Case report
A Simple Modified Trephine Technique for Lesser Tarsometatarsal Joints-in Situ Arthrodesis Using a Commercially Available Bone Graft Harvester
1.Foot and Ankle Fellow, Medstar Union Memorial Hospital, Baltimore, Maryland, United States.
2.Foot and Ankle Specialist, Baptist Health Orthopaedic Care, Baptist Health South Florida, Coral Gables, Florida, United States.
*Corresponding Author: Solangel Rodriguez Materon, Foot and Ankle Fellow, Medstar Union Memorial Hospital, Baltimore, Maryland, United States.
Citation: Solangel R Materon. (2023). A Simple Modified Trephine Technique for Lesser Tarsometatarsal Joints - in Situ Arthrodesis Using a Commercially Available Bone Graft Harvester. Journal of Clinical Rheumatology and Arthritis, BioRes Scientia Publishers. 1(1):1-6. DOI: 10.59657/2993-6977.brs.23.005
Copyright: © 2023 Solangel Rodriguez Materon, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 26, 2023 | Accepted: July 13, 2023 | Published: August 24, 2023
Abstract
Arthritis of the lesser tarsometatarsal joints (TMT) is a frequent pathology encountered in the foot and ankle consultation that can lead to disability and chronic pain. It can be present alone or with any other foot deformities. After exhausting conservative treatment, the standard of care is surgery consisting on fusion of the affected joints. Many surgical techniques have been described for the first TMT arthrodesis but there are few with regard to the lesser TMT joints.
We propose as simple technique using one trephine to prepare the joint to be fused and to remove the autograft from the calcaneal bone. Once the graft is harvested, it can be placed in a press-fit fashion at the site of arthrodesis. We use a staple to maintain fixation, taking advantage also of its compression properties.
Keywords: tarsometatarsal arthritis; arthrodesis; midfoot; autograft; lesser tarsometatarsal joints
Introduction
The midfoot tarsometatarsal joint (also known as Lisfranc joint) [1] can be divided into three columns: medial, central and lateral. The medial column corresponds to the first TMT (tarsometatarsal) joint, the central to the second and third TMT joints, and the lateral to the fourth and fifth TMT joints [2]. The arch configuration of the midfoot in the coronal plane is due to the wedge-shaped dorsally based cuneiforms. Metatarsal bases also have a similar shape. The second metatarsal is more proximal positioned versus the other four metatarsals, assuming the position of the keystone. This disposition of bones and the capsule-ligamentous elements surrounding them, give the Lisfranc joint its inherent stability [1, 3].
The metatarsal bases are attached by strong interosseous ligaments, except between the first and second. The Lisfranc ligament, the strongest in this complex, goes obliquely plantarwards from the medial cuneiform to the base of the second metatarsal. The peroneus longus tendon also supports the entire configuration [1]. Arthritis of the TMT joint is a challenging problem to treat. Non-operative treatment can consist of shoe modifications, orthotics, nonsteroidal anti-inflammatories and corticosteroid injections [1, 4, 5]. If this fails, operative treatment is indicated in the appropriate patient. Arthrodesis of the affected joint(s) is considered the definitive surgical treatment of TMT joint arthritis [1]. Arthrodesis is not without its pitfalls as a nonunion rate of up to 11% has been reported.[6] One explanation for this high nonunion rate is shown in a cadaveric study by Johnson et al [7] in which traditional methods of prepping the Lisfranc joints for arthrodesis via curettage, demonstrated a residual layer of calcified cartilage covering the subchondral plate. This was theorized to prevent bony healing at the fusion site.
Multiple techniques have been described for fusion of the TMT joints. These include curettage and fenestration of the joints, with or without bone grafting, using a variety of fixation techniques [1]. Use of autogenous bone grafting, regardless of fixation type, has been found to decrease nonunion rate [6]. Trephine arthrodesis of the TMT joint has gained popularity recently. This technique was first described in the Spine surgery literature [8] and has since been adapted in foot and ankle surgery [9]. Johnson and Johnson [10] first described the use of a trephine arthrodesis technique for lesser metatarsal arthrodesis in which a corresponding dowel graft was taken from the iliac crest and fitted into the previously trephined areas of the Lisfranc joint. Whitney described a similar technique however the dowel graft was obtained from the calcaneus [11].
The technique in this report describes the use of a commercially available bone graft harvester, (In2Bones®, Memphis TN) which is used as a trephine to prepare the TMT joint for fusion as well as obtain cancellous autograft from the ipsilateral calcaneus. Rather than using a cortico- cancellous dowel graft, which may involve taking a large diameter area of lateral wall of the calcaneus or distal tibia, a six- or eight-millimeter cortical window is made with the bone graft harvester.
Technique
An incision is made based on whether a single or multiple TMT joints are being fused. In the example of an isolated second TMT fusion, a 2.5 cm incision can be made directly over the second TMT joint. In the case of a Lapidus procedure with second TMT fusion, the incision can be made slightly longer and more medial. The TMT joint is then curetted down to subchondral bone (figure 1).
