Case Report
Acute Abdomen in Second Trimester Due to Ruptured Bicornuate Uterus
Post graduate institute of Medicine, University of Colombo, Sri Lanka.
*Corresponding Author: Sanjaya Walawe Nayaka,Post graduate institute of Medicine, University of Colombo, Sri Lanka.
Citation: Walawe Nayaka S. (2023). Acute Abdomen in Second Trimester Due to Ruptured Bicornuate Uterus, Journal of Women Health Care and Gynecology, BioRes Scientia publishers. 2(2):1-3. DOI: 10.59657/2993-0871.brs.23.012
Copyright: © 2023 Sanjaya Walawe Nayaka, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 10, 2023 | Accepted: August 24, 2023 | Published: August 26, 2023
Abstract
Acute abdomen in pregnancy is a challenging condition to the physicians due to difficulty in diagnosing and management. Bicornuate uterus (BU) is rare congenital anomalies which can gives arise to various obstetrics complications including uterine rupture even in unscarred uterus, present as acute abdomen. This is a case of acute abdomen in second trimester due to ruptured BU.
Keywords: bicornuate uterus; mullerian; uterine rupture; primi gravida
Introduction
Acute abdomen refers to sudden onset severe abdominal pain which may associate with nausea and vomiting that demands urgent medical or surgical interventions [1]. Obstetrics and gynecological causes present as acute abdomen are placental abruption, ruptured ectopic pregnancy, uterine rupture, cysts accidents and red degeneration of fibroids. Other causes include acute appendicitis, cholecystitis, pancreatitis, and diverticulitis [1]. Proper history, examination, appropriate investigation and immediate relevant therapeutic measures reduce the morbidity and mortality.
Out of the obstetrics causes for acute abdomen, uterine rupture is a relatively rare catastrophic condition with high morbidity and mortality which usually seen in scarred uterus (previous caesarean section or myomectomy) or multi gravida (during labour). Thus, it is extremely rare among primi gravida (1 in 7643 to 1 in 16,849 deliveries) without any past myomectomies [2-4]. Rupture of the uterus is a rare life-threatening event in first two trimesters and it is mostly due to the congenital uterine anomalies. 0.1% to 3% of all women and 10% of women with 3 or more consecutive pregnancy losses have congenital uterine anomalies [5,6]. BU origins due to the failure of fusion of Mullerian ducts during embryogenesis and accounts for 25% of all mullerian duct developmental abnormalities [7]. Other than recurrent pregnancy losses and subfertility; women with BU may present with obstetrics complications such as mid-trimester miscarriages, preterm labor and delivery, malpresentation, and antepartum and postpartum hemorrhage while 60% of women with BU will have a live birth [8]. BU may be the only risk factor for rupture of an unscarred uterus even though it is rare [3]. This is a case of an acute abdomen during second trimester due to ruptured BU.
Case history
26-year-old previously healthy lady who was in her 23rd week of her first pregnancy which was found to be uncomplicated so far, presented with sudden onset diffuse severe abdominal pain for the last 30 minutes. She didn’t have any per vaginal bleeding. She had two previous ultra sound scans at 12th week and 20th week which found to be normal for the gestational age without any ovarian cysts or uterine fibroids. She denied any past history of pelvic imaging or abdominal surgeries.
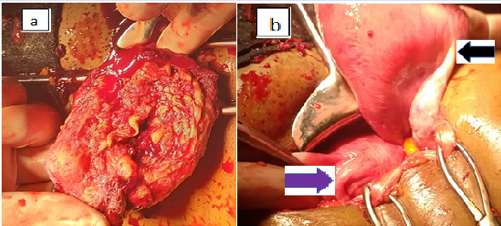
On examination she was pale, drowsy and tachypnoeic. Her pulse rate was 130beats per minutes and blood pressure was 70/40mmHg. Her abdomen was slightly distended and extremely tender. Uterus can’t be palpated properly as she was in severe pain. There was no bleeding through the cervical os and she had cervical motion tenderness. Immediate resuscitation was started and blood was sent for full blood count, grouping and cross matching. Trans-abdominal scan of the abdomen demonstrated the fetus with absent fetal cardiac activity and free fluid in the hepato-renal pouch. Her hemoglobin level was 4g/dl. Following these clinical and radiological findings, tentative diagnosis of uterine rupture was made and immediate laparotomy was done. Massive hemoperitoneum was noted (approximately 1500ml) due to ruptured right cornu of a BU. Right tube had been completely separated from the uterus. Gestational sac with the fetus was in the peritoneal cavity.
Figure 1: Intra operative view of the uterus (a) ruptured site at right tubal insertion (b) postero-superior view of the uterus (left side horn-purple arrow and right-side horn- black arrow).
