Case Report
Acinetobacter Baumannii Necrotizing Fasciitis Associated with Chincken Skin Wrapped Around the Knee Area?
1Department of Emergency Medicine, Sisli Hamidiye Etfal Training & Research Hospital, University of Health Sciences, Turkey.
2Department of Aesthetic Plastic and Reconstructive Surgery, Sisli Hamidiye Etfal Training and Research Hospital, University of Health Sciences, Turkey.
3Department of Emergency Medicine, Bağcılar Training and Research Hospital, University of Health Sciences, Turkey.
*Corresponding Author: Abuzer Coskun, Department of Emergency Medicine Bağcılar Training and Research Hospital, University of Health Sciences Turkey, Istanbul, Turkey.
Citation: Mehmet N. Sutasir, Oztürk S, Altınbilek E, Coskun A. (2024). Acinetobacter Baumannii Necrotizing Fasciitis Associated with Chincken Skin Wrapped Around the Knee Area? Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(3):1-6. DOI: 10.59657/2837-4681.brs.24.065
Copyright: © 2024 Abuzer Coskun, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 28, 2023 | Accepted: January 22, 2024 | Published: January 29, 2024
Abstract
Necrotizing fasciitis is an uncommon and potentially fatal infection that can affect the epidermis, dermis, and more commonly the subcutaneous, fascia, and muscle layers. Necrotizing fasciitis is usually caused by toxin-producing bacteria with a relatively fast progression associated with severe surrounding tissue destruction. Early diagnosis and management are crucial factors for survival. Microbiological examination confirmed the diagnosis of necrotizing fasciitis caused by Acinetobacter baumanii. A broad-spectrum antibiotic therapy was administered and later readjusted according to the results of microbiological culture. Broad-spectrum antibiotics along with surgical debridement, sometimes multiple, are needed in order to stop or slow down the progression of Necrotizing fasciitis. Despite optimal care, necrotizing fasciitis remains a highly morbid condition with a high mortality rate. In this case we present a 71 years old patient who injured right knee three days ago and chicken skin was wrapped around the trauma site with rapidly developing fatal Acinetobacter baumaniiassociated with necrotizing fasciitis.
Keywords: necrotizing fasciitis; acinetobacter baumanii; chicken skin
Introduction
Necrotizing fasciitis [NS] is a life-threatening and rapidly progressive skin infection that occurs mostly in the extremities. NS could affect the perineum, the genital area, and most commonly the lower extremities. It is a rapidly progressing condition, making timely clinical diagnosis challenging and taking immediate measures the most important factors for survival and treatment. Some predisposing conditions are diabetes mellitus, alcoholism, hypertension, and malignancies. In addition to these conditions, obesity, chronic kidney dysfunction, and lymphocytic dysfunction leading to immunosuppression are all predisposing factors to NS [1-3]. Necrotizing fasciitis is often misdiagnosed as cellulitis or other similar skin and soft tissue infections such as erysipelas. It is a polymicrobial infection in approximately 70% of cases. The most common pathogens associated with necrotizing fasciitis include group A Beta-hemolytic Streptococcus, Group-B Streptococcus, Enterococci, Coagulasenegative Staphylococci, Staphylococcus Aureus, Escherichia Coli, Pseudomonas Aeruginosa, Bacteroides, and Clostridium [4]. Acinetobacter Baumannii is rarely associated with NFS, fasciitis, especially in immunocompetent hosts [5].
Acinetobacter baumannii is the Gram-negative opportunistic human pathogen. Acinetobacter baumannii, an aerobic, Gram-negative bacillus, is ubiquitously isolated from soil, water [1]. This Gram-negative pathogen is recognized by the Centers for Disease Control and Prevention and the World Health Organization as an urgent threat to public health and a critical priority for which the development of new antibiotics is crucially needed, respectively [2]. A significant proportion of patients have other comorbidities such as diabetes, cancer, chronic renal failure and rheumatoid arthritis and are often immunocompromised [1]. Study in which A. baumannii was the sole microbial cause of human necrotizing fasciitis Reported in 2009 [6]. Necrotizing fasciitis caused byAcinetobacter baumannii is particularly rare but reports of these infections have increased over the last decade. Many patients presented with classical symptoms like erythema, swelling and tachycardia, had abnormal blood results and had a clear minimal trauma or a /surgical wound as the portal of entry [7]. Once necrotizing fasciitis is diagnosed, immediate debridement and intravenous antibiotic therapy are required to limit the spread of infection [8]. This study reports a case report Acinetobacter baumannii in necrotizing fasciitis for a tertiary hospital.
