Research Article
A Case Study with Six-Week Physiotherapy Rehabilitation Intervention on Intervertebral Disc Prolapse Disorder
Physiotherapist, District Ayurveda Health Center, Hetauda, Makwanpur, Nepal.
Acupuncturist, District Ayurveda Health Center, Hetauda, Makwanpur, Nepal.
Pharmacy assistant, District Ayurveda Health Center, Hetauda, Makwanpur, Nepal.
*Corresponding Author: Rati Kumari Gurung,1Physiotherapist, District Ayurveda Health Center, Hetauda, Makwanpur, Nepal.
Citation: Rati K. Gurung, Syantang B, Maharjan S. (2024). A case study with six-week physiotherapy rehabilitation intervention on intervertebral disc prolapse disorder, International Journal of Medical Case Reports and Reviews, BioRes Scientia Publishers. 3(1):1-6. DOI: 10.59657/2837-8172.brs.24.040
Copyright: © 2024 Rati Kumari Gurung, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 22, 2024 | Accepted: February 08, 2024 | Published: February 12, 2024
Abstract
This article describes the case of an adolescent female with lumbar disc herniation characterized by chronic low back pain (LBP) and antalgic gait. A 27-year-old woman presented with chronic low back pain and subsequent deterioration in her quality of life and impairment in activities of daily living. The patient was evaluated and diagnosed based on her medical history, clinical examination and imaging. She had shown failure in both her symptomatic and functional improvement in natural history and conservative management due to an injury to the facet joint of her lower lumbar spine. Pain radiating to the lower extremities in a young adolescent should be considered, especially in cases of minor trauma or when her LBP becomes chronic. Further research is needed on the long-term effects of such disc injuries in young adults and how best to conservatively manage these patients. Includes discussion of disc herniation pain associated with adolescent disc injuries.
Keywords: disc herniation; rehabilitation; low back pain; physiotherapy
Introduction
Low back pain in children and adolescents is an important and growing problem, with prevalence increasing with age. A systematic review and meta-analysis study on Low Back Pain (LBP) in adolescence found that the mean and 1-year prevalence of LBP in adolescence was approximately 12% and 33%, respectively [1]. Historically, considered trivial and non-limiting, LBP in this age group may have immediate and long-term consequences for most patients. Disc degeneration is considered the most common cause of back pain and work-related disability in people under the age of 45. This is an aging process, and multiple genetic, genetic, environmental, and socioeconomic factors contribute to poor disc health, leading to subsequent degeneration and herniation [2]. Although the symptoms and signs associated with lumbar disc herniation are wide-ranging, the main clinical manifestations are back pain and radicular symptoms in the form of sciatica, loss of sensation, and even decreased mobility, rarely autonomic. Neurologic symptoms may also occur [3]. There is also increasing evidence that physiological and psychosocial factors have a significant impact on the etiology of LBP in this age group [4]. Most cases of LBP in the younger population are considered 'mechanical' and 'uncomplicated', with pathological causes such as neoplasm and infection being very rare. Conservative management and natural history are quite favorable, with the percentage of cases that persist with discomfort longer than one week being less than 15% [5]. Therefore, should a young person diagnosed with uncomplicated LBP not respond as quickly as expected to conservative management, pathological causes should again be considered and further clinical examination undertaken. Additionally, less common, non-pathological causes of low back pain such as 'active' spondylolysis must be re-introduced into the differential diagnosis [5]. An important and probably underappreciated source of LBP in children and young adolescent persons is the intervertebral disc (IVD) joint. Lumbar disc herniation (LDH), encompassing the categories of protrusion, extrusion, and sequestration is well known to cause LBP. Involved in the herniation process are annular tears and other intervertebral joint sources of LBP such as end plate subchondral edema. Multiple factors have been identified as potential causes, with 30–60% of cases of children and adolescents with symptomatic LDH having had a history of trauma before the onset of their LBP [1]. This case study describes a young adolescent patient with chronic intervertebral discogenic Low Back Pain who showed progressive improvement with natural history and conservative management. We discuss intervertebral disc injury in the young age group and clinically relevant pathophysiology of intervertebral disc pain.
