Case Report
A Clinical Course of Repeated Supratherapeutic Ingestion of Acetaminophen
- Neelay Shah 1*
- Hunter Campbell
- Vishal Patel
- Jill Moormeier
1Neurology, University of Missouri Kansas City School of Medicine, Kansas City, United States.
2Internal Medicine, University of Missouri Kansas City School of Medicine, Kansas City, United States.
*Corresponding Author: Neelay Shah, Neurology, University of Missouri Kansas City School of Medicine, Kansas City, United States.
Citation: Shah N, Campbell H, Patel V, Moormeier J. (2023). A Clinical Course of Repeated Supra-therapeutic Ingestion of Acetaminophen. Clinical Case Reports and Studies, BioRes Scientia Publishers. 5(6):1-4. DOI: 10.59657/2837-2565.brs.24.132
Copyright: © 2024 Neelay Shah, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 10, 2024 | Accepted: May 24, 2024 | Published: June 03, 2024
Abstract
Acute liver failure (ALF) represents a rapid decline in liver function among individuals with previously healthy livers, often manifesting through symptoms like jaundice, confusion, and potentially life-threatening complications. Timely medical intervention, and in severe instances, liver transplantation, are essential for enhancing outcomes and averting further deterioration. While the causes of ALF are multifaceted, in developed nations, it predominantly arises from drug-induced liver injury. Treatment primarily revolves around supportive measures, with severe cases necessitating liver transplantation. In instances where acute overdose with acetaminophen serves as the instigating factor, N-acetylcysteine (NAC) emerges as a pivotal component of management, as indicated by the Rumack-Matthew nomogram. The Rumack-Matthew nomogram guides treatment for acetaminophen overdose by correlating serum levels with the risk of liver damage. If levels exceed a set threshold, N-acetylcysteine (NAC) is administered to prevent toxicity by replenishing glutathione. The decision to administer NAC is typically guided by this clinical tool, which aids healthcare providers in determining the appropriate course of action. NAC assumes a critical role in ameliorating the detrimental effects of acetaminophen overdose, particularly in averting liver damage, thus holding significant importance in patient care and recovery. While chronic acetaminophen overdose cases leading to ALF may also benefit from NAC, the supporting evidence remains weak. In this context, we present a case of ALF stemming from chronic acetaminophen ingestion, managed with NAC when liver transplantation was not a viable option.
Keywords: N-acetylcysteine; AST; ALT; RSTI
Introduction
Acute liver failure results from an acute injury to the liver, severe enough to impair synthetic function and alter mental status without pre-existing liver disease [1]. There is an extensive list of factors that can cause and/or contribute to liver failure; however, the most common cause in the United States is acetaminophen toxicity [2]. Most occurrences of acute liver failure are from single overdoses, but acute liver failure from chronic acetaminophen ingestion is associated with morbidity and mortality as well [2]. Repeated supratherapeutic ingestion (RSTI) diagnosis can be difficult, as signs and symptoms are often nonspecific and point towards other diagnoses [3]. The therapeutic dose maximum is 4000 mg every 24 hours [1].
Patients who take a single dose of 250 mg/kg or greater than 4g over a 24-hour period without medical supervision are likely to acquire toxicity [4]. Severe liver toxicity is almost inevitable when a patient ingests an excess of 350mg/kg per dose [5]. Severe liver toxicity is defined as peak Aspartate aminotransferase (AST) or Alanine aminotransferase (ALT) greater than 1000IU/L [5]. In addition, clinical factors such as chronic alcohol use, certain other medications, other liver diseases, poor nutritional status, genetics, age, and tobacco use also contribute to the decline in liver function [6]. Here we present a case of acute liver failure caused by repeated supratherapeutic ingestions of acetaminophen, with the patient achieving a full recovery [7].
Case Presentation
Our patient is a 47-year-old female with a history of GERD, gastric Roux-en-Y bypass in 2018, and anastomotic marginal ulcer who was admitted for severe abdominal pain.
