Case report
A Case Report: Development of Lyme Arthritis Despite 14 Days of Amoxicillin for Early Lyme Disease
1Department of medicine, University hospital of Lausanne, Lausanne, Switzerland.
2Department of medicine, Semmelweis University Budapest, Hungary.
3Department of Medicine, Szeged University, Hungary.
*Corresponding Author: Noemie Schiever, Department of medicine, University hospital of Lausanne, Lausanne, Switzerland.
Citation: N Schiever, Romina S, Roseanna S. (2023). A Case Report: Development of Lyme Arthritis Despite 14 Days of Amoxicillin for Early Lyme Disease. Clinical Case Reports and Studies, BRS Publishers. 2(1); DOI: 10.59657/2837-2565.brs.23.016
Copyright: © 2023 Noemie Schiever, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 20, 2022 | Accepted: January 12, 2023 | Published: January 20, 2023
Abstract
Objective: The development of Lyme arthritis in children is usually preventable by the administration of appropriate antibiotic treatment. This case report reviews the case of a three-year-old child who developed Lyme arthritis despite beginning antibiotic treatment of amoxicillin a month after the onset of his symptoms.
Method: A review was done by grouping 5 cases that were similar in terms of delayed treatment with a bad outcome. The patients were analyzed based on their demography, symptomatology, clinical course, management, and results.
Results: Of the 5 cases reviewed, 3 were said to have delayed antibiotic treatment, leading to poor results. In two cases, children over 8 years of age were treated with doxycycline and those below the age of 8 with amoxicillin. Those who failed to respond for the second round of treatment were considered to have antibiotic refractory arthritis.
Conclusion: Early treatment of Lyme disease can prevent the development of Lyme arthritis. Earlier treatment within one month of symptom onset prompts a better outcome. Although rare, another factor that should be considered is antibiotic resistance.
Keywords: lyme arthritis; amoxicillin; lyme disease; erythema chronicum; migratory arthralgia
Introduction
Lyme disease is a common vector-born disease caused by the spirochete Borrelia Burgdorferi, spread by ticks belonging to the Ixodes species. It is a multisystemic disease with the characteristic erythema chronicum migrans in the first stage of the disease. In the second and third stage, dissemination of the disease can cause joint, heart and nervous system symptoms and presentation. The incidence of Lyme disease has increased worldwide with changing localization of the vector. In Switzerland, Lyme disease is the most prevalent tick born disease. Lyme arthritis develops in about 15% of the cases of Lyme. Treatment by antibiotics such as doxycycline or amoxicillin has proven to be effective in treating the first stage of the disease and preventing complications. This case report illustrates a case of Lyme arthritis in a young boy in Switzerland despite initial adequate treatment.
Case Presentation
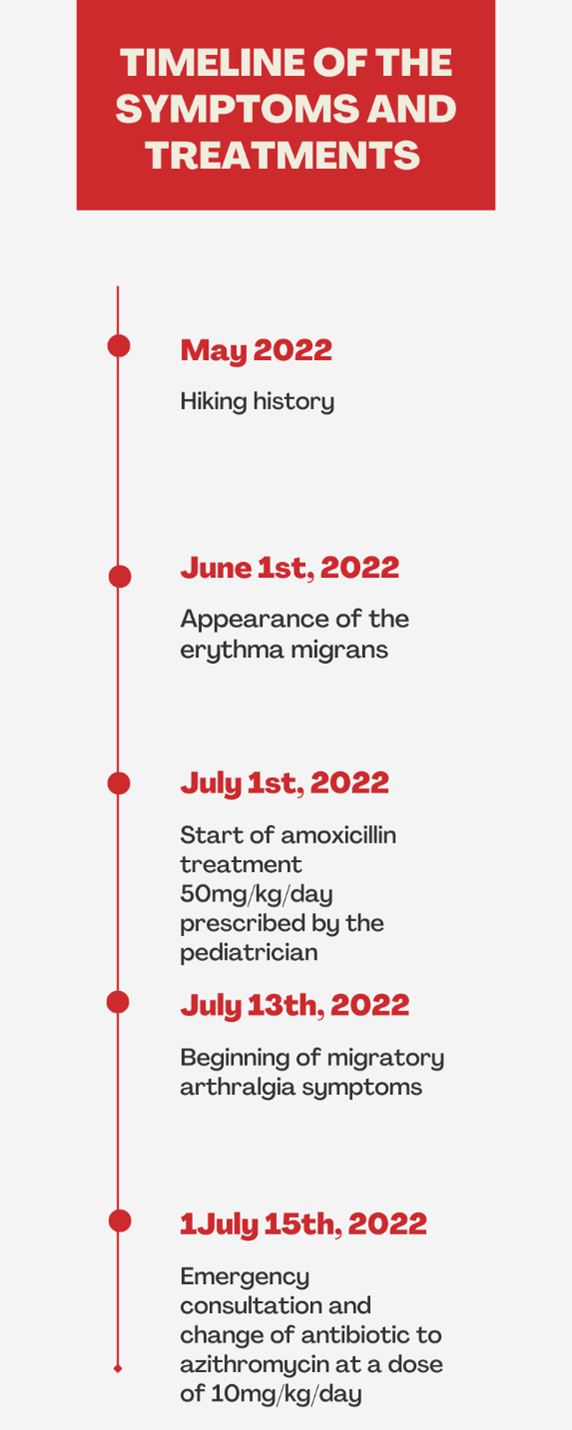
A three-year-old boy otherwise in good general health, presented to the local emergency department in July 2022 for migratory arthralgia developing for the last 2 days with swelling, stiffness and redness of the right knee and right ankle. He avoids putting weight on the right lower limb and refuses to walk. Stiffness and redness of the left elbow also presented earlier during the day. The child did not have fever or any other systemic complaints. Figure 1 presents the timeline of the case.
