Case Report
A Rare Case Report of Idiopathic Infected Radicular Cyst
1Implantologist, Private practitioner, India.
2Private Practice, Silver Spring, Maryland, USA.
3Radiologist, Private practitioner, India.
4Oral Pathologist, India.
5Restorative dentist and Endodontist, India.
*Corresponding Author: Lanka Mahesh, Implantologist, Private practitioner, India.
Citation: Mahesh L, Gregori M Kurtzman, Sahai S, Jain A, Paliwal T. (2023). A Rare Case Report of Idiopathic Infected Radicular Cyst. Dentistry and Oral Health Care, BRS Publishers. 2(1); DOI: 10.59657/2993-0863.brs.23.005
Copyright: © 2023 Lanka Mahesh, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 17, 2023 | Accepted: May 01, 2023 | Published: May 08, 2023
Abstract
Peri radicular pathosis can be differentially diagnosed as odontogenic or non-odontogenic cyst, epithelial cyst, neoplastic lesions or non - neoplastic bone lesions and inflammatory lesions. But diagnosis can only be made on the basis of clinical, radiographic features, histopathological evaluation of tissues and cytological evaluation of fluid. In this case report teeth were non vital with radicular cystic lesion size > 10mm. Histological examination revealed presence of cholesterol clefts, foam and giant cells. Enucleation in combination with root canal treatment, GBR with xenograft and membrane helps to get the predictable outcome.
Keywords: radicular cyst; periradicular surgery; histology, cytology; gbr
Introduction
Periapical pathosis occurs due to microorganism within the pulp canal system which releases inflammatory mediators due to which resorption of surrounding bone starts [1]. Carries and traumatic injuries are the most common cause of periapical cyst. Peri radicular pathosis can be differentially diagnosed as odontogenic or non-odontogenic cyst, epithelial cyst, neoplastic lesions or non - neoplastic bone lesions and inflammatory lesions. But the diagnosis can only be made on the basis of clinical, radiographic features, histopathological evaluation of tissues and cytological evaluation of fluid [2].
Pommer et al. stated that trauma induces bleeding and enzymatic activity which causes resorptive changes. Traumatic bone cyst mimics a radicular cyst, despite having an epithelial covering and expansive growth; it has a communication with the root apex. Therefore, it could be referred as a pseudocyst. True periapical cysts do not have communication with the root canal [3].
Likelihood of a periapical cyst is more in cases where the lesion involves more than one tooth, with size >5mm, and microscopic examination of straw-coloured fluid containing cholesterol crystals, necrotic pulp without carious involvement. If the tooth maintains pulp vitality, periapical pathology is of non-endodontic origin. Majority of the periapical lesions can be healed by non-surgical endodontic approach but cystic lesion requires surgical intervention [4].
As in this case report, no history of trauma, clinically no causative factor was present and lesion size was more than 10mm. It’s better to adopt surgical intervention for diagnostic and therapeutic purposes [5]. Although incidences are low but if not treated well, periapical cystic lesion may evolve into metaplasia or dysplasia. The rate of successful healing of periapical surgery has been reported to range from 60% to 91% [6]. Enucleation, marsupialization or a combination of both can be used as surgical modalities. So endodontic treatment followed by peri radicular surgery was planned.
