Case Report
A Case Report: Anaesthesia for Awake Craniotomy
1Anaesthesia Department, King Hamad University Hospital, Kingdom of Bahrain.
2Head of Anaesthesia Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain.
3Neurosurgery Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain.
*Corresponding Author: Ahmed Alanzi, Anaesthesia Department, King Hamad University Hospital, Kingdom of Bahrain.
Citation: Alanzi A., Hakemi S., Adeel S., Hayat F. (2023). A Case Report: Anaesthesia for Awake Craniotomy. Clinical Case Reports and Studies, BRS Publishers. 2(3); DOI: 10.59657/2837-2565.brs.23.032
Copyright: © 2023 Ahmed Alanzi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 20, 2023 | Accepted: May 02, 2023 | Published: May 10, 2023
Abstract
Background: Awake craniotomy is a neurosurgical technique that enables the precise localization of functional neural networks through intraoperative brain mapping and real-time monitoring. This operative method has been popularized in recent years due to decreased postoperative morbidities. We present a case of 31 years old female who was presented with episodes of generalized tonic colonic seizures. She had a history of recurring seizures occurring 2 to 3 times a week. Upon further investigations, she was diagnosed with brain space-occupying lesions initially suspected as low-grade glioma. Considering lesion site, the patient was deemed a suitable candidate for an awake craniotomy. To achieve conscious sedation, the patient received infusions of Remifentanil and Propofol at varying rates. During the procedure, the patient was under sedation and regularly tested for response to predetermined commands. The tumour was successfully excised by using a combination of local anaesthesia on the scalp and the administration of propofol and boluses through a systemic infusion. This case report highlights the importance of the team work among anaesthesia and surgeons where local /regional anaesthesia can be combined with sedation to perform a surgical procedure in certain conditions.
Keywords: seizures; complication; anaesthesia; maintenance; brain
Introduction
Awake craniotomy is an intracranial surgical procedure in which the patient is maintained in a state of partial consciousness [1]. Historically, this procedure has been used for the treatment of seizures and epilepsy. However, it has evolved over the past century to become a widely accepted technique for a range of intracranial conditions such as primarily gliomas due to their close proximity with eloquent areas in the brain [2,3]. Awake craniotomy was first performed under conscious sedation by Wilder Penfield in 1937, who believed that the patient's consciousness and alertness should be preserved through the use of local anaesthesia [4]. He professed that the patient should be able to describe sensations while maintaining minimal pain. In recent times, awake craniotomy has also been employed in various conditions including arteriovenous malformations, supratentorial tumours, and mycotic aneurysms [5,6]. The purpose of this procedure is to accurately localize and remove lesions while simultaneously assessing the patient's motor, sensory, and language capabilities in real time. This improves the post-operative functional neurological status and quality of life [7]. However, the implementation of awake craniotomy presents significant challenges for both neurosurgeons and anaesthetists [8]. The anaesthesiologist must meticulously regulate the administration of sedatives and pain management agents while maintaining respiratory and cardiovascular stability. Simultaneously, the anaesthesiologist must ensure the patient remains conscious and responsive to facilitate accurate neurological assessment [9]. Furthermore, due to the physically and psychologically demanding nature of the procedure, it is crucial to establish a strong relationship of trust between the surgeon, anaesthetist, and patient to ensure a successful outcome [10]. We are presenting a case of 31 years old female who was diagnosed with low-grade glioma after the appearance of recurrent seizures.
Case Presentation
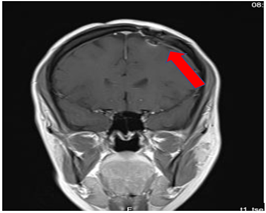
Our patient is a 31-year-old female who presented to the emergency department due to two episodes of generalized tonic colonic seizures. Upon presentation, the patient was administered supplemental oxygen. She was drowsy and confused while exhibiting signs of right-sided hemiparesis and paralysis. Her pupils were 3 mm and reacted briskly while she showed good left-sided localizing. Her seizures terminated after intravenous administration of midazolam at 5mg. Her previous history revealed that she was allergic to dates, bananas, and eggs. Further, it was known that she has been symptomatic for one month and had been suffering from episodes of seizures, with shaking and tremors of upper limbs, and brief episodes of blackouts for about a minute. These episodes were associated with headache and nausea but were self-limited. Seizures recurred 2 to 3 times per week. She denied any fall, tongue bite, Loss of consciousness and limb weakness or numbness. For further investigations, a CT scan was suggested which showed left high parietal hypodensity with vasogenic edema (Figure 1).