Figure 1: An incision can be made directly over the affected TMT joint in the case of isolated TMT arthrosis. In this case, the incision is more medial due to concomitant Lapidus procedure.
The 8mm diameter bone graft harvester is placed centrally over the TMT joint and reamed down to, but not through the plantar cortex of the base of the metatarsal and cuneiform (figure 2).
Figure 2: The bone graft harvester is used as a trephine to prepare the second TMT joint for fusion. The plantar, medial and lateral cortices are not violated to provide stability to construct.
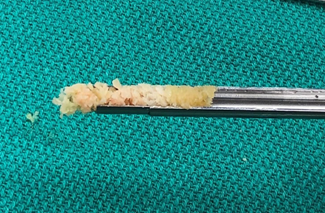
To remove the bone, the outer sleeve of the harvester is disassembled. Viable bone graft can be obtained from the trephine reamings as the bone tends to ‘layer out’ with the sclerotic subchondral bone and cartilage tend to remain in the central portion of the reamings with the metaphyseal bone on either side of the joint to the right and left to it (figure 3).
Figure 3: Reamings from the bone graft harvester can be used to fill the defect. The central portionof the reamings tends to be sclerotic bone and cartilage, which can be separated priorto filling the defect.
This metaphyseal bone can be saved for use later in the case. Attention is then brought to the lateral hindfoot where a 1cm incision is made in the safe zone of the calcaneus. The same bone graft harvester is used and multiple passes at different angles can be made to obtain more bone graft (figure 4).
Figure 4: Bone graft from ipsilateral calcaneus is obtained with the same trephine.
Cancellous bone graft from the calcaneusis then mixed with the bone saved earlier in the case and packed into the fusion site (fig 5). A single Nitinol Compression staple is used to fix the fusion.
Figure 5: The place of the fusion is packed with the bone graft. The desired fixation method is placed we usually use a single Nitinol Compression staple.
Case report
The patient was informed that data concerning the case would be submitted for publication, and she provided consent. Female patient of 52 years-old. Presents with a history of symptomatic bunion, lesser TMT arthritis and bunionette of the right foot. After conservative treatment was exhausted (CAM boot, icing, anti-inflammatories, orthopaedic shoes and activity modification), the patient is taken to surgery (Lapidus procedure, second TMT joint fusion with the technique described, and fifth metatarsal MIS osteotomy). Preoperative x-rays are shown in figure 6. After surgery, the patient was put into an AO type splint.
Figure 6: Preoperative x-rays of the right foot. AP (A), oblique (B), and lateral (C). Hallux valgus, bunionette, and arthritis of the second and third TMT joints.
Postoperative protocol consisted of non-weightbearing (WB) for 6 weeks, progressed weightbearing as tolerated over the following 6 weeks and full weightbearing at 12 weeks. Passive range of movement starts during their early postoperative period. Complete healing of the TMT joint fusions was observed after 12 weeks in radiographs. In last follow-up after a year, the patient was pain free. 1-year post-operative x-rays are shown in figure 7.
Discussion
The fusion technique using autologous bone is a cost-effective technique and has demonstrated less rates of nonunion in foot and ankle surgery [6]. In our technique, we use an autograft taken from cancellous bone from the calcaneus with minimal disruption of the cortex. Taking cancellous bone from the calcaneus and excluding cortical bone from the graft provides less structural damage to the calcaneus and lower donor site morbidity [11]. The use of autograft with only cancellous bone provides better osteoconductive, osteo inductive and osteogenic properties compared to cortical autograft and with any other type of graft and substitute [12].
Claaßen et al describes the surface anatomy of the first, second and third TMT joints in a group of 100 patients (females and males) and reports the average value measured with computed tomography (CT). The distal articular surface width and height of the medial cuneiform are 19.0±5.9 mm and 22.6±6.4 mm respectively. The distal articular surface width and height of the intermedium cuneiform are 13.7±4 mm and 15.9±4.2 mm respectively. The distal articular surface width and height of the lateral cuneiform are 12.9±3 mm and 12.5±2.5 mm respectively [13].
Considering the range of values corresponding to the width of the intermedium and lateral cuneiform, and being able to remove the full depth of the joint, the 8 mm trephine used will prepare for fusion 45% to 82% of the second TMT joint and 50 to 81% of the third TMT joint. Dorsey et al [14] demonstrated that a minimum of 33% bone bridging across the fusion site accurately corresponds with clinical stability during arthrodesis of the ankle and/or arthrodesis of the subtalar joint. Bone bridging depends on many mechanical and biological factors, but the size of surface contact achieved with our technique grants that threshold. The remaining surround of joint provides the structural stability for the fusion, that later will be reinforced by the placement of the implant, in this case a staple.
Between all the options for TMT fusion fixation, staples are a fast and technically simple method that requires less soft tissue dissection and offers a quicker joint preparation. Aiyer et al demonstrated that staples afford better dynamic fixation and sustained compression across the TMT joint when used for arthrodesis as compared to claw plating and crossed screws [15].
