Case Report
A Rare Case of Heterotopic Pregnancy with Ruptured Rudimentary Horn Pregnancy: A Case Report
- Yismaw Yimam Belachew *
- Zemen Asmare Emiru
- Yosef Gebremedin kassie
- Akilog Almaw Yigzaw
- Mulugeta Wondimu kedimu
- Adisu Alem Nigatu
Faculty of Medicine, College of Medicine and Health Sciences, Debre-Tabor University, Debre-Tabor, Ethiopia.
*Corresponding Author: Yismaw Yimam Belachew, Faculty of Medicine, College of Medicine and Health Sciences, Debre-Tabor University, Debre-Tabor, Ethiopia.
Citation: Belachew Y Y, Emiru Z A, Kassie Y G, Yigzaw A A, kedimu M W, et al. (2024). A Rare Case of Heterotopic Pregnancy with Ruptured Rudimentary Horn Pregnancy: A Case Report. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 4(1):1-4. DOI: 10.59657/2993-0871.brs.24.048
Copyright: © 2024 Yismaw Yimam Belachew, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 25, 2024 | Accepted: June 25, 2024 | Published: August 10, 2024
Abstract
Introduction: Pregnancy in the rudimentary horn is an extremely rare obstetric complication that usually result in rupture in the second trimester. The incidence of intrauterine pregnancy in unicornuate uterus and associated rudimentary horn pregnancy is estimated to be around one in ten million gestations.
Case presentation: A 22 years-old gravid II para I (alive) women presented to our hospital with compliant of severe lower abdominal pain of 24-hours duration. There were no signs of vaginal bleeding. She had no previous ultrasound reports. The physical examination revealed severe pallor with pulse rate-128beats /minute, and blood pressure-80/50 mmHg. A distended abdomen with diffuse tenderness and a positive sign of fluid collection was discovered during an abdominal examination. Ultrasound revealed significant intra-abdominal fluid collection in the peritoneal cavity and a 22-weeek intrauterine pregnancy with positive cardiac activity. A 22-week-old fetus with negative cardiac activity is seen in the right uterine fundus. Emergency laparotomy was done.
It was discovered intraoperatively that there was a ruptured right Rudimentary Horn Pregnancy with a 500gram dead fetus inside the Rudimentary Horn and a 22week sized unicornuate uterus that was not communicating. There was approximately 1700 mL of hemoperitoneum. A rudimentary horn resection was performed, along with a right salpingectomy. The patient was discharged without any complications.
Conclusion: There should be a high index of suspicion for this rare complication because it is frequently associated with high maternal and fetal loss if treated late.
Keywords: uterine anomalies; rudimentary horn; heterotopic pregnancy
Introduction
Uterine anomalies are estimated to affect approximately 5.5% of the population, with a higher prevalence among women with infertility and a history of miscarriage (8.0% and 13.3%, respectively) [1]. Buttram and Gibbons classified Mullerian anomalies for the first time in 1979, and the American Society of Reproductive Medicine later revised their classification. Unicornuate uterus is a type 2 uterus with unilateral hypoplasia or agenesis that can be further classified as communicating, non-communicating, without a cavity, and without a horn [2]. A unicornuate uterus accounts for 2.4%–13% of Mullerian anomalies. Near to 72–85% of the rudimentary horns are non-communicating. Pregnancy in a rudimentary horn is an extremely rare phenomenon that, if ruptured, can have disastrous consequences. The majority of cases are discovered after the rupture. This type of pregnancy occurs in approximately 1 in 76,000 to 1in 140,000 pregnancies. Pregnancy in a non-communicating horn occurs by trans peritoneal migration of spermatozoa or the fertilized ovum [2, 3]. We report one rupture rudimentary horn pregnancy diagnosed at 22 weeks with alive gestation in unicornuate uterus.
Case Report
A 25-year-old gravida II para I (alive) mother who had been amenorrheic for the previous 5 months. She was referred to our hospital by a rural health center with a diagnosis of 2nd trimester pregnancy plus acute abdominal pain due to a ruptured uterus. Three years ago, she had an uneventful vaginal delivery of a 2.8kg baby. She presented with severe lower abdominal pain that had lasted 24 hours. She also experienced fatigue, vertigo, and lightheadedness. She didn't have any vaginal bleeding, fever, headache, chills, or discharge. She had not yet detected fetal movement. She received no antenatal care. On physical examination, she appeared acutely sick, agitated, and confused. Her vital signs were as follows: blood pressure: 80/50 mmHg, pulse rate: 128 beats per minute, respiratory rate: 24 breaths per minute, and temperature: 37.3 degrees Celsius. Her conjunctiva was paper white, and she had a dry tongue and buccal mucosa. The chest was clear and resonant. There was an S3 gallop heard.