Case Report
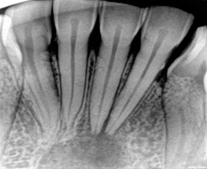
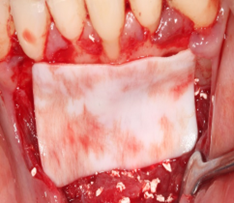
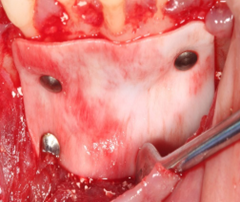
A 33 years old female patient reported to the clinic with mild discomfort in lower front teeth region. On clinical examination, Pulp vitality test showed delayed response in relation to teeth 32, 31 followed by no response in relation to teeth 41, 42. No carious involvement was detected. Tenderness on percussion and fremitus test was negative. No history of previous dental or medical treatment was elicited. Intraoral periapical radiographs were taken (FIG 1). These revealed a well-defined, solitary, unilocular, radiolucent lesion with distinct margins in relation to lower anterior teeth. Patient was advised further imaging work-up with CBCT. CBCT study of the mandible revealed a well-defined, minimally expansile, osteolytic lesion in the mandibular symphysis, Para symphysis regions extending from periapical regions of tooth #32 till #42 region. Lesion measured approx. 6.1mm x 8.8mm x 10.5mm in greatest antero-posterior, transverse and supero-inferior dimensions respectively with distinct and thin, partially corticated margins. Internal structure of lesion was hypodense without internal calcifications or septage. Thinning and effacement of adjoining alveolar labial cortical plate was seen. Associated teeth 31, 32 & 41, 42 revealed intact root outlines. (FIG 2) Imaging findings could be suggestive of differential that includes infected periapical, radicular cyst, traumatic bone cyst, glandular odontogenic cyst, periapical granuloma. Definitive diagnosis can be obtained by histopathological analysis. The treatment plan included root canal treatment followed by surgical intervention, GBR with xenograft and membrane
Figure 1: Pre-operative radiograph demonstrating a large apical lesion associated with the mandibular lateral and central incisors.
Figure 2: Pre-operative CBCT scan of the affected area.
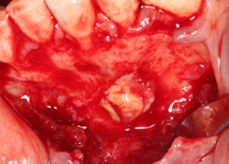
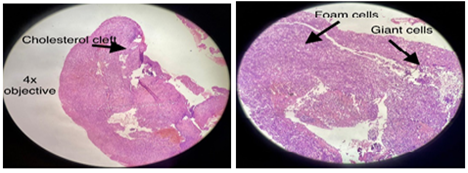
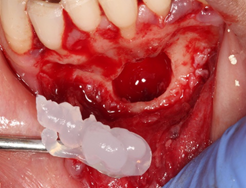
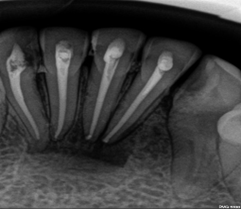
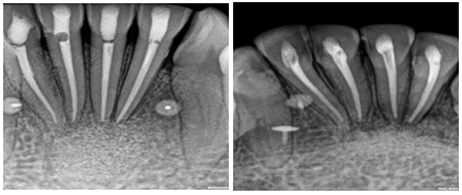
At the first visit, under local anaesthesia and isolation, access preparation was done. Yellow reddish exudate was seen in access cavity irt 31 41 42. All root canals were negotiated with 10K hand file (Dentsply Maillefer, Ballaigues, Switzerland) and biomechanical preparation with crown down technique till 25/.04 (Neo Endo Flex, Orikem, Finland) completed with 5% Na O Cl, 17percent EDTA and saline with ultrasonic activation (eighteenth ultra-X blue tip) irrigation. After drying the canals triple antibiotic paste placed as an intracanal medicament for disinfection of lesion. Swelling was seen after one week, calcium hydroxide as an intracanal medicament was replenished after ultrasonic irrigation. On 3rd visit, after 14 days, surgical intervention was done. Papilla preservation flap was raised with releasing incision from mesial of 43 to 33. (FIG 3) Full mucoperiosteal trapezoidal flap was raised. Immediately, pus discharge was seen from exposed underlying lesion. (FIG 4) Erosion of buccal bony plate area was present. Enucleation was done. No cystic capsule was found. Tissue was collected and sent for histopathological evaluation. (FIG 5) Obturation done under sterile condition with gutta percha points and Seal apex (Kerr Dental, Orange, CA, USA) followed by apicoectomy and retrograde filling with MTA (Angelus). (FIG 6) Access cavity was restored with composite resin. Bony cavity was sterile again by placement of blue m gel (Blue M care) for 10-12 mints. (FIG 7) With fresh bleeding particulate xenograft (Tio-oss, Gyenggido, Korea) were gently packed (FIG 8 & 9) apically and buccally, and then an absorbable collagen membrane (FIG 10) (Creos, Nobel BioCare, Kloten, Switzerland) was secured with titanium tacks (Bioner, Spain) (FIG 11). Flap was repositioned, closed and sutured with PTFE non -resorbable suture 3-0 (FIG 12 & 13) (Cytoplast, Osteogenic Biomedical, TX, USA). After one-week sutures were removed. Six month follow up was uneventful demonstrating conversion of the osseous graft material to blend with the adjacent host bone (FIG 14).