Case Presentation
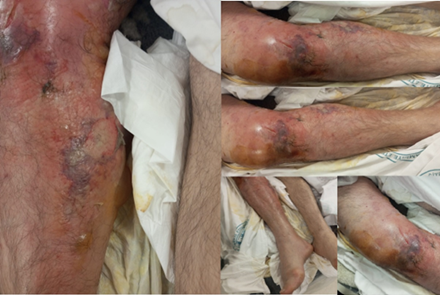
A 71-year-old male patient was admitted to the Emergency Department with an injured right knee caused by a cleaver three days ago. According to the patient, chicken skin was wrapped around the trauma site for healing purposes. The patient’s complaint was worsening and liquid accumulation on the wound, which was kept closed for one day. In the emergency room physical examination (Figure 1) diffuse erythema starting from the right thigh and extending to the crus and a diffuse bullous area with irregular borders were observed. There was a clear diameter difference in the contralateral leg.
Figure 1: Anteromedial view of the right knee of the patient admitted to the emergency room after the wound was wrapped with chicken skin.
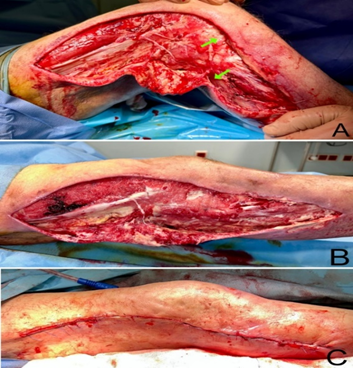
There was tenderness and increased temperature on palpation, and no crepitus was observed. Distal pulses were palpable. There was diffuse hypoesthesia in the right lower extremity. Right lower extremity motor movements were limited secondary to pain. The patient was operated on by a plastic surgeon under spinal anesthesia on the second day of admission to the emergency room, according to his general condition. In the operation, fasciotomy was performed in all compartments of the lower extremity through medial and lateral longutidunal incisions (Figure2A-3A). Aggressive debridement of necrotic tissues was performed until viable tissues were reached. A deep tissue biopsy and culture were then obtained (Figure2A). No neurovascular structure or bone exposure was observed in the defect. An extensive washout with hydrogen peroxide and, afterwards, a Vacuum-Assisted Closure [VAC] dressing was applied to the defect.
Figure 2: Fasciotomy was performed in the operation room. A. Debridement of necrotic tissues through a lateral longitudinal incision is shown. Green arrows indicate the sites of deep tissue culture. B. Healing of the lateral defect is seen on day 16 of admission. C. The lateral defect was primary closed on day 19 of admission.
Microbiological examination confirmed the diagnosis of necrotizing fasciitis caused by Acinetobacter baumanii. A broad-spectrum antibiotic therapy was administered and later readjusted according to the results of microbiological culture. Cultures from the right leg confirmed the growth of Acinetobacter baumannii, resistant to amikacin, imipenem, ciprofloxacin, piperacillin/tazobactam, co-trimoxazole, and sensitive to colistin and tigecycline. After consultation with an infectious diseases’ physician, the antibiotic regimen was changed to intravenous polymyxin and meropenem. The patient had a large defect in the right lower extremity, and his hemodynamics deteriorated due to fluid and protein loss in the inpatient unit follow-up. The patient's hemoglobin level was 6.6g/dl, while the albumin level was 2.2g/dl. Therefore, two units of erythrocyte suspension were transfused, and albumin treatment was administered. In the inpatient unit follow-up, bedside debridement was performed every third day of VAC treatment. As the patient's general condition improved, the wound was re-examined in the operating room on the 11th and 16th days of admission. The wound was clean, but there were still areas of necrosis along the wound edges (Figure 2B-3B). Although there was necrotic tissue attached to the fascia, the musculature was living. As the edema of the lower extremity decreased, approximating sutures were placed on the lateral and medial skin flaps. A new VAC dressing was applied.
Figure 3: Necrotic tissue attached to the fascia. A. Debridement of necrotic tissues through a medial longitudinal incision is shown. Signs of necrotizing fasciitis are shown clearly. B. Healing of the medial defect is seen on day 16 of admission.
19 days after the admission, it was noted in the operation room that there was significant improvement. Therefore, the defect on the lateral side was closed primerally (Figure 2C). Approximating sutures were applied to the medial defect, and the VAC dressing was applied again.