On initial questioning, she reported worsening severe epigastric abdominal pain for two months with acute worsening during the past 5 days, which she attributed to her history of marginal ulcer. She also had non-bloody vomitus and black stools in the two days prior to presentation. Her pain had been initially well controlled using therapeutic doses of acetaminophen, but in the last week she had required additional doses of acetaminophen to control her pain. She estimated taking 1-2 tablets of 500mg acetaminophen every 2-3 hours over the past week (dose equivalent to 6000-12000mg total/day). Upon presentation, she was mildly tachycardic but with other vital signs within normal limits. Her labs were significant for an AST (Aspartate Aminotransferase) of 1899 IU/L (normal range: 8 to 48 IU/L) and ALT (Alanine Aminotransferase) of 533 IU/L (normal range: 7 to 56 IU/L), indicating severe liver damage. The INR (International Normalized Ratio) was within the normal range at 1.0 (normal range: 0.8 to 1.2), suggesting preserved blood clotting function. Her hemoglobin level was 11.1 gm/dL (normal range: 12.0 to 15.5 gm/dL), reflecting a slightly decreased level of red blood cells.
Additionally, her serum acetaminophen level returned at 29 mcg/ml, and a urine drug screen was positive for cocaine. In response to these findings, she was initiated on pantoprazole, Lactated Ringer's solution at 75 ml/hr, and N-acetylcysteine, aligning with the standard management protocol for acetaminophen overdose. The elevated AST and ALT levels underscore the severity of liver involvement, emphasizing the necessity for prompt and comprehensive medical intervention.
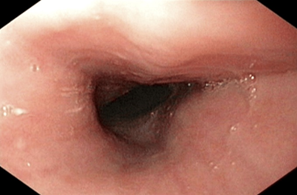
During her admission, she developed jaundice as well as severe elevation of her hepatic transaminases within the 10,000s. Hyperbilirubinemia and an elevated INR suggestive of acute liver failure during hospital day 1 (Table 1) were concurrently noted. She was initiated on a continuous NAC infusion 15 mg/kg/hr for 7 days. Clinical evaluation was notable for normal iron studies, a negative autoimmune panel, and negative serology for viral hepatitis and herpes simplex virus. Mesenteric doppler ultrasound was performed and did not identify portal or hepatic vein thrombosis. With supportive fluids and NAC, her liver function steadily improved with a peak in her LFTs above 10,000, INR at 3.08, and total bilirubin at 22.5 on the 4th hospital day, and then followed by down trending of all labs until normal lab values were achieved. She underwent a scheduled EGD after improvement in hepatic function on 8/15/23 which demonstrated normal appearing esophageal mucosa (Figure 1).
Table 1: Represents correlation between HD with regards to Hgb, Cr, Total Bili, AST/ALT, PT, INR, and Acetaminophen levels; H=High; L=Low
| Dates | 8/9/23 | 8/10/23 | 8/11/23 | 8/12/23 | 8/14/23 | 8/15/23 | 8/16/23 | 8/17/23 | 8/18/23 |
| Hospital Day (HD) | 1 | 2 | 3 | 4 | 6 | 7 | 8 | 9 | 10 |
| Hemoglobin (12.0-15.5g/dL) | L 9.7 | L 8.7 | L 7.5 | L 6.5 | L 5.4 | L 7.7 | L 8.8 | L 7.7 | L 7.7 |
| Creatinine (0.84 - 1.21 mg/dL) | L 0.76 | L 0.79 | L 0.83 | L 0.67 | L 0.69 | L 0.57 | L 0.77 | L 0.67 | L 0.73 |
| Total Bilirubin (0.1-1.2 mg/dL) | 0.9 | H 3.5 | H 13.0 | H 22.5 | H 20.0 | H 4.3 | H 4.3 | H 3.4 | H 2.5 |
| AST (8 - 48 U/L) | 1899 | H>10000 | H>10000 | H 8235 | H 3636 | H 169 | H 93 | H 62 | H 55 |
| ALT (7 - 56 U/L) | H 533 | H 3125 | H>5000 | H 4264 | H 3063 | H 1217 | H 935 | H 694 | H 546 |
| PT (11.0 - 13.0 seconds) | H 28.4 | H 36.0 | H 22.0 | H 15.0 | H 14.2 | H 18.0 | H 15.8 | H 14.5 | H 13.4 |
| INR (0.8 - 1.2) | H 2.38 | H 3.05 | H 1.89 | H 1.28 | H 1.24 | H 1.56 | H 1.37 | H 1.26 | 1.17 |
| Acetaminophen Levels | 20 | 29 | <10> | <10> | <10> | <10> | <10> | <10> | <10> |
Figure 1: EGD Image Representing Normal Appearing Esophageal Mucosa
Discussion
When an individual consumes acetaminophen, it undergoes a transformation and detoxification process in the liver by innate CYP450 enzymes. The liver plays a pivotal role in its subsequent biotransformation. However, prolonged and excessive use of acetaminophen can adversely affect the liver, resulting in significant disruptions to normal functioning leading to harmful consequences. In cases of excessive acetaminophen intake, a specific liver enzyme known as CYP2E1 metabolizes a portion of the drug. Glutathione, an antioxidant present in the liver, plays a vital role in neutralizing NAPQI, a toxic metabolite, by binding to it. Excessive acetaminophen consumption depletes the liver's glutathione reserves, which, in turn, leads to an increase in free radicals within the body. To ensure safety, the U.S. Food and Drug Administration (FDA) recommends that adults should not exceed 12,000 milligrams of acetaminophen per day and should refrain from prolonged use for more than ten days. The presence of metabolites and inflammation resulting from acetaminophen-induced liver damage can disrupt cellular signaling pathways involved in liver regeneration. These pathways are typically mediated by growth factors such as Hepatocyte Growth Factor (HGF) and Transforming growth factor alpha (TGF-α) [6].