Figure 3: Initial incision to preserve the papillae.
Figure 4: Presentation of the lesion upon reflection of a full thickness flap.
Figure 5A & 5B: Histopathological presentation of the biopsy as viewed at 4x (left) and 10x (right).
Figure 6: Cystic cavity upon enucleation of the lesion and apicoectomy with MTA retrograde filling of the four apex.
Figure 7: Decontamination of the operative site with Blue M gel.
Figure 8: Ti-Oss bone graft being placed into the enucleated cystic cavity.
Figure 9: The graft was packed to completely fill the cystic cavity.
Figure 10: A Creos membrane was placed to overlay the graft material and adjacent host bone.
Figure 11: The membrane was secured with titanium tacs.
Figure 12: The flap was repositioned and secured with 3-0 Cytoplast sutures.
Figure 13: Radiograph immediately following surgical treatment.
Figure 14: Radiograph at 6-months post-surgical treatment demonstrating conversion of the osseous graft to blend with adjacent host bone.
Microscopic Analysis
Submitted H and E-stained section shows the presence of fibro cellular connective tissue stroma with dense infiltration of chronic inflammatory cells predominantly composed of lymphocytes and plasma cells. Areas showed the presence of multinucleated gains cells along with the presence of granular appearing foam cells with pale cytoplasm. Cholesterol clefts were present in few areas of the section. Blood vessels of varying shape and sizes are evident along with entrapped RBC’s and haemorrhagic areas.
Table 1: On the basis of histopathological features following differential diagnosis was considered.
| Features | Central Giant cell Granuloma | Aneurysmal bone cyst | Traumatic bone cyst | Radicular cyst | Present ease |
| Stratified Squamous epithelium showing arcading Pattern | x | x | x | ✓ | x |
| Chronic inflammatory Reaction | ✓ | ✓ | ✓ | ✓ | ✓ |
| Presence of Giant cells | ✓ | ✓ | ✓ | ✓ | ✓ |
| Cholesterol clefts | x | x | x | ||
| Presence of bony trabeculae showing areas of Resorption | ✓ | ✓ | ✓ | x/✓ | x |
| Presence of Hemosiderin Pigment | x | x | x | ✓ | ✓ |
| Necrotic or Myxoid areas | x | x | ✓ | x | x |
| Foam Cells | x | x | x | ✓ | ✓ |
Discussion
Although, pulp is a sterile tissue but invasion of microorganisms along with progression of inflammation due to pulpal injury leads to peri radicular changes or may cause resorption [7]. Similarly, Dental trauma is one of the factors which are responsible for immediate or delayed pulpal injury followed by necrosis or periapical lesion. CBCT is an imaging tool to visualize 3D morphologic features, pathologies and its treatment planning along with assessment of treatment outcomes [8]. However, histopathology only, is considered to be the “gold standard” for achieving confirmatory diagnosis. According to Von Arx classification this case was allocated to 1b category for endodontic surgery [9].
In this case teeth were asymptomatic and radiological differentials included traumatic bone cyst, periapical granuloma, or glandular odontogenic cyst. There was no history, signs and symptoms of trauma. Due to minimal cortical expansion and thinning-effacement, the lesion could have been mistaken for a karate cystic odontogenic tumor, if it were larger in size and extending till body of mandible [10]. Majority of cystic lesions cause bony expansion along with no loss of pulpal vitality except inflammatory periodontal cyst or radicular cyst. Preserved vitality of associated teeth and no change in their positions also suggested otherwise. Teeth with traumatic bone cyst do not show change in vitality [7]. Simple or traumatic bone cyst was also excluded because these lesions are not associated with the tooth/teeth apices and have intact epithelial lining. Granulomas are usually solid soft tissue lesions while cysts are semi solid or liquefied areas.
