0.9 | 12.8±1.0 |
| F | 14.1±2.1 | 12.7±1.4 | 12.9±2.2 | 12.5±1.0 | 12.5±1.5 | |
| M+F | 14.1±1.9 | 12.8±1.1 | 12.2±1.7 | 12.5±0.9 | 12.7±1.2 | |
| (8) 21-35 | M | 14.7±1.4 | 13.4±1.1 | 11.6±1.0 | 12.7±1.3 | 13.4±1.3 |
| F | 14.6±1.8 | 13.5±1.4 | 12.8±1.6 | 14.1±5.9 | 13.0±1.0 | |
| M+F | 14.7±1.6 | 13.5±1.2 | 12.2±1.4 | 13.4±4.1 | 13.2±1.1 | |
| (9) 36-60 | M | 15.1±2.6 | 13.7±1.8 | 12.2±1.1 | 13.1±1.2 | 13.1±1.3 |
| F | 15.8±1.9 | 14.1±1.2 | 13.5±1.4 | 14.1±1.3 | 13.6±1.2 | |
| M+F | 15.4±2.3 | 13.9±1.6 | 12.8±1.4 | 13.5±1.3 | 13.3±1.3 | |
| (10) 60-74 | M | 15.6±1.3 | 14.8±1.8 | 13.8±2.0 | 14.2±1.1 | 14.3±1.2 |
| F | 15.8±1.9 | 14.4±2.1 | 12.8±1.3 | 13.6±1.4 | 13.8±2.0 | |
| M+F | 15.7±1.7 | 14.6±2.0 | 13.2±1.6 | 13.8±1.3 | 14.0±1.7 | |
| (11) 75-90 | M | 16.4±1.2 | 14.2±1.7 | 13.1±2.4 | 13.8±2.2 | 13.6±2.2 |
| F | 15.4±1.9 | 14.0±2.1 | 12.2±1.1 | 12.6±1.5 | 12.7±0.9 | |
| M+F | 15.8±1.7 | 14.1±1.9 | 12.6±1.8 | 13.1±1.9 | 13.1±1.6 |
*- statistically significant difference
Discussion
Many studies illustrate the importance of understanding lumbar spinal canals' distinct measurements and morphology across various populations. This data underpins clinical research, informs surgical interventions, and aids the development of appropriately designed implants to cater to varying physiological norms [27]. Our study suggests that lumbar vertebral foramen significantly varied in shape depending on the age group: in newborns, it has a drop shape; in children with a broad longitudinal diameter, it takes the form of an oval; and in teenagers, it takes the shape of a triangle. Also, there is a significant anatomical diversity in the form of the lumbar vertebral foramen in adults.
It supports the previous study regarding the dimensions of the lumbar spinal canal in the Egyptian population, identifying the importance of precise dimensions of the lumbar vertebrae for surgical interventions and designing implants. Three hundred CT scans were gathered to quantify the typical values of the midsagittal diameter, interpedicular distance, and lateral recess depth at different levels of the lumbar spine. This study found variability along the lumbar spine's length, noting a transition from circular or rounded shapes in the upper lumbar vertebrae, trefoil shapes primarily in the lower lumbar vertebrae (mostly at L5), and triangular shapes in the mid-lumbar vertebrae. The L3 level was the narrowest; very few patients showed a statistically stenotic midsagittal diameter measurement [28]. Two studies suggested spinal canal development concludes by age seventeen [19, 20]. Their research found noticeable variability in spinal canal size during development and contributed towards a reference range for lumbar spinal canal dimensions across sexes and different age groups. Our data support these findings and indicate that the transverse diameter of the spinal canal the most significantly increases in the first year of the postnatal life by 31% and the anterior-posterior diameter by 13.9% in the teenager group (by the age of 16). After this age, we did not find significant changes in the spinal canal sizes.
The demographic heterogeneity in spinal dimensions is supported by two comparative investigations conducted on CT scan images of patients from Indian and Pakistani populations. Males typically exhibited larger anterior-posterior spinal canal dimensions, according to research conducted on patients in India (13.29±1.1 mm - 16.19±1.26 mm) and patients in Pakistan (14.77mm-17.7mm) [23, 24]. We recorded smaller sizes of the spinal canal anterior-posterior diameter for the same age group in the Ukrainian population: 12.8±1.6 mm - 14.6±1.8 mm. Notably, our data support a consistent pattern where the spinal canal anterior-posterior diameter was smallest at L3, subsequently enlarging cranially and caudally, as described in the previous study in the Chinese population [20].