Previously, he presented 2 weeks ago to his pediatrician with erythema chronicum migrans that had developed for a month (Figure 2). He gave a history of hiking in the North of Switzerland around 4 weeks prior to the eruption but no report of tick bite. He had been on amoxicillin treatment for the past 15 days 50mg/kg/day divided into three doses. The treatment by amoxicillin was started one month after the onset of the erythema chronicum migrans.
Figure 1: Timeline of the symptoms and treatments
Figure 2: Erythema Migrans (1)
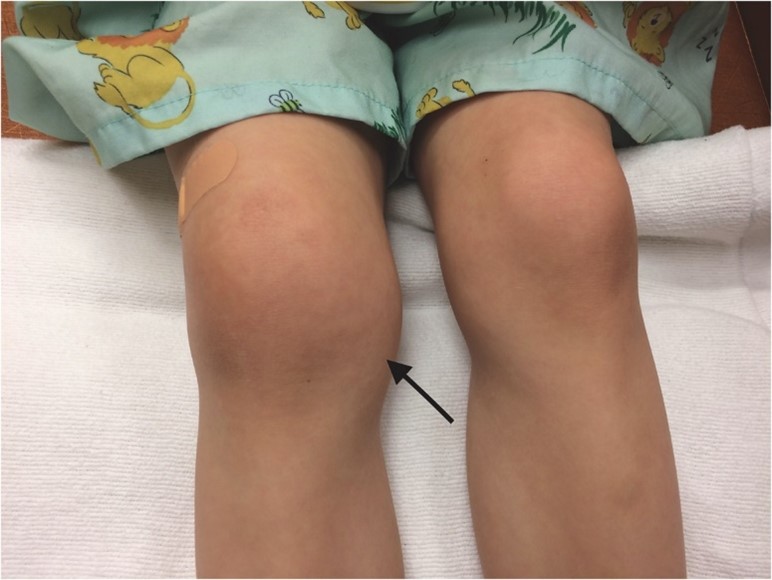
Figure 3: Unilateral right knee swelling (2)
Upon examination, his right knee was swollen and stiff with reduced mobility, showed in figure 3.
At appearance, it was red and hot at touch. His right ankle also showed redness, induration, and tenderness along the deltoid ligament with reduced and painful mobility.
On the abdomen, an erythematous annular plaque was visible approximately 6 x 5 cm in size in decreasing intensity. There were no lymphadenopathies present.
Systemic examination was unremarkable, especially the neurological exam.
As the evolution of the disease progressed from stage 1 with the erythema chronicum migrans to a disseminated stage with migratory arthralgia, we suspected he was presenting clinical signs of Lyme arthritis.
The patient was subject to investigation to confirm Lyme disease. Serology for Borrelia burgdorferi was done using enzyme-linked immunosorbent assay (ELISA) and confirmed with Western Blot (Table 1).
The human antibody response to the VlsE antigenic variation protein of Borrelia Burgdorferi was positive for IgG and IgM [6]. VlsE is a surface lipoprotein on Borrelia Burgdorferi. This antigen is marker of active infection. IgG response for other Borrelia Burgdorferi antigens was also measured (Table 2). The response with IgG and IgM being positive confirmed the diagnosis of an ongoing subacute infection of Lyme.
| Infection | Result | Reference |
| B.b. (VlsE) IgG | positive | negative |
| B.b. (VlsE) IgG quantity | 129 | <10> |
| B.b. (VlsE) IgM | positive | negative |
| B.b. IgG immunoblot | positive | negative |
Table 1: Lyme disease serology results; B.b. = Borrelia Burgdorferi
| Lipid IgG | - |
| p83/100 IgG | + |
| P58 IgG | - |
| P39 IgG | - |
| P20 IgG | + |
| P21 IgG | + |
| P19 IgG | - |
| P18 IgG | - |
Table 2: IgG response to Borrelia Burgdorferi special antigens
Differential diagnosis of septic arthritis was excluded as the patient presented in good general state, with no fever and oligoarticular joint involvement. We concluded the diagnosis of Lyme arthritis considering the positive serology and the polyarticular joint involvement.
