Research
A Rare Case of Placental Site Trophoblastic Tumor
- Yapa Wijeratne *
- Chintana Hapuachchige
- Madara Ojithmali
- Namal Wickramasinghe
- Sanjaya Nagasinghe
National Cancer Institute (Apeksha Hospital), Maharagama, Sri Lanka.
*Corresponding Author: Yapa Wijeratne,National Cancer Institute (Apeksha Hospital), Maharagama, Sri Lanka
Citation: Wijeratne Y, Hapuachchige C, Ojithmali M, Wickramasinghe N, Nagasinghe S. (2023). A Rare Case of Placental Site Trophoblastic Tumor. International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(3); DOI: 10.59657/2837-8172.brs.23.025
Copyright: © 2023 Yapa Wijeratne, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 21, 2023 | Accepted: July 12, 2023 | Published: July 17, 2023
Abstract
Placental site trophoblastic tumor (PSTT) is a rare entity of malignant gestational trophoblastic neoplasia (GTN) with an incidence of 0.23 to 3% of all gestational trophoblastic diseases (GTD). They originate from intermediate trophoblastic cells of the placenta. They are slow-growing tumors and less chemo sensitive. Per vaginal bleeding following a miscarriage is not uncommon, however malignant variants of gestational trophoblastic neoplasia also could be a possibility. We are reporting a 24-year-old who was an otherwise healthy female who presented with persistent per vaginal bleeding following the first-trimester miscarriage in her second pregnancy. Initial histology of suction evacuation for her miscarriage has shown a partial mole. Since she continues to have per vaginal bleeding even a month later, repeat evacuation was done and beta hCG was high (2132mIU/ml), she was treated with a methotrexate regime. During follow up there was a slow rising of beta hCG level and hysterectomy was carried out due to the suspicions of invasive mole or PSTT. Histology confirmed a placental site trophoblastic tumor and her recovery and follow-up were uneventful.
Keywords: gestational trophoblastic neoplasia; pstt; rare gynecological tumors
Introduction
Placental site trophoblastic tumor (PSTT) is a rare entity of malignant gestational trophoblastic neoplasia (GTN). The incidence is 0.23 to 3% of all gestational trophoblastic diseases (GTD) [1].
Cell proliferation in GTD is produced by the placental trophoblast cells which are composed of syncytiotrophoblasts, cytotrophoblasts, and interme-diate trophoblasts. Syncytiotrophoblast cells are multinuclear cells that form outer layers, primarily producing human chorionic gonadotropin (hCG) and invading the endometrial stroma. Cytotrophoblast cells, which form the basal layer, can differentiate into syncytiotrophoblastic cells or intermediate tropho-blastic cells. Intermediate trophoblastic cells leave the placenta and restructure the spiral arteries to reduce resistance to blood flow toward the placenta [2]. PSTT originates from these spiral arterioles [3]. Case series have shown the average age of the patient is around 32 years [4]. Clinical presentation often varies including amenorrhea, bleeding per vagina, uterine rupture, abdominal pain, post-menopausal bleeding, or metastatic symptoms [5]. Lung, liver, and vagina are the most common sites of metastasis [5]. The level of serum β-hCG in PSTT is usually under the measurable limit or slightly elevated unlike other GTNs like Invasive mole or choriocarcinoma due to the absence of syncytiotrophoblastic cells [6]. In 97% of patients have shown β-hCG levels below 400 Miu/mL [7]. Imaging is used for the anatomical stage in FIGO staging where the uterine confined disease is staged I and spread beyond lungs with or without genital tract involvement is staged IV [8]. Transvaginal ultrasound in PSTT has shown solid, cystic, or cystic-solid lesions with ill-defined borders and non-peripheral, abundant echo-color Doppler [9]. Magnetic resonance imaging (MRI) is useful for myometrial invasion and whole-body computerized tomography (CT) or PET-CT are especially useful in staging including pulmonary metastasis [1]. Hysterectomy is the mainstay of the treatment since they are less chemo sensitive while uterine curettage, hysteroscopic resection, or chemotherapy could be an option in situations where fertility preservation is concerned and the disease is focal [8]. Oophorectomy is not indicated unless there is a family history of ovarian cancer or menopause [1]. The lymphatic metastasis is 5.9% at the time of diagnosis or the recurrence in PSTT [5]. Hence lymph node sampling is recommended by many authors [1]. Etoposide, cisplatin, methotrexate, actinomycin-D, or paclitaxel with cisplatin, or etoposide can be used as adjuvant treatment in advanced-stage disease [8].
Case History
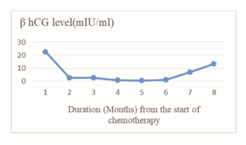
Twenty-four-year-old who was an otherwise healthy Sinhalese female, presented with persistent per vaginal bleeding following the first-trimester miscarriage in her second pregnancy. She had a term vaginal delivery in her first pregnancy which had an uneventful antenatal and postnatal period 6 years ago. She was on oral contraceptive pills for 5 years for contraception and stopped for one year and planned her next pregnancy. Her menstrual cycles were regular 28 days with normal flow and had no dysmenorrhea. At 8 weeks of period of amenorrhea, she experienced mild spotting and the ultrasound was suggestive of retained products of conception or partial mole. The suction evacuation was done and histology showed a partial mole. As she continued to have per vaginal bleeding even a month later, ultrasound-guided repeat suction evacuation was carried out. Her postoperative serum β-hCG was 2132mIU/ml and she was treated with a methotrexate (MTX) regime. Serum β-hCG level plunged to 22.6mIU/ml in a month following the MTX treatment. Serum β-hCG levels were monitored monthly and noted rising serum β-hCG levels (Figure 1) while on follow-up after nine months of the repeat evacuation.
