Research Article
Acceptability of Bilateral Tubal Ligation Among Women Attending Antenatal Clinic in University College Hospital (UCH), Ibadan
1Department of Obstetrics and Gynaecology, University College Hospital, Ibadan, Oyo State, Nigeria.
2University of Ibadan, Ibadan, Oyo State, Nigeria.
*Corresponding Author: Stephen SALUFU, Department of Obstetrics and Gynaecology, University College Hospital, Ibadan, Oyo State, Nigeria.
Citation: Stephen Salufu. (2025). Acceptability of Bilateral Tubal Ligation Among Women Attending Antenatal Clinic in University College Hospital (UCH), Ibadan. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 5(3):1-7. DOI: 10.59657/2993-0871.brs.25.086
Copyright: © 2025 Stephen Salufu, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 28, 2025 | Accepted: April 22, 2025 | Published: March 04, 2025
Abstract
Background: Female sterilization or bilateral tubal ligation (BTL) is the most popular method of contraception worldwide and globally; an estimated 220 million couples rely on tubal ligation for contraception. Though female sterilization is one of the safest contraceptive methods with complications <1%, the acceptability of this method of family planning is still very low in Nigeria with uptake rate of 1.00%–3.15%. There are different factors militating against acceptability of BTL in different parts of Nigeria, and these factors include poor awareness, lack of access, cultural factors, religious factors, lack of partner or family members approval, and so on. This study, therefore, was to identify uptake and the factors affecting the acceptability of BTL among patients receiving antenatal care in UCH, Ibadan and proffers solution to the age long problem of the country.
Objectives: The study assessed the level of knowledge of modern contraceptives among the women attending antenatal clinic in UCH, Ibadan, and their readiness to uptake bilateral tubal ligation after completion of family size.
Methods: The study was a descriptive cross-sectional study involving consenting registered antenatal patients at UCH, Ibadan. Result of study: Majority of the respondents (75.0%) were not aware of bilateral tubal ligation, and only 17.3% of the participants were willing to consider this method of contraceptive after completing their family size with future regret being the major reason they will not consider this method of contraceptive. The study also demonstrated that there was significant relationship between source of information and level of acceptability of BTL. Other reasons for regret include women of low or nulliparity, partner’s disapproval, religious and cultural beliefs were other reasons giving in this study for the rejection of BTL by the participants
Conclusion: This study demonstrates there is poor uptake of bilateral contraceptive which may be as a result of poor knowledge of this method of contraception.
Keywords: sterilization; contraception; relationship; family planning
Introduction
Bilateral tubal ligation (BTL), a form of female sterilization, results in mechanical blocking or interruption of the fallopian tubes to prevent sperm from fertilizing the egg [1–4]. The procedure was first used in the early 19th century by James Blundell, and the first published report of this procedure was in 1881 [5,6]. By mid-20th century, it has begun to gain popularity [6]. It is one of the best and effective method of contraception for women who have completed their family size or for whom there is medical indication [2,6]. There are different methods of tubal ligation and they include Pomeroy, Modified Pomeroy, Parkland, Uchida, Madlener, Kroener and Irving [7]. Modified Pomeroy’s method is the common technique used for tubal ligation in Nigeria. This is because it is easier to perform, and it is one of the techniques with the lowest failure rate [8,9]. The fallopian tube can be approached through laparotomy, minilaparotomy, culdotomy, culdoscopy and laparoscopy using different anaesthetic techniques [7,9].
The procedure can be carried out either on an outpatient or inpatient basis at any time in the menstrual cycle in the non-pregnant women or during the post-partum (usually within 48hours after delivery), interval (done six weeks or more after delivery) or following spontaneous or induced abortion [1,3,7,9,10] . It can be done during caesarean section (C/S) or as a sub-umbilical mini-laparotomy before uterine involution following vaginal delivery [3,7,11]. Hysteroscopic tubal ligation is generally performed during the early follicular phase of the menstrual cycle [7]. Most bilateral tubal ligations in Nigeria are usually carried out during caesarean section [2,9,12]. The most common indication for tubal ligation in Nigeria is repeat caesarean sections with completion of family size [8,9]. Failure after surgical ligation is rare and crude failure rate ranges from 0.2%-1.3% with highest failure rate in tubal ligation done at caesarean section or immediate post-partum [1,7].