We suspected the possibility of resistance to the antibiotic treatment. We decided to change the antibiotics and treatment was initiated immediately prior to the serology results, with azithromycin at a dose of 10mg/kg 1 time per day. The treatment was continued for a total of 28 days.
The patient quickly recovered and presented improvement after 1 week of azithromycin treatment. He was seen by his pediatrician that confirmed the improvement of the above-mentioned features of this patient. The medication was continued for a total of 28 days and resulted in the resolution of the symptoms.
Discussion
Table 3: Literature review table
| Study | Location and Demography | Symptomatology | Clinical course | Management | Results |
| Hirsch et al. 2020 (3) | Pennsylvania, USA (778 respondents) | Rash, observation of tick bite, positive blood test for Lyme disease. | Median time to treatment was 13 days. | Delayed treatment was associated with a higher risk of post treatment Lyme disease syndrome | Prevention of delayed treatment can be used for better outcomes. |
| Sharma et al. 2017(4) | India (10 year old boy) | Brownish lesion with surrounding redness and lymphadenopathy. | 3 weeks | Doxycycline treatment 100mg twice daily | Lesions were cured after 3 weeks of treatment |
| Hirsch et al. 2018 (5) | Pennsylvania, USA (26 participants) | Ten participants had a rash, 3 of which were bulls-eye. Eleven experienced joint pain and fatigue. Eight patients reported Bell’s palsy. Two patients reported carditis and one reported meningitis. | Ten of twenty six patients sought care for their symptoms at an emergency department. Nine were not diagnosed with Lyme disease initially. Seven were misdiagnosed. | Delayed treatment which could lead to complications. | Prevention of delayed treatment can be used for better outcomes. |
| Tory et al. 2015 (6) | USA (99 children from ages 2 to 18 years) | Lyme arthritis with swelling, limited motion, pain. | 5-13 months | Doxycycline for patients over 8 years old and amoxicillin for those below 8 years old. Ceftriaxone and unknown antibiotics were used for 8 patients. | 70 patients were cured with antibiotics. 29 patients failed to respond to initial antibiotic treatment and were given 28 days of PO and IV antibiotics. Those who failed to respond for the second round of treatment were considered to have antibiotic refractory arthritis. |
| Horton et al. 2020 (7) | USA (Children below 18 years old | Fever, joint pain and swelling. | 6-8 weeks | Doxycycline for older patients > 8 years old and amoxicillin for younger patients < 8> | Children with systemic inflammation have more favorable outcomes compared to children with arthritis limited to the knees, older children, and those with poor response to initial antibiotic treatment |
Prompt correct diagnosis and adequate treatment is key for the management of Lyme disease. The course and symptoms of the disease is variable making the diagnosis challenging, as the only specific sign of Lyme disease is erythema migrans chronicum. The presence of this sign confirms the Lyme disease [8]. However, presence of IgM and IgG antibodies against Borrelia Burgdorferi doesn’t confirm the ongoing acute infection as the antibodies can stay positive for years. Diagnosis of Lyme disease and specifically arthritis is primarily based on the medical history, clinical features and exclusion of differential arthritis diagnosis [8].
Lyme arthritis develops in 60% of untreated patients with Lyme disease. However, those treated appropriately for at least 10 days for early Lyme disease had only 1% chance of developing disseminated Lyme disease, which is extremely rare [9]. For our case, Lyme arthritis developed despite treatment by Amoxicillin for 14 days.
Lack of response to the antibiotics could be questioned due to the delayed treatment. The rash appeared 30 days before the introduction of amoxicillin in this patient. In comparison to our outcome, a research article showed that treatment delayed to more than 30 days from the start of the symptoms increased the odds of developing post-treatment Lyme syndrome 2.26 times [3]. In Table 3, we review 5 cases that were similar in terms of delayed treatment followed by bad outcome. The patients were analyzed based on their demography, symptomatology, clinical course, management, and results. We can conclude that longer delay between symptom onset and initiation of antibiotics has been associated with worse outcome. Appropriate treatment, such as administering doxycycline for older patients above 8, and amoxicillin for younger patients below 8 could lead to better results.