The morphometric study was conducted within Bosnia and Herzegovina and focused on measuring and analyzing the anterior-posterior and transverse diameters of the lumbar spinal canaldrawing from a cohort of adults(20-60 years old) patients who underwent CT scans due to lumbar pain. The data showed the largest sample average anterior-posterior diameter at the L1 level (19.06 mm) and the smallest at the L3 level (16.66 mm). An interesting observation was the hourglass shape of the anterior-posterior diameter, showing narrowing at the L3 level across genders. The transverse diameter was largest at the L5 level with an average of 31.94 mm and smallest at the L1 level with an average of 24.78 mm in this group. Gender differences were evident, with the anterior-posterior diameter significantly larger in females and the transverse diameter larger in males from L1 to L5. A comparative analysis revealed that the Bosnian and Herzegovinian populations had significant variations in these measurements compared to other global populations. In Bosnia and Herzegovina, this offers helpful reference information for the treatment of patients with lumbar canal stenosis and lower back pain [29]. In contrast, we did not find statistically significant gender differences in spinal canal dimensions for the Ukrainian population, except anterior-posterior diameter for children 3-7 years old. However, our data supports that transverse diameter increases in a caudal direction from L1 -23.6±3.1 mm until L5 - 26.9±3.3 mm.
The other research comparatively evaluates the lumbar anatomy of Māori people, the indigenous population of New Zealand (NZ), against NZ Europeans, examining vertebral body heights, lengths, segmental angles, pedicle height, width, and vertebral canal dimensions. Differing from the other global studies, which rarely factored in ethnic variations, it focused on assessing the canal-to-body ratio, vertebral canal length, and width across patient demographics of age, sex, and ethnicity. This research underlined fundamental differences between Māori and NZ Europeans [30]. The principle findings for NZ Europeans were increasing spinal canal width down (22.6±2.0 mm -28.2±3.1 mm) up to a maximum at L5 and the smallest anterior-posterior diameter on the level L3 -14.8±1.9 mm increasing up L1 - 16.6±1.8 mm and L5 -15.1±1.8 mm down. These findings are well associated with our results for the Ukrainian population in the same age group: L1-L5 transverse diameter was 23.7±3.3 mm - 27.0±3.5 mm, and the smallest anterior-posterior diameter on the level L3 - 13.2±1.6 mm increasing up L1 - 15.7±1.7 mm and down L5 - 14.0±1.7 mm.
Conclusion
In conclusion, this study contributes to the comprehension of the features unique to the human spinal canal by providing a comprehensive database of spinal canal dimensions in the Ukrainian population in relation to age and gender, comparing this information with the architecture of the spinal canal in different ethnic groups, which is important in improving methods for identifying and managing disorders specific to the lumbar area that differ among various racial and ethnic groups.
Conflict of interest
The authors declare no conflicts of interest, financial or otherwise.
References
- Raja A, Hoang S, Patel P, Mesfin FB. (2023). Spinal Stenosis. 2023 Jun 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Publisher | Google Scholor - Boissière L, Moal B, Gille O, De-Roquefeuil E, et al. (2017 ). Lumbar spinal muscles and spinal canal study by MRI three-dimensional reconstruction in adult lumbar spinal stenosis. Orthop Traumatol Surg Res.103(2):279-283.
Publisher | Google Scholor - Kitab S, Lee BS, Benzel EC. (2018). Redefining lumbar spinal stenosis as a developmental syndrome: an MRI-based multivariate analysis of findings in 709 patients throughout the 16- to 82-year age spectrum. J Neurosurg Spine. 1;29(6):654-660.
Publisher | Google Scholor - Kitab S, Habboub G, Abdulkareem SB, Alimidhatti MB, Benzel E. (2019). Redefining lumbar spinal stenosis as a developmental syndrome: does age matter? J Neurosurg Spine. 17;31(3):357-365.
Publisher | Google Scholor - Abbas J, Yousef M, Peled N, Hershkovitz I, Hamoud K. (2023). Predictive factors for degenerative lumbar spinal stenosis: a model obtained from a machine learning algorithm technique. BMC Musculoskelet Disord. 23;24(1):218.
Publisher | Google Scholor - Shrestha I. (2022). Mean Canal-body Ratio among Specimens of Dried Lumbar Vertebrae in the Department of Anatomy of a Medical College: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 60(248):389-392.
Publisher | Google Scholor - Lee JH, Kang KC, Kim KT, Kim YC, Chang TS. (2021). Extent and characteristic of relationships in canal dimension and canal body ratio between cervical and lumbar spine. Sci Rep. 16;11(1):18471.
Publisher | Google Scholor - Jaganjac B, Džidić-Krivić A, Bečulić H, Šljivo A, et al. (2023). Magnetic resonance morphometry of the lumbar spinal canal in Zenica - Doboj Canton in Bosnia and Herzegovina. Med Glas (Zenica). 1;20(2).
Publisher | Google Scholor - Mahato NK. (2023). Load-Bearing Shifts in Laminar and Ligament Morphology: Comparing Spinal Canal Dimensions Using Supine versus Upright Lumbar MRI in Adults without Back Pain. Indian J Radiol Imaging. 6;33(3):344-350.
Publisher | Google Scholor - Lee DH, Lee DG, Hwang JS, Jang JW, et al. (2021). Clinical and radiological results of indirect decompression after anterior lumbar interbody fusion in central spinal canal stenosis. J Neurosurg Spine. 15;34(4):564-572.