It has been shown by various studies that despite good knowledge of modern contraceptives, most people have reservations and are unwilling to accept bilateral tubal ligation [1,10]. Different studies have shown the poor uptake of modern contraceptives in Nigeria especially the uptake of Bilateral Tubal Ligation (BTL). This study therefore, was to identify the level of uptake and the factors determining the acceptability of BTL among those receiving antenatal care in University College Hospital, Ibadan and proffers solution to the age long problem of the country.
The findings from study can also be used by the family planning unit of the hospital and the government at large to formulate policies that will improve the uptake of modern contraceptives in University College Hospital (UCH) and in Nigeria at large.
Objectives
The study assessed the level of knowledge of modern contraceptives among the women attending antenatal clinic in University College Hospital, Ibadan, and their readiness to uptake bilateral tubal ligation after completion of family size.
Method
Study design: The study was a cross-sectional, descriptive study involving consenting registered antenatal patients seeking care at UCH, Ibadan.
Study area: This study was carried out at the antenatal clinic at the university College Hospital, Ibadan. At the moment, antenatal clinics are conducted on three days at the University College Hospital. The number of clients at each clinic session averages 100-150. The routine activities at the sessions include group health education, performance of vital signs by the nurses, and laboratory investigations (urinalysis and packed cell volume). The University College Hospital, Ibadan is a tertiary hospital that serves as a referral centre for private and primary care facilities as well as secondary health care facilities. The hospital was initially commissioned in the year 1957 with a capacity of 500 beds; presently it has 1000 beds and 163 examination coaches. The maternity section has 130 beds.
Study population: All pregnant women assessing antenatal care at the University College Hospital, Ibadan.
Sampling technique: Convenience sampling.
Sample size determination
The sample size was estimated Cochran Formula:
N = Zα2PQ
where N = the minimum sample size; Zα = the standard normal deviate corresponding to a side level of
significance of 0.05; P = the proportion of respondent who will consider BTL as appropriate from Port-Harcourt study = 0.183 (Enyindal 2018); Q = 1-p; d = the desired level of precision = 0.05
N= 1.962 x 0.183 (1 – 0.183) / 0.052 = 230
This gave a minimum sample of size of 230 participants. Assuming a non-response rate of 20%, a sample size of 276 women was gotten.
Ethical consideration: Ethical approval was obtained from the Institution Review Board (IRB) of the University of Ibadan/University College Hospital, Ibadan with IRB number UI/EC/23/0461.
Data analysis: Self and Interviewer administered questionnaires were used to obtain data from the women. The questionnaires were pretested and validated. The data obtained was imputed on the data page of the statistical package for social sciences version 24, and the data was cleaned as appropriate. Analysis of data was by computer using the Statistical Package for Social Sciences (SPSS; SPSS- 24 for Windows Evaluation Version). Level of statistical significance was set at 95% confidence level.
Results
273 out of the 276 were properly filled by the respondents giving a response rate of 98.91% questionnaires for this study. The mean age of the participated in this study was 31.41±4.73. Majority (53.1%) of the respondents were within the age range of 31-40 years. 18% were civil servants while 16.5% were Artisan. 243 of the respondents had tertiary level of education. Almost all (97.8%) the respondents were married. Seventy-five percent of the respondents practice Christianity while (24.4%) practice Islamic religion. Eighty-one percent were from the Yoruba’s ethnicity group. More than half (54.2%) have had 1 or 2 parous experiences.