Thompson et al described a technique using nitinol staples for lesser TMT fusion in 21 joints.[16] The authors report less soft tissue burden compared to dorsal plate and a stable fixation construct with 100% radiographic fusion after 6 months of surgery [16]. The removal of the cartilage across the joint to be fused is a crucial step in order to promote further healing. Exposure of the cancellous bone is the basis of a successful fusion. Preparation with curettage has previously shown preserved cartilage layers in cadaveric studies, being a potential reason for non-union [11].
Figure 7: 1-year Postoperative x-rays of the right foot. AP (A), oblique (B), and lateral (C). Arthrodesis of the first TMT joint, second TMT joint, and Akin osteotomy fixed. Site of fusion healed. Osteotomy of the fifth metatarsal healed.
Conclusion
We propose a technique that uses the same trephine to harvest the graft, to prepare the fusion site at the TMT joint and to position the autograft. The device is delivered in sterile, single-use kit for rapid harvest. Obtaining morselized cancellous autograft bone also allows to press-fit the graft in the place of fusion over the TMT joint and will enhance the bone healing.
References
- Kurup H, Vasukutty N. (2020). Midfoot arthritis- current concepts review. J Clin Orthop Trauma,11(3):399-405.
Publisher | Google Scholor - Ettinger S, Altemeier A, Stukenborg-Colsman C, Yao D, Plaass C, Lerch M, et al. (2021). Comparison of Isolated Screw to Plate and Screw Fixation for Tarsometatarsal Arthrodesis Including Clinical Outcome Predictors. Foot Ankle Int, 42(6):734-743.
Publisher | Google Scholor - Sripanich Y, Steadman J, Krähenbühl N, Rungprai C, Saltzman CL, Lenz AL, et al. (2021). Anatomy and biomechanics of the Lisfranc ligamentous complex: A systematic literature review. J Biomech, 119:110287.
Publisher | Google Scholor - Drakonaki EE, Kho JS, Sharp RJ, Ostlere SJ. (2011). Efficacy of ultrasound-guided steroid injections for pain management of midfoot joint degenerative disease. Skeletal Radiol, 40(8):1001-1006.
Publisher | Google Scholor - Kalichman L, Hernández-Molina G. (2014). Midfoot and forefoot osteoarthritis. Foot (Edinb), 24(3):128-134.
Publisher | Google Scholor - Buda M, Hagemeijer NC, Kink S, Johnson AH, Guss D, DiGiovanni CW. (2018). Effect of Fixation Type and Bone Graft on Tarsometatarsal Fusion. Foot Ankle Int, 39(12):1394-1402.
Publisher | Google Scholor - Johnson JT, Schuberth JM, Thornton SD, Christensen JC. (2009). Joint curettage arthrodesis technique in the foot: a histological analysis. J Foot Ankle Surg, 48(5):558-564.
Publisher | Google Scholor - Cloward RB. (1961). Treatment of acute fractures and fracture-dislocations of the cervical spine by vertebral-body fusion. A report of eleven cases. J Neurosurg, 18:201-209.
Publisher | Google Scholor - Ryan JD, Timpano ED, Brosky TA, 2nd. (2012). Average depth of tarsometatarsal joint for trephine arthrodesis. J Foot Ankle Surg, 51(2):168-171.
Publisher | Google Scholor - Johnson JE, Johnson KA. (1986). Dowel arthrodesis for degenerative arthritis of the tarsometatarsal (Lisfranc) joints. Foot Ankle, 6(5):243-253.
Publisher | Google Scholor - Withey CJ, Murphy AL, Horner R. (2014). Tarsometatarsal joint arthrodesis with trephine joint resection and dowel calcaneal bone graft. J Foot Ankle Surg, 53(2):243-247.
Publisher | Google Scholor - Roberts TT, Rosenbaum AJ. (2012). Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis, 8(4):114-124.
Publisher | Google Scholor - Claaßen L, Venjakob E, Yao D, Lerch M, Plaass C, Stukenborg-Colsman C, et al. (2021). Erratum: The computed tomography-based anatomy of the ossa cuneiformia. Orthop Rev (Pavia), 13(1):9156.
Publisher | Google Scholor - Dorsey ML, Liu PT, Roberts CC, Kile TA. (2009). Correlation of arthrodesis stability with degree of joint fusion on MDCT. AJR Am J Roentgenol, 192(2):496-499.
Publisher | Google Scholor - Aiyer A, Russell NA, Pelletier MH, Myerson M, Walsh WR. (2016). The Impact of Nitinol Staples on the Compressive Forces, Contact Area, and Mechanical Properties in Comparison to a Claw Plate and Crossed Screws for the First Tarsometatarsal Arthrodesis. Foot Ankle Spec, 9(3):232-240.
Publisher | Google Scholor - Thompson JC, Scott J, Johnson M, Detweiler B, Anderson JM, Hawkins B. (2022). Lesser Tarsal Metatarsal Joint Fusion Using Nitinol Staples, Bone Marrow Aspirate Concentrate, and a Calcaneal Bone Dowel: A Technical Note. Foot Ankle Int.
Publisher | Google Scholor