Publisher | Google Scholor - Lee CW, Yoon KJ, Kim SW. (2019). Percutaneous Endoscopic Decompression in Lumbar Canal and Lateral Recess Stenosis - The Surgical Learning Curve. Neurospine. 16(1):63-71.
Publisher | Google Scholor - Linkoaho O, Kivisaari R, Ahonen M. (2017). Spinal canal dimensions affect outcome of adolescent disc herniation. J Child Orthop. 11(5):380-386.
Publisher | Google Scholor - Gatam AR, Gatam L, Phedy, Mahadhipta H, et al. (2022). Full Endoscopic Lumbar Stenosis Decompression: A Future Gold Standard in Managing Degenerative Lumbar Canal Stenosis. Int J Spine Surg. 16(5):821-830.
Publisher | Google Scholor - Pennington Z, Alentado VJ, Lubelski D, Alvin MD, et al. (2019). Quality of life changes after lumbar decompression in patients with tandem spinal stenosis. Clin Neurol Neurosurg. 184:105455.
Publisher | Google Scholor - Hartman J, Granville M, Jacobson RE. (2019). Radiologic Evaluation Of Lumbar Spinal Stenosis: The Integration Of Sagittal And Axial Views In Decision Making For Minimally Invasive Surgical Procedures. Cureus. 11(3):e4268.
Publisher | Google Scholor - Tobin MK, Gragnaniello C, Horwitz J, Sun FW, Schizas C, Neckrysh S. (2021). Generational Changes in Lumbar Spinal Canal Dimensions: Findings from a Sample U.S. Population. World Neurosurg. 146:e902-e916.
Publisher | Google Scholor - Long MT, Del Re AM, Uya A, Kanegaye JT, Nguyen MB. (2022). Seated Position Does Not Change Lumbar Dimensions Compared with Lateral Position. Pediatr Emerg Care. 1;38(1):e23-e26.
Publisher | Google Scholor - Papp T, Porter RW, Aspden RM. (1994). The growth of the lumbar vertebral canal. Spine (Phila Pa 1976). 19(24):2770-3.
Publisher | Google Scholor - Watts R. (2013). Lumbar vertebral canal size in adults and children: observations from a skeletal sample from London, England. Homo. 64(2):120-8.
Publisher | Google Scholor - Griffith JF, Huang J, Law SW, Xiao F, et al. (2016). Population reference range for developmental lumbar spinal canal size. Quant Imaging Med Surg. 6(6):671-679.
Publisher | Google Scholor - Peters JR, Servaes SE, Cahill PJ, Balasubramanian S. (2021). Morphology and growth of the pediatric lumbar vertebrae. Spine J. 21(4):682-697.
Publisher | Google Scholor - Mavrych V, Bolgova O, Ganguly P, Kashchenko S (2014). Age-Related Changes of Lumbar Vertebral Body Morphometry. Austin J Anat. 1(3): 1014.
Publisher | Google Scholor - Yadav U, Singh V, Bhargava N, Kumar Srivastav A, et al. (2020). Lumbar Canal Diameter Evaluation by CT Morphometry-Study of Indian Population. Int J Spine Surg. 30;14(2):175-181.
Publisher | Google Scholor - Alam MM, Waqas M, Shallwani H, Javed G. (2014). Lumbar morphometry: a study of lumbar vertebrae from a pakistani population using computed tomography scans. Asian Spine J. 8(4):421-6.
Publisher | Google Scholor - Monier A, Omoumi P, Schizas S, Becce F, Schizas C. (2017). Dimensional changes of cervical and lumbar bony spinal canals in one generation in Western Switzerland: a computed tomography study. Eur Spine J. 26(2):345-352.
Publisher | Google Scholor - Maeder B, Becce F, Kehtari S, Monier A, et al. (2023). Evolution of the Cross-Sectional Area of the Osseous Lumbar Spinal Canal across Decades: A CT Study with Reference Ranges in a Swiss Population. Diagnostics (Basel). 15;13(4):734.
Publisher | Google Scholor - Chazono M, Tanaka T, Kumagae Y, Sai T, Marumo K. (2012). Ethnic differences in pedicle and bony spinal canal dimensions calculated from computed tomography of the cervical spine: a review of the English-language literature. Eur Spine J. 21(8):1451-8.
Publisher | Google Scholor - Aly T, Amin O. (2013). Geometrical dimensions and morphological study of the lumbar spinal canal in the normal Egyptian population. Orthopedics. 36(2):e229-34.
Publisher | Google Scholor - Cizmic M, Hadziosmanovic E, Baljic R, Ahmetspahic A, Merhemic Z. (2023). Morphometric Study of Lumbar Spinal Canal Dimensions in Bosnia and Herzegovina Population. Acta Inform Med. 31(3):200-205.
Publisher | Google Scholor - Cook WH, Baker JF. (2021). Comparative Analysis of Lumbar Spine Vertebral Morphology Between Māori and New Zealand Europeans: A Computed Tomography Study. Int J Spine Surg. 15(6):1072-1081.
Publisher | Google Scholor