Table 1: Sociodemographic characteristics of the respondents
| Variables | Frequency | Percent |
| Ages (in years) | ||
| ≤ 20 | 5 | 1.8 |
| 21-30 | 114 | 41.8 |
| 31-40 | 145 | 53.1 |
| ≥ 41 | 9 | 3.3 |
| Occupation | ||
| Civil servant | 49 | 18.4 |
| Professional | 90 | 33.7 |
| Artisan | 44 | 16.5 |
| Students | 12 | 4.5 |
| Trader | 35 | 13.1 |
| Business woman | 29 | 10.9 |
| Self employed | 2 | 0.7 |
| Housewife | 4 | 1.5 |
| Unemployed | 2 | 0.7 |
| Highest Level of Education | ||
| Secondary | 23 | 8.6 |
| Tertiary | 243 | 91.4 |
| Marital status | ||
| Single | 7 | 2.2 |
| Married | 272 | 97.8 |
| Religion | ||
| Christianity | 205 | 75.6 |
| Islam | 68 | 24.4 |
| Ethnicity | ||
| Yoruba | 221 | 81.0 |
| Igbo | 26 | 9.5 |
| Others | 26 | 9.5 |
| Parity | ||
| 0 | 109 | 40.0 |
| 1-2 | 148 | 54.2 |
| >2 | 16 | 5.8 |
Table 2: Knowledge of modern contraception
| Variables | Frequency | Percent |
| Knowledge of contraception | ||
| Yes | 224 | 82.4 |
| No | 49 | 17.6 |
| Source of information about contraception | ||
| Hospital staff | 98 | 35.9 |
| Friends/Relatives | 60 | 22.0 |
| Radio/social media | 54 | 19.8 |
| All | 10 | 3.7 |
| Others | 18 | 6.6 |
| Not heard | 33 | 12.1 |
82 percentage of the participants have heard of contraception and this information was mainly from hospital staff, but 12 percentage of the respondents have never heard about any of the contraceptive methods.
Table 3: Knowledge of bilateral tubal ligation
| Variables | Yes | No | ||
| n | % | n | % | |
| Ever heard of bilateral tubal ligation (BTL)? | 68 | 25.0 | 205 | 75.0 |
| Do you know anyone who has done BTL? | 22 | 8.1 | 250 | 91.9 |
| Bilateral tubal ligation is the tying of both fallopian tubes | 75 | 27.8 | 195 | 62.2 |
| Bilateral tubal ligation is reversible | 34 | 12.6 | 236 | 86.4 |
| Bilateral tubal ligation is for those who have completed their family size | 71 | 26.2 | 190 | 73.8 |
| Bilateral tubal ligation is safe | 60 | 22.1 | 211 | 77.9 |
Only 25% of the participants are aware of bilateral tubal ligation, 8.1 percentage of the participants know someone who has done BTL in the past, and 77.9% of the respondents believed that BTL is safe.
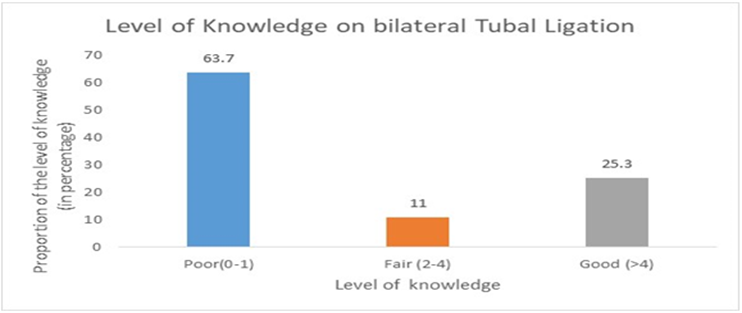
Figure 1 above shows that 63.7 percentage of the respondents had poor knowledge while twenty-five percent had good knowledge on bilateral tubal ligation.
Table 4: Acceptability of bilateral tubal ligation
| Variables | Yes | No | Indifferent | |||
| n | % | n | % | n | % | |
| Willingness to do BTL after completion of family size | 47 | 17.2 | 158 | 57.9 | 68 | 24.9 |
| Reasons for not wanting BTL in the future Partner’s disapproval | 126 | 46.3 | 69 | 25.0 | 8 | 28.7 |
| Religious belief against BTL | 51 | 18.8 | 111 | 40.1 | 109 | 40.2 |
| Cultural belief against BTL | 30 | 11.0 | 119 | 43.9 | 122 | 45.0 |
| BTL causes regret in the future | 75 | 49.9 | 98 | 36.6 | 98 | 36.2 |
| Will you become an advocate for BTL? | 56 | 21.0 | 121 | 44.5 | 94 | 34.2 |
The acceptability of BTL among the participants was poor with only 17.2 percentage of them showing their willingness to do BTL after the completion of their family size. Future regret was the major reason they will not consider it.