Immediate hospitalization and meticulous monitoring are imperative for patients with liver failure to maintain their physiological stability [8, 1]. Priority should be given to care, involving the stabilization of vital signs and the management of complications, such as cerebral edema and changes in mental status [4]. The primary therapeutic objective is to identify and address the underlying cause of acute liver failure [3]. In cases of drug overdose, like acetaminophen, the administration of NAC interventions should be considered [7]. In situations where both acetaminophen and alcohol have been chronically consumed, there is an increased burden on CYP2E1 enzymes, leading to glutathione depletion and an increase in the production of NAPQI [1, 5].
Acute Single Acetaminophen Toxicity Effects
Acetaminophen, a ubiquitous over-the-counter pain reliever, carries a substantial risk when consumed in acute single ingestion exceeding recommended limits [7]. In standard therapeutic scenarios, acetaminophen undergoes glucuronidation and sulfation, yieling benign metabolites [9]. However, in cases of overdose, a significant portion is metabolized by the cytochrome P450 system, culminating in the formation of the hazardous metabolite N-acetyl-p-benzoquinone imine (NAPQI) [8].
The toxic mechanism involves an overwhelming of the liver's detoxification capacity, resulting in hepatocellular necrosis [10]. The severity of liver damage correlates directly with the ingested dose, and acute overdose can swiftly progress to fulminant hepatic failure [7]. Initial symptoms are often nonspecific, encompassing nausea, vomiting, and malaise, but as toxicity advances, patients may manifest right upper quadrant abdominal pain, jaundice, and hepatic encephalopathy [11]. As exemplified in studies such as "Acetaminophen-Induced Hepatotoxicity: a Comprehensive Update" by McGill and Jaeschke (BioMed Research International, 2013), and the pioneering work of Rumack and Matthew in "Acetaminophen Poisoning and Toxicity" (Journal of Pediatrics, 1975), the molecular mechanisms and historical perspective on acetaminophen toxicity to the liver has been proven on a dosage dependent basis [11]. The Rumack-Matthew nomogram is a graphical tool used to assess the risk of liver injury in cases of acute acetaminophen overdose. It plots serum acetaminophen levels against time elapsed since ingestion. If the plotted concentration surpasses a predetermined "treatment line," N-acetylcysteine (NAC) therapy is recommended to prevent liver damage. NAC replenishes depleted glutathione stores, neutralizing the toxic metabolite of acetaminophen. Utilizing the nomogram enables timely intervention and improves patient outcomes by reducing the risk of hepatotoxicity [11]. The primary intervention for acute acetaminophen overdose is the timely administration of N-acetylcysteine (NAC), crucial for replenishing glutathione levels and neutralizing the toxic metabolite [11]. Early initiation of NAC is paramount for a positive outcome, underscoring the significance of prompt medical attention in cases of overdose [9].