Figure 1: Pre-operative CT of the Brain
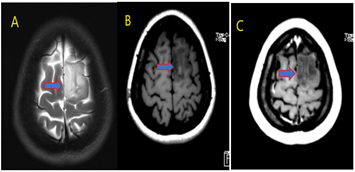
She was recommended Keppra 1.5g and dexamethasone 12 mg. Further, a contrast MRI of the brain was performed. A cortical mass lesion measuring 1.7 cm in length was found in the left frontal lobe/superior frontal gyrus, specifically in the supplementary motor area-medial premotor cortex. The lesion was characterized by mild diffusion restriction and faint minimal contrast enhancement, which was indicative of low-grade glioma. A focal cortical dysplasia (4x5 mm) was identified in the left middle frontal gyrus near the main lesion. This was causing a blurring of the white matter-grey matter junction and an abnormal T1 hypointense and T2 hyperintense pattern in the juxtacortical and subcortical layers. However, there was no obvious trans mantle sign or overlying cortical/sulcal abnormality observed.
Figure 2: MRI brain with contrast [figure (A) T2, Figure(B) T1 and figure (C) T1 post contrast], Space occupying cortical mass lesion in the left frontal lobe/superior frontal gyrus [basically located in the supplementary motor area-medial premotor cortex {cortical mass vertical length (1.7 cm) [figure A T2 WI] with subcortical-surrounding vasogenic edema}] showing mild faint minimal contrast enhancement [figure C] [? low grade glioma]
After a thorough evaluation of the patient's medical records and current condition, it was decided to proceed with an excision of the tumor using Awake Craniotomy and 5-Aminolevulinic acid guidance (Table 1). To foster trust and comfort, the same anesthesia and surgical teams were assigned to the patient. Before the procedure, the patient was fully informed about the nature of the procedure and the possibility of a failed outcome or further need for a conversion to general anesthesia. To assess the patient's cognitive and language abilities, pre-agreed questions and exercises were performed. These included memory-related queries, such as asking for the patient's phone number and the names of her dog, and motor commands, such as squeezing a squeaky toy. The patient was prepared for awake navigator-assisted left frontal craniotomy for excision of the left frontal lobe space-occupying lesion which was suspected to be either a low-grade glioma or fibrous dysplasia.During the surgical procedure, a central line was placed in the right jugular vein using ultrasound, followed by the insertion of a right radial arterial line, a urinary catheter, and two additional venous lines. The patient received a continuous flow of 4-6 liters of oxygen per minute. To achieve conscious sedation, the patient received infusions of Remifentanil and Propofol at varying rates.
Table 1: Contraindications of AC
| Absolute |
| Patient refusal |
| Inability to lay still for any length of time |
| Inability to co-operate (ex. Confusion) |
| Relative |
| Patient cough |
| Learning difficulties |
| Inability to lay flat |
| Patient anxiety |
| Language barriers |
| Obstructive sleep apnoea |
| Young age |
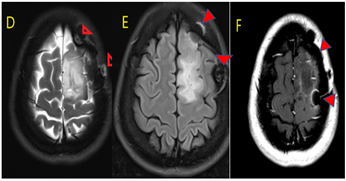
The patient underwent a 5-hour surgical procedure to remove a tumor. During the procedure, the patient was under sedation and regularly tested for response to predetermined commands. Her conscious sedation level fluctuated but she never lost consciousness. The removal of the tumor was successful, and postoperative examination revealed normal motor function and cranial nerve function. The patient was taken to the Intensive Care Unit (ICU) with instructions to keep her head elevated at 45 degrees. A postoperative CT scan showed the resolution of any post-surgery haemorrhaging and a decrease in surrounding edema. A postoperative MRI showed persistent changes such as a craniotomy scar. However, there was a reduction in the size of the mass lesion in the left frontal lobe/superior frontal gyrus, along with mild vasogenic edema surrounding it.
Figure 3: MRI brain with contrast [figure (D) T2, figure (E) FLAIR and figure (F) T1 post contrast].
Status post-op for left frontal cortical / subcortical lesion. In comparison to the fore mentioned study; Still noted postoperative changes in the form of craniotomy [red arrowhead] Noted regression of size of space occupying cortical mass lesion with mild surrounding vasogenic edema in the left frontal lobe/superior frontal gyrus.
Discussion
Awake craniotomy (AC) has been focused on the identification and excision of any intra-axial lesions that are encroaching upon eloquent cortical areas of the brain that play a crucial role in motor, linguistic, and cognitive functions [11,12]. Therefore, it is imperative to preserve these areas in order to maintain the optimum quality of life of the patient. Prior to performing Awake craniotomy (AC), it is crucial that a thorough evaluation of absolute and relative contraindications should be considered (Table 1).
Communication between all stakeholders involved in the procedure is of paramount importance for the success of the AC procedure [13]. In the current study, we kept the same anaesthesia staff and other staff to ensure optimum communication and trust levels between stakeholders. Clear communication with the patient is crucial for a successful procedure and any impediments that emerge in this relationship can affect the outcome of the procedure [14]. Generally, it includes conditions such as decreased awareness, difficulties with speaking, and confusion. Furthermore, several other factors can influence the outcome of the procedure and increase the risk of complications, such as obesity or large tumours that affect blood flow and prolong the operative time [15]. These risks should be evaluated before the procedure, and the patient should be counselled about the risks. To reduce the risk of confusion during the procedure, pre-operative agreements on questions and commands can be made to ensure clear communication [16].