Table 5: Association between contraceptive use and knowledge of BTL
| Variables | Level of knowledge of BTL | Total | χ2 | p-value | ||
| Poor | Fair | Good | ||||
| Ever heard of contraceptives | ||||||
| Yes | 142(63.4) | 26(11.6) | 56(25.0) | 224 | 0.461 | 0.794 |
| No | 31(64.6) | 4(8.3) | 13(27.1) | 48 | ||
| Source of information | ||||||
| Hospital staff | 63(64.3) | 12(12.2) | 23(23.5) | 98 | 23.930 | 0.002* |
| Friends/Relatives | 41(68.3) | 8(13.3) | 11(18.3) | 60 | ||
| Radio/social media | 37(68.5) | 3(5.6) | 14(25.9) | 54 | ||
| All | 5(27.8) | 1(5.6) | 12(66.7) | 18 | ||
| Others | 6(60.0) | 3(30.0) | 1(10.0) | 10 | ||
| Ever used any type of contraceptive | ||||||
| Yes | 81(68.1) | 11(9.2) | 27(22.7) | 119 | 1.873 | 0.392 |
| No | 92(60.1) | 19(12.4) | 42(27.5) | 153 | ||
| Husband approval of contraceptive | ||||||
| Yes | 73(68.2) | 10(9.3) | 24(22.4) | 107 | 1.948 | 0.378 |
| No | 12(54.5) | 2(9.1) | 8(36.4) | 22 | ||
Parenthesis = %; *-significant at p-value less than 0.05
Twenty-five percent who had ever heard of contraceptives, had good knowledge of BTL compare to (27.1%) who have never heard of contraceptives but had good knowledge. Although this difference is not statistically significant (p-value >0.05), the table shows further that (25.9%) who had about contraceptive via radio/social media had good knowledge of BTL compare to (68.5%) who had poor knowledge. Therefore, there was significant relationship between source of information and level of acceptability of BTL.
Table 6: Readiness to undertake bilateral tubal ligation.
| Variables | Yes (%) | No (%) |
| Age of Respondent | ||
| less than 20 years | 0.4 | 1.5 |
| 20 – 30 years | 6.6 | 35.2 |
| 31 – 40 years | 9.2 | 44 |
| ≥ 41 years | 1.1 | 2.2 |
| Level of Education | ||
| Secondary | 1.9 | 6.8 |
| Tertiary | 15.4 | 75.9 |
| Parity | ||
| None | 5.9 | 38.6 |
| 1 – 2 | 9.9 | 40.4 |
| 3 - 4 | 1.1 | 3.7 |
| > 4 | 0.4 | 0 |
| Tribe | ||
| Yoruba | 15.3 | 69.3 |
| Igbo | 1.1 | 8.8 |
| Others | 0.8 | 4.6 |
| Religious | ||
| Christianity | 12.5 | 63.1 |
| Islam | 4.8 | 19.6 |
The table shows that across every variable, the respondents that rejected BTL were more than those who were willing to accept it.
Discussion
There were two hundred and seventy-three women participants in this study with a mean age of 31.41±4.73 years. Almost all of the participants (97.8%) were married with 54.2% of them having 1 or 2 parous experiences, and 91.4% had tertiary level of education. 33% of them were professionals; 18% were civil servants while 16.5% were Artisans. Christians were the majority (75%). Most of the participants were from the Yoruba ethnic group. Even with good knowledge of modern contraceptives (82.4%), only 25.0% have heard of BTL with just 8.1% of having knowledge of someone who has used bilateral tubal ligation in the past. This observation of good contraceptive knowledge was collaborated by the studies of Ugoji et al and Egede et al in which 65.5% and 83.3% respectively where aware of various modern contraceptive methods [1,13,14]; while the poor knowledge of BTL agrees with the study done by Enyindah et al in which 52.5% of respondents have never heard of bilateral tubal ligation [15]. The study also demonstrated that there was significant relationship between source of information and level of acceptability of BTL. The knowledge of contraceptives in this study was mainly gotten from hospital staff (35.9%), friends/relatives (22.0%) and radio/social media (19.8%), but it is disheartening to note that 17.6% of the respondents have never heard about contraceptives despite the availability of the various sources of information about it. 42.6% of those who have never used any modern contraceptive methods in this study are also not willing to use them in the future [16].