Subacute/Chronic Acetaminophen Toxicity with Multiple Doses
In contrast to acute single ingestion, subacute or chronic toxicity emerges from the cumulative effect of multiple doses of acetaminophen over time, surpassing recommended limits [8]. With repeated use, there's an inherent risk of gradual metabolite accumulation, particularly the toxic NAPQI, within the liver [10]. This form of toxicity may present challenges in early detection, as symptoms tend to be subtle and insidious [11]. Prolonged exposure to elevated acetaminophen metabolite levels contributes to ongoing hepatocellular damage, with chronic users possibly experiencing persistent, low-grade symptoms such as fatigue, malaise, and gastrointestinal discomfort [11]. Management of subacute or chronic toxicity necessitates discontinuation of acetaminophen use and vigilant monitoring of liver function [9]. Healthcare providers might consider interventions aimed at enhancing liver detoxification processes [7]. Recognizing the potential harm from prolonged acetaminophen use underscores the importance of adhering to recommended dosages and consulting healthcare professionals if persistent symptoms arise [8]. A study involving 71 hospitalized individuals who had overdosed on acetaminophen revealed a distinction between two distinct groups: those who had accidentally consumed an excessive amount and those who had intentionally used it for self-harm [5]. Surprisingly, the group that accidentally overdosed exhibited a higher incidence of severe liver-related complications, hepatic encephalopathy, and fatalities compared to the individuals who deliberately poisoned themselves [3]. This contrast persisted even though the intentionally self-poisoned group had ingested substantial quantities of acetaminophen [1]. These unexpected findings shed light on the relationship between the method of acetaminophen ingestion and its subsequent impact on the liver [4]. This suggests that different pathways may lead to liver damage based on the clinical circumstances [2].
Conclusion
Most cases of acute liver failure seen in the United States are caused by acetaminophen toxicity, typically from single use overdoses. If discovered in a timely manner, the use of NAC has proven to be beneficial in the recovery of such patients. Compared to its use in acute acetaminophen overdose, the use of NAC has not been well documented in supratherapeutic acetaminophen ingestions, suggesting a possible difference in the pathways leading to liver failure in each circumstance. This case report highlights acute liver failure in a patient who consumed acetaminophen in repeated supratherapeutic quantities and the use of NAC in the management of her care. Further research will need to be conducted to determine if a difference truly exists in the development of liver damage from acute versus subacute supratherapeutic acetaminophen ingestion.
References
- Begriche K, Penhoat C, Bernabeu-Gentey P, Massart J, Fromenty B. (2023). Acetaminophen-Induced Hepatotoxicity in Obesity and Nonalcoholic Fatty Liver Disease: A Critical Review. Livers, 3:33-53.
Publisher | Google Scholor - Bernal W., Auzinger G., Dhawan A. (2010). Acute liver failure. The. Lancet,. 376:190-201.
Publisher | Google Scholor - (2011). European Association for the Study of the Liver: EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol, 55:245-64.
Publisher | Google Scholor - Kamath P; Wiesner R, Malinchoc M: M.D., M.B.A.(2001). A Model to Predict Survival in Patients With End-Stage Liver Disease. Hepatology, 33(2):464-470.
Publisher | Google Scholor - Khanam A, Kottilil S. (2000). Acute-on-Chronic Liver Failure: Pathophysiological Mechanisms and Management. Front Med Lausanne, 8:752875.
Publisher | Google Scholor - Kim WR, Therneau TM, Wiesner RH, et al. (2000). A revised natural history model for primary sclerosing cholangitis. Mayo Clin Proc., 75:688-694.
Publisher | Google Scholor - Fantilli A, López Villa, SD, et al. Hepatitis E virus infection in a patient with alcohol related chronic liver disease: a case report of acute-on-chronic liver failure. Virol J, 18:245.
Publisher | Google Scholor - Osna NA, Donohue TM Jr, Kharbanda KK. (2017). Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol Res., 147-161.
Publisher | Google Scholor - Ozturk NB, Herdan E, Saner FH, Gurakar. (2023) A. A Comprehensive Review of the Diagnosis and Management of Acute Liver Failure. Journal of Clinical Medicine, 12:7451.
Publisher | Google Scholor - Polson J, Lee WM. (2005). American Association for the Study of Liver Disease. AASLD position paper: the management of acute liver failure. Hepatology, 41:1179-1197.
Publisher | Google Scholor - Chan AC, Fan, ST, et al. Liver transplantation for acute-on-chronic liver failure. Hepatol Int., 3:571-581.
Publisher | Google Scholor