Case presentation
Clinical history and examination
A 27-year-old female presented to a District Ayurveda health care center, Makwanpur with a complaining of localized LBP with symptomatic referral into the lower limbs. It was a daily annoyance, particularly worse at night and in the mornings, even affecting her sleep at night. Her pain was described as “achy and annoying”, not allowing her to sit for long periods due to soreness increasing pain with radiculopathy to right lower limb. She could only remember activities from cattle farm on same time her back pain began, but she did not remember it causing her any significant pain or disability at that time. She missed multiple weeks’ activities of household, stopped most physical activities, and was lying on her bed for 4 days continued without any treatment and her relatives took her to hospital. As per the doctor suggestion and observation, she was advised for the MRI scan and referred to higher center for the same. The Scan report showed intervertebral disc prolapsed at L4-L5. She had also been treated sporadically on four occasions at various clinics conservatively with physiotherapy rehabilitation care and acupuncture which included stretching of hamstrings, piriformis and quadriceps muscles, myofascial release and exercises, along with electrotherapy treatment. Both NSAID and manual treatment provided only short-term minimal relief. It was obvious that the patient had not likely been following any recommended plan of management from the previous practitioners. Pertinent examination findings revealed a slightly malnourished, non-distressed, and adolescent with no significant scoliosis or lumbar antalgic in standing neutral position. When prompted, the patient pointed to the right L4–S1 and sacroiliac joint zones as her main area of discomfort. An Adam’s test was performed to assess for scoliosis, in which the patient was asked to bend straight forward and to try and touch his toes. This movement reproduced her LBP and created an abnormal lateral lumbar deviation to the right, appearing at the time to be a possible lumbar scoliotic curve. The patient also stated she could not flex further than shown due to pain levels and a feeling of significant low back stiffness. Active lumbar range of motion (ROM) was additionally painful in all other ranges, particularly extension, localized at the area of chief complaint. Right lumbar Kemp’s test was positive. Bilateral lower limb neurological examination was unremarkable, revealing 2+ patellar and achilles reflexes, intact sensation to light touch of L1 to S2 dermatomes, and 5/5 motor testing of L4 to S1 myotomes. Supine examination revealed a Straight Leg Raise (SLR) test that was negative for lower limb radicular pain production, and limited to 45 degrees bilaterally due to significant hamstring tightness. Anatomical leg length measurement (ASIS to medial malleolus) was 90.0 cm right and 91.0 cm left. Prone examination revealed an estimated right functional short leg of 1 cm, and visually his right hemipelvis was significantly cephalad and superior (heightened off the table) oriented, compared to the left hemipelvis. Right sided upper sacroiliac joint compression test was positive for pain and restriction. Left upper sacroiliac joint compression test was negative for pain but was restricted. Palpation of the right quadratus lumborum, lumbar erector spinae and multifidus muscles revealed significant (3+) hypertonicity and tenderness. Right L4/5 and L5/S1 facet joints were restricted during static and motion palpation. No other orthopedic and manual physical examination findings regarding the hips, pelvis and lower back were remarkable.
Diagnostic and radiology finding
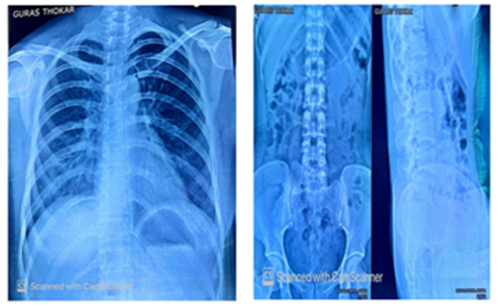
Chest x-ray, hip and lumber regional and MRI scan done for the confirmation of the diagnosis (Figure 1).
Figure 1: Chest x-ray and Lumbo-sacral x-ray.
On the other hand, her AP lumber view x-ray demonstrated on figure 1, the main pelvic ring and associated with pathology and slight posterior displacement of both the main pelvic ring and displacement of pubic symphysis along with the chest x-ray showed the pulmonary tuberculosis.
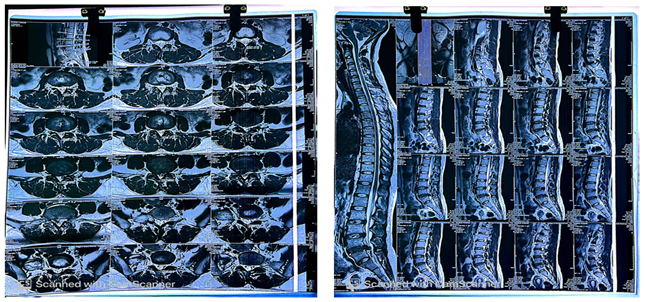
Figure 2: MRI Scan of lumbar spine.
Furthermore, the patient was subsequently referred for MRI examination of the lumbar spine by the doctor to a private facility on the second visit to assess for lower lumbar annulus fibrosus lesion, disc herniation and inflammatory adjacent marrow edema. These lesions were considered possible pain-inducing candidates given the patients clinical picture of chronicity, painful antalgia and night pain. The figure 2, MRI scan showed the intervertebral disc prolapse at level L4-L5 with multiple mild disc bulges at L2-L3, L3-L4 vertebral level and narrowing of the lateral stenosis.