The other potential reason that should be suspected for developing Lyme arthritis in our patient is antibiotic resistance. Antibiotic resistance should be considered if the disease involves despite adequate treatment compliance. Treatment by amoxicillin or doxycycline has proved to be effective in the majority of the cases of early Lyme disease and Lyme arthritis. Antibiotic refractory Lyme disease is rare.
However, it has been proven that despite treatment, musculosqueletal symptoms can develop in some cases. It has been shown that immunogenic Spirochaete antigens persist near the cartilage after treatment [10], and being inflammatory, release pro-inflammatory cytokine TNF that causes arthritis [10]. Other occurrences of antibiotic Lyme refractory disease can happen in immunosuppressed patients. Treatment of refractory Lyme arthritis is cefuroxime, azithromycin or IV ceftriaxone [10].
Conclusion
Lyme disease remains a clinical diagnosis that should be made early in the course of the disease to prevent delayed treatment and progression to later stages of the disease. In the literature, only a few cases of Lyme disease progression despite adequate treatment have been reported. Our patient presented with the characteristic erythema migrans, was treated appropriately 30 days following the rash onset and developed Lyme arthritis. This case report highlights the possibility of worse outcome with delayed treatment. Furthermore, our case shows that antibiotic resistance in Lyme disease could be a possibility as our patient got switched to azithromycin and his symptoms improved.
Clinical message
In face of this case report, two problematics were raised.
Health care providers should think of initiating Lyme treatment rapidly within the beginning of symptoms. In our case, the treatment was initiated about a month after the appearance of the erythema chronicum migrans. This delayed therapy could explain the development of Lyme arthritis.
The other issue that was raised was the possibility of antibiotic resistance to Amoxicillin that has to be suspected in case of progression of the disease despite adequate treatment.
Disclaimer
The views expressed in the submitted articles are the authors and not an official position of the institution.
All data generated or analysed during this study are included in this published article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
We confirm that the patient and legal guardian has given their informed consent for the case report to be published.
Availability of data and materials
Not applicable.
Competing interests
Not applicable.
Funding
Not applicable.
Authors' contributions
Both authors worked on all section of the case report. All authors read and approved the final manuscript.
Acknowledgements
Not applicable
References
- Glatz M, Resinger A, Semmelweis K, Ambros-Rudolph CM, Müllegger RR. (2015). Clinical spectrum of skin manifestations of Lyme borreliosis in 204 children in Austria. Acta Derm Venereol. 95(5):565-571.
Publisher | Google Scholor - Guardado KE, Sergent S. (2022). Pediatric unilateral knee swelling: A case report of a complicated differential diagnosis and often overlooked cause. J Osteopath Med, 122(2):105-109.
Publisher | Google Scholor - Hirsch AG, Poulsen MN, Nordberg C, Moon KA, Rebman AW, Aucott JN, et al. (2020). Risk Factors and Outcomes of Treatment Delays in Lyme Disease: A Population-Based Retrospective Cohort Study. Front Med. 7:1-10.
Publisher | Google Scholor - Sharma A, Guleria S, Sharma R, Sharma A. (2017). Lyme disease: A case report with typical and atypical lesions. Indian Dermatol Online J. 8(2):124.
Publisher | Google Scholor - Hirsch AG, Herman RJ, Rebman A, Moon KA, Aucott J, Heaney C, et al. (2018). Obstacles to diagnosis and treatment of Lyme disease in the USA: A qualitative study. BMJ Open. 8(6):1-7.
Publisher | Google Scholor - Tory HO, Zurakowski D, Sundel RP. (2010). Outcomes of children treated for lyme arthritis: Results of a large pediatric cohort. J Rheumatol. 37(5):1049-1055.
Publisher | Google Scholor - Ann L Coker, Nalawansha, Dhanusha A. Pflum MK. (2017). Pediatric Antibiotic-Refractory Lyme Arthritis: A Multicenter Case-Control Study. Physiol Behav. 176(5):139-148.
Publisher | Google Scholor - Strle F, Stanek G. (2009). Clinical manifestations and diagnosis of lyme borreliosis. Curr Probl Dermatol. 37:51-110.
Publisher | Google Scholor - Kowalski TJ, Tata S, Berth W, Mathiason MA, Agger WA. (2010). Antibiotic treatment duration and long-term outcomes of patients with early lyme disease from a lyme disease-hyperendemic area. Clin Infect Dis. 50(4):512-520.
Publisher | Google Scholor - Bockenstedt LK, Gonzalez DG, Haberman AM, Belperron AA. (2012). Spirochete antigens persist near cartilage after murine Lyme borreliosis therapy. J Clin Invest. 122(7):2652-2660.
Publisher | Google Scholor