In this case, non-vital teeth, with lesion size larger than 10mm, continuity with root apex are more likely to be suggestive of a radicular cyst. It is a type of inflammatory jaw cyst which originates from epithelial remnants of PDL as a result of consequences of pulpal necrosis. Surgical intervention was needed for the same. Histological examination was required for definitive diagnosis which revealed presence of cholesterol clefts, foam cells and giant cells. It has been reported 60-70% lesion measuring 10-20mm in diameter, 29-43
Conclusion
Asymptomatic idiopathic lesion needs to be evaluated thoroughly with all possible means of diagnosis. Bone graft, membrane with retrograde filling with bio ceramic materials enhances bone regeneration with predictable treatment outcomes. This case report reveals satisfactory post-surgical result in teeth with primary endodontic involvement.
References
- Trope M, Pettigrew J, Petras J, Barnett F, Tronstad L. (1989). Differentiation of radicular cyst and granulomas using computerized tomography. Endod Dent Traumatol, 5:69-72.
Publisher | Google Scholor - Paul V. Abbott. (2004). Classification, diagnosis and clinical manifestations of apical periodontitis. Endodontic topics, 8:36-54.
Publisher | Google Scholor - Gallego D, Torres D, García M, Romero MM, Infante P. et al. (2002). Diagnóstico diferencial y enfoque terapéutico de los quistes radiculares en la práctica odontológica cotidiana. Medicina Oral B, 7:54-62.
Publisher | Google Scholor - Natkin E, Oswald RJ, Carnes LI. (1984). The relationship of lesion size to diagnosis, incidence, and treatment of periapical cysts and granulomas. Oral Surg Oral Med Oral Pathol, 57(1):82-94.
Publisher | Google Scholor - Mead C, Javidan-Nejad S, Mego ME, Nash B, Torabinejad M. (2005). Levels of evidence for the outcome of endodontic surgery. J Endod, 31(1):19-24.
Publisher | Google Scholor - Reit C, Hirsch J. (1986). Surgical endodontic retreatment. Int Endod J, 19(3):107-112.
Publisher | Google Scholor - Karamifar K, Tondari A, Saghiri MA. (2020). Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur Endod J, 5(2):54-67.
Publisher | Google Scholor - Ludlow JB, Ivanovic M. (2008). Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 106:106-114.
Publisher | Google Scholor - Von Arx T, Cochran DL. (2001). Rationale for the application of the GTR principle using a barrier membrane in endodontic surgery: a proposal of classification and literature revie. Int J Periodontics Restor Dent, 21:127-139.
Publisher | Google Scholor - Olech E, Sicher H, Weinmann JP. (1951). Traumatic mandibular bone cysts. Oral Surg Oral Med Oral Pathol, 4:1160-1172.
Publisher | Google Scholor - Grzesik WJ, Narayanan AS. (2002). Cementum and periodontal wound healing and regeneration. Crit Rev Oral Biol Med, 13:474-484.
Publisher | Google Scholor - J.F. Siqueira Jr., H.P. Lopes. (1999). Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J, 32:361-369.
Publisher | Google Scholor - Schwarz F, Mihatovic I, Ghanaati S, Becker J. (2017). Performance and safety of collagenated xenogeneic bone block for lateral alveolar ridge augmentation and staged implant placement. A monocenter, prospective single-arm clinical study. Clin Oral Implants Res, 28:954-960.
Publisher | Google Scholor - Lin L, Chen MYH, Ricucci D, Rosenberg PA. (2010). Guided tissue regeneration in periapical surgery. J Endod, 36:618-625.
Publisher | Google Scholor - Mahesh L, Kurtzman GM, Shukla S. (2015). Regeneration in Periodontics: Collagen-A Review of Its Properties and Applications in Dentistry. Compend Contin Educ Dent, 36(5):358-363.
Publisher | Google Scholor