Ruptured right horn was excised and uterine reconstruction was done. Three units of blood were transfused and post-operative ICU care given for 24 hours. Her recovery was uneventful and she was discharged after counselling.
Discussion
BU is considered as a major risk factor for uterine rupture in mid trimester even in an unscarred uterus due to presence of fibrous band between two corpora which limits the uterine wall distention [8]. BU may associate with longitudinal vaginal septum (in 25% of cases) and renal anomalies [9]. BU can be sub divided into two depending on the involvement of cervical canal.
- Bicornuate unicollis- uterus with one cervical canal and central myometrium extends up to internal os.
- Bicornuate bicollis- uterus with two cervical canals and central myometrium extends up to the external os.
Most of the women with BU are asymptomatic and usually diagnosed when they are being investigated for pregnancy complications [recurrent pregnancy loss (25%), preterm birth (15–25%) and cervical insufficiency (38%)] or during abdominal surgeries (caesarean section, laparoscopy or hysterectomy) [10]. Otherwise, this can be diagnosed by imaging with ultra sound scan (USS), hysterosalpingogram (HSG) or magnetic resonance image (MRI) [9]. Concave or heart shape external appearance, widely diverged uterine horns, widened intercornual distance (>4cm) and more than one-centimeter-deep central cleft are the characteristic features of BU. Usually the communication of two horns is taken place at the level of uterine isthmus. The angle between two horns is usually more than 105 degrees [11]. Differential diagnoses are uterine didelphys and septate uterus [9]. BU should be distinguished from septate uterus as septate uterus can be treated with hysteroscopic resection. Most reliable method of diagnosing BU would be combined hysteroscopy and laparoscopy.
As ruptured BU usually present as an acute abdomen during mid trimester, high index of suspicion is needed for diagnosis as clinicians don’t think about obstetric causes like this in a primi gravida with unscarred uterus. Treatment of choice is immediate stabilization of the patient followed by emergency laparotomy and resection of the ruptured horn. Patient should be advised regarding the importance of using reliable contraception for at least one year and risk of happening the same thing to the remaining horn during next pregnancy. As BU associates with renal anomalies, it would be a good practice to arrange USS to exclude it.
Conclusion
Even though BU is a rare anomaly, it can be presented in mid trimester with catastrophic intra-peritoneal hemorrhage which need high index of suspicion to diagnose and prevent the delay in surgical management to minimize the maternal morbidity and mortality. Proper counselling plays a major role in preventing adverse out comes during subsequent pregnancies.
Declarations
Conflict of interest
No conflict of interest.
Funding
No funding
Consent
Informed written consent obtained from the patient.
References
- John W. Patterson, Sarang Kashyap, Elvita Dominique. Acute Abdomen.
Publisher | Google Scholor - D.A. Miller, T.M. Goodwin, R.B. Gherman, R.H. Paul. (1997). Intrapartum rupture of the unscarred uterus, Obstet Gynecol, 89:671-673.
Publisher | Google Scholor - V. Catanzarite, L. Cousins, D. Dowling, S. (2006). Daneshmand, Oxytocin-associated rupture of an unscarred uterus in a primigravida. Obstet Gynecol, 108:723-725.
Publisher | Google Scholor - Singh N, Singh U, Verma ML. (2013). Ruptured bicornuate uterus mimicking ectopic pregnancy: A case report. J Obstet Gynaecol Res, 39(1):364-366.
Publisher | Google Scholor - Acien P. (1997). Incidence of Müllerian defects in fertile and infertile women. Hum Reprod, 12:1372-1376.
Publisher | Google Scholor - Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, Pellicer A. (1997). Reproductive impact of congenital Müllerian anomalies. Hum Reprod, 12:2277-2281.
Publisher | Google Scholor - Nahum GG. (1998). Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med, 43:877-887.
Publisher | Google Scholor - B. Nitzsche, M. Dwiggins, S Catt. (2017). Uterine rupture in a primigravid patient with an unscarred bicornuate uterus at term, Case Rep. Womens Health, 15:1-2.
Publisher | Google Scholor - Gaillard F, Weerakkody Y, Niknejad M, et al. (2023). Bicornuate uterus. Reference article, Radiopaedia.org.
Publisher | Google Scholor - S. Jayaprakash, L. Muralidhar, G. Sampathkumar, R. Sexsena. (2011). Rupture of bicornuate uterus, BMJ Case Rep.
Publisher | Google Scholor - Ly JQ. (2002). Rare bicornuate uterus with fibroid tumors: hysterosalpingography-MR imaging correlation. AJR Am J Roentgenol, 179(2):537-538.
Publisher | Google Scholor