Discussion
Necrotizing fasciitis is characterized by a rapidly progressing necrosis of both the fascia and subcutaneous tissue. The fulminant tissue necrosis may rapidly progress into septic shock with multiorgan failure [9]. Once symptomatic, the progression of disease is typically measured in hours; early diagnosis and treatment are crucial to survival. It is a surgical emergency with an associated mortality as high as 75%. When NFS is established or highly suspected, urgent exploration and debridement of tissue is the cornerstone of obtaining a diagnosis and successful management. During surgery, the findings of grayish necrotic fascia, decrease in resistance to blunt dissection, absence of bleeding of the fascia, and presence of foul-smelling purulent discharge are diagnostic [10].
The treatment of patients with NS is challenging and consists of adequate surgical debridement, supportive care by the intensivist and starting broad spectrum antimicrobials. The choice of antibiotics depends on the suspected causative microorganisms, part of the body that is affected and clinical picture. Antibiotic therapy can be narrowed down as culture results are known. The most important factor is early surgical aggressive debridement, which is associated with a lower mortality when performed within 24 hours [11]. In our case we were also treated wıth aggressıve debrıdement. Acinetobacter Baumannii was detected in the culture and antibiotic treatment was continued. Acinetobacter Baumannii is Gram-negative Bacillus which is known to cause ventilator-associated pneumonia, blood infections, wound infections, and catheter-related infections. This pathogen produces AmpC Cephalosporinases and Aminoglycoside modifying enzymes with an ability to upregulate its efflux pumps and downregulate its outer membrane porins. Moreover, this organism has been known to have a heightened ability to acquire resistance from the environment. Up to 30% of Acinetobacter Aaumanii isolates from intensive care units have been shown to be multidrug resistant and have been associated with increased mortality rates [9,10,12]. Literature shows that other rare reports of necrotizing Acinetobacter Baumannii involving both "peau d'orange" cellulitis developing vesicles [also progressing to sepsis and death] and bacteremia concurrent with bullae; these findings provide further evidence that this is a unique infectious syndrome with recognizable features. our patient who had bullae with bacteremia, demonstrating the usefulness of blood cultures to identify the organisms causing bullous cellulitis when wound cultures are not available [13,14]. Clinical observations suggest that the spectrum of disease caused by Acinetobacter baumannii includes severe and necrotizing skin and soft tissue infection and thatAcinetobacter baumannii is an important consideration in the contemporary differential diagnosis of severe and necrotizing skin and soft tissue infection. The surgical management of our case was aggressive with a total of 3 procedures during his hospital admission with histology and repeated microbiology obtained to guide antimicrobial therapy. A review of patients with complicated skin and soft tissue infections confirmed susceptibility in patients with co-morbidities, prior surgical intervention, more severe infections such as bacteraemia affected fascia and in patients admitted to intensive care unit [15].
The early diagnosis of necrotizing soft tissue infection is challenging, but the key to successful management of patients with necrotizing soft tissue infection are early recognition and complete surgical debridement. Early initiation of appropriate broad-spectrum antibiotic therapy must take into consideration the potential pathogens. Critical care management such as the initial fluid resuscitation, end-organ support, pain management, nutrition support, and wound care are all important aspects of the care of patients with necrotizing soft tissue infection. Soft tissue reconstruction should take into account both functional and cosmetic outcome. Importantly in patients with necrotizing soft tissue infection, a delay of surgical treatment of >12 hour is associated with an increased number of surgical debridements and higher incidence of septic shock and acute renal failure. Because aggressive radical debridement of all poorly perfused tissue is required, patients frequently suffer from massive skin defects, which often requires autograft skin grafting or myocutaneous flaps [16]. Our patient's situation was different in that he had a history of trauma three days ago and had been infected by wrapping chicken skin instead of trauma. Acinetobacter baumannii is emerging as an important cause of severe, lifethreatening cellulitis and other skin and soft tissue infections and may be associated with a high mortality despite early aggressive and appropriate treatment.
Conclusion
Necrotizing fasciitis remains an important disease in our community with significant morbidity and mortality. Early diagnosis of NS can be difficult and requires a high index of suspicion in all patients presenting with cellulitis or unexplained sepsis. NS which is caused by Acinetobacter baumannii is a rare life-threatening condition that requires prompt recognition and aggressive surgical debridement along with broad-spectrum antibiotics.
Declarations
Author Contributions
Conception/Design of study- M.N.C, S.O; Data acquisition- E.A, A.C.; Data analysis/Interpretation- M.N.C, E.A; Drafting manuscript- E.A, A.C.; Critical revision of manuscript- A.C.; Final approval and accountability- S.O; Technical or material support – M.N.C, S.O; Supervision – M.N.C, S.O, E.A, A.C.