This study demonstrates that only 17.3% of the participants will consider bilateral tubal ligation after the completion of their family size, which was similar to what was obtained in the studies by Kahansim ML et al in which only 17.7% of patients accepted BTL, and that by Enyindah et al where 18.3% are willing to undergo BTL after the completion of their family size [13,17]. Different studies have demonstrated this poor uptake of BTL in various parts of Nigeria and Africa. For instance, the study in Makurdi shows that only 78 women representing 2.7% of all acceptors of family planning had bilateral tubal ligation, 2.1% in the study by Ugo et al, and also low uptake in the study by Tesfaw et al at Ethiopia[1,4,8]. There was a rise in the acceptability of BTL at the University of Jos Teaching Hospital, when the Access to Voluntary Safe Contraception (AVSC) assisted the hospital to train counsellors and doctors in female sterilization by minilaparotomy under local anesthesia, thereby making the procedure readily available and affordable with peak of 36.1% of BTL in 1992 [18]. After 1992, there has been a steady decline in the uptake of BTL due to delaying childbearing until later in life, increased availability and variety of long acting equally effective reversible contraceptives particularly the contraceptive implants (Implanon Classic, Implanon NXT, and Jadelle) [18]. Similar decline in the used of BTL has also been observed in different countries such as Norway, Australia, and the United Kingdom where there was reduction by 67%, 60%, and 68.5%, respectively [17,18]. The incidence of tubal ligation in the United States peaked in 1977, but experienced a steady decline in the total annual cases of sterilization (from 687,000 in 1995 to 643,000 in 2006) despite 4% growth in population [17].
Although, some participants in this study age 31 to 40 years, with tertiary level of education, Christians, and Yoruba want bilateral tubal ligation in the future, majority of women in the same categories still refused BTL showing that uptake of BTL age, education and religion. These findings were different to those found by Enyindah CE et al and Makhathini et al where the choice of BTL was influenced by level of education, religion and employment status; or the findings in another study in the United State of America where BTL was more common among women with lower income, lower education, and higher parity [11,15,17]. Unfortunately, the number of children was not a determinant of the acceptability of BTL in this study as most multipara women were not ready to uptake this method of contraception. Future regret was the strongest reason for rejecting this method of contraception in this study. The probability that a woman will regret undergoing sterilization is said to be 14% [6]. Young age (under 30 years of age) has been found to be the strongest risk factor for regret following tubal ligation [6,7]. Other reasons for regret include women of low or nulliparity, partner’s disapproval, religious and cultural beliefs were other reasons giving in this study for the rejection of BTL by the participants. The permanent nature of the method, fear of operation, unexpected child loss, invasive nature of BTL, religious beliefs, and cost consideration were some of the reasons responsible for the poor uptake of BTL in different studies from various parts of Nigeria [2,12,15,16,19].
Failure following sterilization has been reported and this is related to the method of sterilization and age of the woman [6]. The reasons for failure of sterilization include incorrect placement of the mechanical device; development of tuboperitoneal fistula; spontaneous recanalization of the ends of the fallopian tube; and unidentified luteal phase pregnancy [6].
Limitations
The study was limited to women who mostly require the approval of their partners to make necessary contraceptive choices including bilateral tubal ligation. Future studies on BTL should involve both partners.
Conclusion
The level of uptake and knowledge of BTL in this study has been demonstrated to be low, more efforts need to be taken to make the patients to be aware of the benefits of this contraceptive option.
Declarations
Author contributions
All authors involved in the conceptualization, design and planning.
SS and BAA involved in data collection.
SS and OOO involved in the analysis.
All authors involved in the writing of the manuscript.
Consent For Publication
All authors agreed that this manuscript should be published in the International Journal of Obstetrics and Gynaecology.
Declaration of Helsinki
The study was conducted according to the principles of Helsinki Declaration
Availability of Data and Materials
Authors are available and ready to supply the data upon any requests through the corresponding author.
Funding or Financial Support
The authors did not receive any funding or financial support for this study.
Conflict of Interest
No conflict of interest to declare.
Acknowledgements
The authors appreciate the head of department, the consultants and every resident of the department of Obstetrics and Gynaecology, University College Hospital, Ibadan. We acknowledge every pregnant woman that volunteered to participate in this study, you are celebrated.