Abdominal examination revealed distended tense abdomen with diffuse tenderness and positive sign of fluid collection. On pelvic examination, the cervix was closed and there was no blood on the examining finger. An ultrasound examination revealed significant intra-abdominal fluid collection in the peritoneal cavity and a 22-week intrauterine pregnancy with positive cardiac activity. A 22-week-old fetus with negative cardiac activity was seen in the right side of the uterine fundus (Figure 1). The liver and both kidneys were otherwise grossly normal. With the impression of hypovolemic shock due to acute blood loss due to a ruptured rudimentary horn pregnancy, to rule out abdominal pregnancy and severe anemia. The patient was resuscitated with 3 liters of intravenous crystalloids while being prepared for an emergency laparotomy. She was investigated for blood group and Rh (B+) and complete blood count. Her hematocrit was 18%.
Figure 1: Ultrasound shows fetal head with placentaoutside intact uterineoutline.
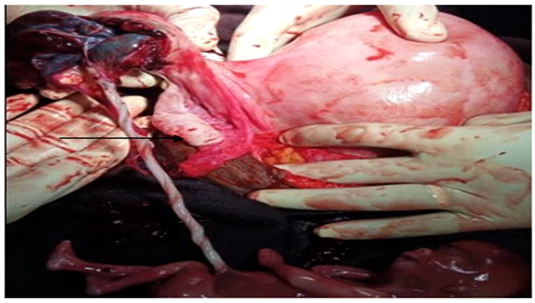
Before taking her to the operating room, four units of cross-matched blood were prepared. Intraoperatively, there was approximately 1700 mL of hemoperitoneum, a ruptured right side rudimentary horn ectopic pregnancy, and the placenta was partially attached to the cavity of the rudimentary horn. Figure 2 shows a 20-week-old unicornuate uterus with a normal ovary and tube (Figure 2), as well as a dead male fetus weighing approximately 500 gm (Figure 3). The rudimentary horn, which had a cavity that was not communicating with the unicornuate uterine cavity and was attached to the placenta, was removed. A rudimentary horn resection and right salpingectomy were performed.
Figure 2: Intraoperative photograph showing the anteriorview of pregnant unicornuate uterus with theruptured right rudimentary horn.
Figure 3: Healthy ovary and fallopiantube
Finally, the stump was examined for any signs of bleeding. Both kidneys were normal in size and location. Finally, the abdominal cavity was mopped and closed in layers. Four units of compatible blood were given to the patient intraoperatively and immediately post operative day. Hematocrit increased to 30%, and anemia symptoms improved after four units of blood transfusions. The post-operative condition was smooth, and the patient was finally discharged on the 5th post-operative date after an ultrasound revealed a normal 2nd trimester pregnancy. She was advised to continue taking ferrous sulfate and was scheduled for another appointment in one month.
Discussion
The paramesonephric ducts, also known as Mullerian ducts, are paired embryonic structures that fuse craniocaudally and later recanalize and develop into the fallopian tubes, uterus, cervix, and upper part of the vagina. During embryonic development, certain malformations can occur, which have been classified by the American Society of Reproductive Medicine. A unicornuate uterus (type II malformation) is classified into four groups based on the presence or absence of functional endometrium and communication [4]. The first case of rudimentary horn pregnancy rupture was reported by Mauriceau and Vassal in 1669. Rudimentary horn rupture, according to Kadan and Romano, is a serious threat to pregnancy and a potentially fatal condition. Pregnancy in a non-communicating rudimentary horn is extremely rare and is thought to be the result of sperm or fertilized ovum trans-peritoneal migration. In the literature, the incidence of twin pregnancy occupying both unicornuate uterus and its associated rudimentary horn is estimated to be 1 in 10 million gestations [3, 5]. A high index of clinical suspicion is essential for early diagnosis prior to rupture. It can be diagnosed using ultrasound or MRI.