Case management
Six weeks physiotherapy rehabilitation started from the day of health care center visit. Patient was assessed and evaluated for her functional limitation, impairments and activities of daily living. Then she was provided with the consent form to be the part of study and treatment session for 6- weeks started along with acupuncture for speedy recovery. In the initial stage, following the diagnosis of IVDP, the aims of physiotherapy are to: reduce inflammation, reduce pain and spasm maintain soft tissues flexibility, improve core strength, stimulate sensory input, and re-train postural responses. Long term goal is to further strengthen core stability, facilitate effective gait, increase exercise tolerance and overall cardiovascular fitness, return to normal function etc.
Table: The following table is an example of a rehabilitation program for rapid recovery and showed a positive response
| Timescale | Physiotherapy aims | Physiotherapy treatment options |
| 0-4 weeks | Reduce inflammation | Electrotherapy – lumbar traction |
| Reduce muscular guarding | Electrotherapy – TENS | |
| Soft tissue massage | ||
| Heat therapy | ||
| Improve core stability | Home exercise program | |
| Increase strength | Home exercise program | |
| Neuromuscular electrical stimulation | ||
| Core stability exercises | ||
| Increase sensation and awareness of body position | Home exercise program | |
| Maintain soft tissue length and flexibility | Home exercise program – passive movements and stretches | |
| Management at home | Exercise restriction | |
| Advice regarding flooring | ||
| Advice regarding walking with a mobility aid e.g. harness and sling if required | ||
| 4-6 weeks | Continue as above | Progression of home exercise program to challenge balance, body awareness and strength |
| Advice on maintaining restricted. | ||
| 6 + weeks | Increase exercise tolerance | Increase exercise level |
| Continue to increase core stability | Home exercise program | |
| Return to full function | Progress to off-lead exercise and previous exercise level |
Figure 3: Rehabilitation with physiotherapy intervention along with acupuncture
Outcomes measures
The outcomes measures or the assessment tools used for the study was Numerical pain rating scale for the pain, manual muscle testing to check strength of muscles and ODI for Low back pain. The pre- test NPRS, MMT and ODI were 9/10, 3 and 22%. After receiving the physiotherapy treatment, there was significant improvement.
Discussion
Conservative treatment of lumbar disc prolapse has been shown to be of great importance in reducing pain and increasing mobility. We believe that the ability to function and return to work is a key indicator of management success. Therefore, in the current study, we compared functional outcomes and work capacity in patients recently diagnosed with symptomatic disc herniation. The degree of success after a particular treatment may be influenced by patient selection, various outcome variables, follow-up time, and degree and duration of mechanical compression of the disc fragment at the nerve root.
In this study, a 6-week physiotherapy rehabilitation protocol was implemented to minimize disc herniation and reduce pain. Initially, treatment focused on reducing inflammation and maintaining patient's functional activities of daily living. Along with these exercises, plans for rapid recovery were selected and implemented. This case study mainly focuses on two recognized rehabilitation methods that exist to treat back pain. The first is a lumbar stabilization program that emphasizes maintaining a neutral spine position during daily activities, core muscle endurance training, and general functional ability [6,7].
This method of stabilization rehabilitation focuses on strengthening the core. It has been shown to be 80-98
Conclusion
Long-term physiotherapy and rehabilitation programs are beneficial modalities for patients recently diagnosed with disc herniation. Such programs can improve function and facilitate a return to work over earlier surgical inventions. There was rapid recovery with no pain, and increased the mobility and flexibility.
References
- Carter, C.T., Amorin-Woods, L.G. & Doss, A. (2013). Early adolescent lumbar intervertebral disc injury: a case study. Chiropr Man Therap, 21(13).
Publisher | Google Scholor - Gregory DS, Seto CK, Wortley GC, Shugart CM. (2008). Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician, 78:835- 842.
Publisher | Google Scholor - Jones GT, Macfarlane GJ. (2005). Epidemiology of low back pain in children and adolescents. Arch Dis Child, 90:312-316.
Publisher | Google Scholor - Benoist M. (2003). Natural history of the aging spine. Eur Spine J, 12(2): S86-S89.
Publisher | Google Scholor - Dang L, Liu Z. (2010). A review of current treatment for lumbar disc herniation in children and adolescents. Eur Spine J, 19:205-214.
Publisher | Google Scholor - Myrtos C. D. (2012). Low Back Disorders. Evidence-Based Prevention and Rehabilitation. The Journal of the Canadian Chiropractic Association, 56(1):76.
Publisher | Google Scholor - Wetzel FT, Donelson R. (2003). The role of repeated endrange/pain response assessment in the management of symptomatic lumbar discs. The Spine J, 3:146-154.
Publisher | Google Scholor - Wetzel FT, Donelson R. (2003). The role of repeated endrange/pain response assessment in the management of symptomatic lumbar discs. The Spine J, 3:146-154.
Publisher | Google Scholor - Legier L. (2005). Treatment of chronic low back pain incorporating active patient participation and chiropractic: A retrospective case report. J Chiro Med, 4(4):200-205.
Publisher | Google Scholor