Informed Consent
Written informed consent was obtained from the patient. Ethics Committee Approval: Ethics committee approval was not required for the case report.
Conflict of Interest
Authors declared no conflict of interest
Financial Disclosure
Authors declared no financial support.
Funding
None declared.
Availability of Data and Materials
All data is available on request without restriction.
Conflict of Interest
None declared.
Human Rights
The study was made in following the Declaration of Helsinki for Human Research.
References
- Sun X, Xie T. Management of Necrotizing Fasciitis and Its Surgical Aspects. Int J Low Extrem Wounds. 2015;14(4):328-34.
Publisher | Google Scholor - Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, Pulcini C, Kahlmeter G, Kluytmans J, Carmeli Y, Ouellette M, Outterson K, Patel J, Cavaleri M, Cox EM, Houchens CR, Grayson ML, Hansen P, Singh N, Theuretzbacher U, Magrini N; WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318-327.
Publisher | Google Scholor - Neilly DW, Smith M, Woo A, Bateman V, Stevenson I. Necrotising fasciitis in the North East of Scotland: a 10-year retrospective review. Ann R Coll Surg Engl. 2019;101(5):363-372.
Publisher | Google Scholor - Sinha N, Niazi M, Lvovsky D. A fatal case of multidrug resistant acinetobacter necrotizing fasciitis: the changing scary face of nosocomial infection. Case Rep Infect Dis. 2014;2014:705279.
Publisher | Google Scholor - Corradino B, Toia F, di Lorenzo S, Cordova A, Moschella F. A difficult case of necrotizing fasciitis caused by Acinetobacter baumannii. Int J Low Extrem Wounds. 2010;9(4):152-154.
Publisher | Google Scholor - Charnot-Katsikas A, Dorafshar AH, Aycock JK, David MZ, Weber SG, Frank KM. Two cases of necrotizing fasciitis due to Acinetobacter baumannii. J Clin Microbiol. 2009;47(1):258-263.
Publisher | Google Scholor - Nisbet M, Ansell G, Lang S, Taylor S, Dzendrowskyj P, Holland D. Necrotizing fasciitis: review of 82 cases in South Auckland. Intern Med J. 2011;41(7):543-548.
Publisher | Google Scholor - Swain RA, Hatcher JC, Azadian BS, Soni N, De Souza B. A five-year review of necrotising fasciitis in a tertiary referral unit. Ann R Coll Surg Engl. 2013;95(1):57-60.
Publisher | Google Scholor - Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21(3):538-582.
Publisher | Google Scholor - Kempf M, Rolain JM. Emergence of resistance to carbapenems in Acinetobacter baumannii in Europe: clinical impact and therapeutic options. Int J Antimicrob Agents. 2012;39(2):105-14.
Publisher | Google Scholor - Bucca K, Spencer R, Orford N, Cattigan C, Athan E, McDonald A. Early diagnosis and treatment of necrotizing fasciitis can improve survival: an observational intensive care unit cohort study. ANZ J Surg. 2013;83(5):365-370.
Publisher | Google Scholor - McConnell MJ, Actis L, Pachón J. Acinetobacter baumannii: human infections, factors contributing to pathogenesis and animal models. FEMS Microbiol Rev. 2013;37(2):130-155.
Publisher | Google Scholor - Villalba F, Mañana P, Limongi G. Celulitis necrotizante por Acinetobacter baumannii [Necrotizing cellulitis caused by Acinetobacter baumannii]. Enferm Infecc Microbiol Clin. 2000;18(9):479-480.
Publisher | Google Scholor - Chiang WC, Su CP, Hsu CY, Chen SY, Chen YC, Chang SC, Hsueh PR. Community-acquired bacteremic cellulitis caused by Acinetobacter baumannii. J Formos Med Assoc. 2003;102(9):650-652.
Publisher | Google Scholor - Garau J, Ostermann H, Medina J, Avila M, McBride K, Blasi F; REACH study group. Current management of patients hospitalized with complicated skin and soft tissue infections across Europe (2010-2011): assessment of clinical practice patterns and real-life effectiveness of antibiotics from the REACH study. Clin Microbiol Infect. 2013;19(9):E377-85.
Publisher | Google Scholor - Kobayashi L, Konstantinidis A, Shackelford S, Chan LS, Talving P, Inaba K, Demetriades D. Necrotizing soft tissue infections: delayed surgical treatment is associated with increased number of surgical debridements and morbidity. J Trauma. 2011;71(5):1400-1405.
Publisher | Google Scholor