Figure 1:Serum β-hCG level change following the MTX treatment
Her magnetic resonance imaging demonstrated the area of signal change within the uterine cavity mainly on the right side of the fundus possibly infiltrating into the inner layer of the myometrium. There were multiple areas of signal change suggestive of abnormal blood vessels seen within the adjacent myometrium raising the overall picture of the suspicion of residual trophoblastic disease. No suspicious lymphadenopathy was noted. The possibility of PSTT or invasive mole was the concern. Following the multidisciplinary discussion and thorough counseling, she underwent a total abdominal hysterectomy and bilateral salpingectomy while preserving both ovaries. She had an uneventful post-operative recovery.
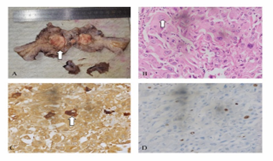
Figure 2: Histology revealed PSTT.
A: Macroscopy of the specimen. Cut surface of the uterus shows a circumferential mass involving the fundus and body of the endometrial cavity. It is tan in color (arrow) with a few hemorrhagic areas. Tumor measures 30 x 25 x 26 mm. B: Microscopy with H& E stains (magnification x 400). The nuclei are pleomorphic with a prominent nucleolus (arrow). The cytoplasm is abundant and eosinophilic. Scattered bizarre cells are seen. C: Microscopy with beta-hCG stain. Scattered tumor cells show strong cytoplasmic positivity (arrow) for beta-hCG. D: Microscopy with Ki-67 proliferation index is 19%. Histology (Figure 2) confirmed the diagnosis of placental site trophoblastic tumor and the tumor size was 30 x 26 x 25 mm with 10% of myometrial invasion. There were no chorionic villi but vascular tumor emboli and areas of necrosis were present. The lower uterine segment was not involved by the tumor. Immunopurified revealed scattered tumor cells showing strong cytoplasmic positivity for beta hCG and Ki67 proliferation index was 19%.
Discussion
PSTT is a rare and slow-growing malignant tumor. They are less chemo sensitive, hence hysterectomy is the option. Clinicians should be alert to the possibility of post-molar gestational trophoblastic neoplasia following any pregnancy event who presents with persistent per vaginal bleeding. Therefore, in a young patient, fertility preservation could be an option if detected early. However, the initial clinical picture could be quite non-specific. Obtaining oncology opinion promptly in cases where the β-hCG levels are abnormally high or slowly rising can initiate chemotherapy by the expert clinicians. Hence the patient is likely to receive a proper follow-up. Her β-hCG levels were within the normal range at the time of the hysterectomy, yet it was slowly rising. The decision; whether to arrange watchful follow-up versus the risk of malignancy and metastasis, was extensively discussed at the multidisciplinary meetings. Even in a low-resource setting, detailed cross-sectional imaging without a delay has led to proper staging which helped to plan the surgical procedure. Lymphadenectomy was not carried out in this patient as MRI has not shown suspicious lesions. Her post-operative β-hCG levels were normal and no adjuvant treatment was offered.
Acknowledgments
Authors would like to thank Dr (Mrs.) Priyanka Abeygunasekara, Consultant histopathologist, department of pathology, National Cancer Institute for providing histology images and explanations.
References
- De Nola R, Schönauer LM, Fiore MG, Loverro M, Carriero C, Di Naro E. (2018). Management of placental site trophoblastic tumor: Two case reports. Medicine (Baltimore), 97(48):13439.
Publisher | Google Scholor - Lurain JR. (2010). Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol, 203(6):531-539.
Publisher | Google Scholor - Hui, P, Wang, H. L, Chu, P, Yang, B, Huang, J, Baergen, R. N, Sklar, J, Yang, X. J, & Soslow, R. A. (2007). Absence of Y chromosome in human placental site trophoblastic tumor. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc, 20(10):1055-1060.
Publisher | Google Scholor - Baergen, R. N, Rutgers, J. L, Young, R. H, Osann, K, & Scully, R. E. (2006). Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance. Gynecologic oncology, 100(3):511-520.
Publisher | Google Scholor - Bouquet de la Jolinière, J, Khomsi, F, Fadhlaoui, A, Ben Ali, N, Dubuisson, J. B, & Feki, A. (2014). Placental site trophoblastic tumor: a case report and review of the literature. Frontiers in surgery, 1:31.
Publisher | Google Scholor - Zeng, X, Liu, X, Tian, Q, Xue, Y, & An, R. (2015). Placental site trophoblastic tumor: A case report and literature review. Intractable & rare diseases research. 2015; 4(3), 147-151.
Publisher | Google Scholor - Hassadia, A, Gillespie, A, Tidy, J, Everard R G N, J, Wells, M, Coleman, R, & Hancock, B. (2005). Placental site trophoblastic tumour: clinical features and management. Gynecologic 99(3):603-607.
Publisher | Google Scholor - Ngan, H, Seckl, M. J, Berkowitz, R. S, Xiang, Y, Golfier, F, Sekharan, P. K, Lurain, J. R, & Massuger, L. (2021). Diagnosis and management of gestational trophoblastic disease: 2021 update. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 155(1):86-93.
Publisher | Google Scholor - Zhu Y, Zhang GN, Zhang RB, et al. (2017). Sonographic image of cervix epithelioid trophoblastic tumor coexisting with mucinous adenocarcinoma in a postmenopausal woman: A case report. Medicine (Baltimore), 96(38):7731.
Publisher | Google Scholor