Tsafrir et al. suggested the following criteria for detecting a pregnancy in the rudimentary horn: (1) a pseudo pattern of asymmetrical bicornuate uterus; (2) absence of visual continuity between the cervical canal and the lumen of the pregnant horn; and (3) the presence of myometrial tissue surrounding the gestational sac. Ultrasound sensitivity is still only 26-30%. MRI has proven to be a very useful diagnostic tool [6]. The natural fate of ectopic pregnancy in rudimentary horn usually results in rupture during the last two trimesters due to underdevelopment, variable thickness, and poor distensibility of myometrium and dysfunctional endometrium. Most cases remain undiagnosed until it ruptures and presents as an emergency with hemoperitoneum. The mainstay of treatment for rudimentary horn ectopic pregnancy is resection of the rudimentary horn and the ipsilateral fallopian tube via laparotomy or laparoscopy [7]. Early diagnosis before rupture can be managed laparoscopically by immediate excision of the horn, pregnancy, and the ipsilateral fallopian tube. Some authors have described systemic methotrexate administration or feticide with intra-cardiac potassium chloride as alternatives or adjuncts to surgery in the early stages of pregnancy [8, 9].
As demonstrated in this case, surgical management in pregnancy with preservation of the unicornuate uterine gestation is possible in patients with the even rarer clinical complication of a heterotopic pregnancy involving a rudimentary horn. While the ongoing unicornuate uterine gestations in these cases are prone to the complications associated with this anomaly (pregnancy loss and preterm birth), live births at 36–37 weeks have been reported [10].
Renal anomalies are observed in 36% of cases; and hence it is mandatory to further assess these women [11], however, in our case, both kidneys were grossly normal on ultrasound. On discharge, the patients should be advised on future risk of ectopic pregnancy and preterm birth related to this anomaly.
Conclusion
There is a need for increased awareness of this rare anomaly, and thus there should be high index of suspicion for this rare complication as it is often associated with high maternal morbidity and mortality if there is a delay.
Declarations
Data Sharing Statement
All relevant data are within the manuscript, but are available from the corresponding author on reasonable request.
Acknowledgments
Our heartfelt thank goes to those who were involved in the management of this patient. We thank the client for giving us the consent for publication.
Author contributions
YY performed the surgery, and wrote the draft of the manuscript. All authors made significant contributions to the work. They have substantially revised for intellectually important contents of the manuscript. All authors have agreed to take responsibility and accountability for the contents. They gave final approval of the version to be published.
Ethical clearance and consent to participate
As this was a case report, Institutional Review Board approval was not required.
Conflicts of Interest
The authors have declared that they have no competing interests.
References
- Ross ME, Scott S, Behbakht K, Harper T. (2020). Spontaneous dichorionic-diamniotic twins in a noncommunicating uterine horn: A case report. Case reports in women's health, 26:e00177.
Publisher | Google Scholor - Vijay Kumar K. R1 SL, Bharath B. Das. (2015). Ruptured Rudimentary Horn Pregnancy of Unicornuate Uterus. Journal of Evidence based Medicine and Healthcare, 2(22).
Publisher | Google Scholor - Jacob S, Karunakaran L, Devasia N. (2020). Rudimentary horn pregnancy: a rare entity. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 9(4):1761.
Publisher | Google Scholor - Kathpalia S. (2018). Rudimentary horn – different clinical presentations. Obstetrics & Gynecology International Journal, 9(6).
Publisher | Google Scholor - Meenakshi Lallar1 M.D. RNDc. (2015). Unruptured rudimentary horn pregnancy presenting with acute haemoperitoneum with combined intrauterine pregnancy. Iran J Reprod Med, 13(1).
Publisher | Google Scholor - Tesemma MG. (2019). Pregnancy in Noncommunicating Rudimentary Horn of Unicornuate Uterus. Case reports in obstetrics and gynecology.
Publisher | Google Scholor - Hafizi L, Ghomian N. (2019). Twin pregnancy in the unicornuate uterus and non-communicating rudimentary horn: A case report. International journal of reproductive biomedicine, 17(1).
Publisher | Google Scholor - Jha QAaC. (2014). Pregnancy in the Rudimentary Uterine Horn, Case report of an unusual presentation. SQU Medical Journal, 14(1).
Publisher | Google Scholor - Thakur S, Sood A, Sharma C. (2012). Ruptured noncommunicating rudimentary horn pregnancy at 19 weeks with previous cesarean delivery: a case report. Case reports in obstetrics and gynecology, 308476.
Publisher | Google Scholor - Brady PC, Molina RL, Muto MG, Stapp B, Srouji SS. (2018). Diagnosis and management of a heterotopic pregnancy and ruptured rudimentary uterine horn. Fertility research and practice, 4:6.
Publisher | Google Scholor - Kanagal DV, Hanumanalu LC. (2012). Ruptured rudimentary horn pregnancy at 25 weeks with previous vaginal delivery: a case report. Case reports in obstetrics and gynecology, 985076.
Publisher | Google Scholor