References
- UGOJI DPC, Fidelis Agwu ONU, ASIEGBU OG, AGWU UM, UGOJI UC, NJOKU CH. Uptake of Bilateral Tubal Ligation as a Contraceptive Option at Alex Ekwueme Federal University Teaching Hospital Abakaliki over a Four-Year Period. Parity. 1(1):3-4.
Publisher | Google Scholor - Thosmas S, Adewole N, Muhammad R, Adebayo F, Offiong R, Agida T. (2021). Trends in female sterilization in north central Nigeria. Int J Res Med Sci, 9.
Publisher | Google Scholor - (2017). Socio-Cultural Factors Influencing Choice of Bilateral Tubal Ligation Among Women Attending University of Ilorin Teaching Hospital. KIU Journal of Social Sciences.
Publisher | Google Scholor - (2024). The Lived Experience of Women Using Bilateral Tubal Ligation Service in Rural Southern Ethiopia: A Phenomenological Study.
Publisher | Google Scholor - (2002). Sterilization C. Global Issues and Trends.
Publisher | Google Scholor - Joshi R, Khadilkar S, Patel M. (2015). Global trends in use of long-acting reversible and permanent methods of contraception: Seeking a balance. Int J Gynecol Obstet, 131(S1):S60-S63.
Publisher | Google Scholor - Micks EA, Jensen JT. (2015). Permanent contraception for women. Women’s Health, 11(6):769-777.
Publisher | Google Scholor - Swende TZ, Hwande TS. (2010). Female sterilization by tubal ligation at caesarean section in Makurdi, Nigeria. Ann Afr Med, 9(4).
Publisher | Google Scholor - Wekere FC, Enyindah CE, Udofia EA. Permanent method of postpartum contraception (Bilateral tubal ligation): Experience at the Rivers State University Teaching Hospital. Age, 25(29):7.
Publisher | Google Scholor - Akpor OA, Fadare RI, Ekanem EI. (2016). Knowledge And Perception of Women Regarding Bilateral Tubal Ligation in Southwest Nigeria. IOSR J Nurs Health Sci IOSR-JNHS, 5(5):1-6.
Publisher | Google Scholor - Makhathini BS, Makinga PN, Green-Thompson RR. (2019). Knowledge, attitudes, and perceptions of antenatal women to postpartum bilateral tubal ligation at Greys Hospital, KwaZulu-Natal, South Africa. Afr Health Sci, 19(3):2615-2622.
Publisher | Google Scholor - Adebimpe WO. (2016). A survey of clients and ethical perspectives of voluntary tubal ligations in the South-Western Nigeria. J Basic Clin Reprod Sci, 5(1):21-26.
Publisher | Google Scholor - Oni GA, McCarthy J. (1986). Use of contraceptives for birth spacing in a Nigerian city. Stud Fam Plann, 17(4):165-171.
Publisher | Google Scholor - (1986). Contraceptive prevalence and preference in a cohort of south-east Nigerian women. PubMed.
Publisher | Google Scholor - Enyindah CE, Hassan KO, Ojule JD, Oranu EO. (2018). Knowledge and Attitude of Fertile Women towards Bilateral Tubal Ligation in Port Harcourt, Southern Nigeria. J Contracept Stud, 3(3):19.
Publisher | Google Scholor - Agida ET, Isah DA, Adebayo FO. (2019). Current Trend in Method Choice among Users of Highly Effective Contraceptives in a Nigerian Tertiary Hospital. J Res Basic Clin Sci, 1(1):29-35.
Publisher | Google Scholor - LM Chan, CL Westhoff. (2010). Tubal sterilization trends in the United States. PubMed.
Publisher | Google Scholor - ML Kahansim, VC Pam, JT Mutihir. (2020). The rise and fall of female sterilization in Jos, Nigeria: A cause for concern. Nigerian Medical Journal.
Publisher | Google Scholor - Ijarotimi AO, Bakare B, Badejoko OO, Akintunde OF, Loto OM, Orji EO. (2015). Contraceptive uptake among women attending family planning clinic in a Nigerian tertiary health facility: a 6 year review. Int J Reprod Contracept Obstet Gynecol, 4(3):721-724.
Publisher | Google Scholor