Various anaesthetic techniques are employed in AC procedures to facilitate efficient tumour excision and protection of the functional cortex. Two commonly used methods are the "Asleep-Awake-Asleep" (AAA) technique and Monitored Anaesthesia Care (MAC) or conscious sedation [17]. However, in our case, a different approach was selected, consisting of a combination of Local Anaesthesia (LA) and conscious sedation, thereby realizing an "Awake-Awake-Awake" technique. Before undergoing the surgical procedure, the administration of local anaesthetic (LA) is performed through scalp blockade, utilizing a combination of bupivacaine and epinephrine for its analgesic properties. The targeted nerve fibres in the scalp region encompass the auriculotemporal, zygomaticotemporal, supraorbital, supratrochlear, and lesser and greater occipital nerves [18]. In our case, conscious sedation was achieved by infusion of Remifentanil and Propofol at varying rates. The most commonly utilized anaesthetic regimen for conscious sedation during surgery involves the systemic administration of propofol in conjunction with short-acting opioids such as fentanyl or remifentanil [19]. This regimen may be administered through continuous infusion, intermittent bolus, or through target-controlled infusion methods. To ensure optimum autonomic respiration, a non-invasive oxygen facial mask is utilized, however, it is crucial to continuously monitor the patient's respirational frequency and the levels of carbon dioxide expired, as some individuals with inherent susceptibilities may experience obstructive apnea [20].
Conclusion
The increased utilization of awake craniotomy has been a persistent endeavor for a century. Despite its associated challenges and complexities, it is frequently employed in tumor excision in eloquent cortical areas with great success. The pivotal role of the anesthesiologist in this regard cannot be overemphasized, as they are responsible for evaluating and mitigating any risk factors that may influence the procedure and determining the most suitable sedation regimen for each individual patient. Adequate preoperative counseling with the patient, continuous monitoring during the procedure, and contingency preparation for any possible complications are keys to ensuring a favorable outcome. Our case report illustrates the utilization of a combination of Local/regional anesthesia and sedation as the optimal option for a successful outcome in awake craniotomy.
Ethics Statement and Conflict of Interest Disclosure
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJ uniform disclosure form. all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Kulikov A, Lubnin A. (2018). Anesthesia for awake craniotomy. Current Opinion in Anesthesiology, 31:506-510.
Publisher | Google Scholor - Saito T, Tamura M, Chernov MF, Ikuta S, Muragaki Y, Maruyama T. (2018). Neurophysiological monitoring and awake craniotomy for resection of intracranial gliomas. Intracranial Gliomas Part I-Surgery, 30:117-158.
Publisher | Google Scholor - Eseonu CI, Rincon-Torroella J, ReFaey K, et al. (2017). Awake craniotomy vs craniotomy under general anesthesia for perirolandic gliomas: evaluating perioperative complications and extent of resection. Neurosurgery, 81:481-489.
Publisher | Google Scholor - Nakul E, Lopez C. (2017). Commentary: Out-of-body experience during awake craniotomy. Frontiers in Human Neuroscience., 11:417.
Publisher | Google Scholor - Chan DYC, Chan DTM, Zhu CXL, et al. (2018). Awake craniotomy for excision of arteriovenous malformations? A qualitative comparison study with stereotactic radiosurgery. Journal of Clinical Neuroscience, 51:52-56.
Publisher | Google Scholor - Zhang JJ, Lee KS, Voisin MR, Hervey-Jumper SL, Berger MS, Zadeh G. (2020). Awake craniotomy for resection of supratentorial glioblastoma: a systematic review and meta-analysis. Neuro-oncology advances, 111.
Publisher | Google Scholor - Motomura K, Natsume A, Iijima K, et al. (2017). Surgical benefits of combined awake craniotomy and intraoperative magnetic resonance imaging for gliomas associated with eloquent areas. Journal of neurosurgery, 127:790-797.
Publisher | Google Scholor - Sewell D, Smith M. (2019). Awake craniotomy: anesthetic considerations based on outcome evidence. Current Opinion in Anesthesiology, 32:546-552.
Publisher | Google Scholor - Kim SH, Choi SH. (2020). Anesthetic considerations for awake craniotomy. Anesthesia and Pain Medicine, 15:269-274.
Publisher | Google Scholor - Khu KJO, Pascual JSG, Ignacio KHD. (2022). Patient-reported intraoperative experiences during awake craniotomy for brain tumors: a scoping review. Neurosurgical Review, 45:3093-3107.
Publisher | Google Scholor - Kaye B, Correa Bastianon Santiago RA, MacKinnon G, et al. (2022). Wide Dissection Trans-Sulcal Approach for Resection of Deep Intra-Axial Lesions in Eloquent Brain Areas. Current Oncology, 29:7396-7410.
Publisher | Google Scholor - de Macêdo Filho LJ, Aguiar GC, Pessoa FC, et al. (2020). Intraparenchymal epidermoid cyst close to Broca area—awake craniotomy and gross total resection. World Neurosurgery, 141:367-372.
Publisher | Google Scholor - Kuribara T, Akiyama Y, Mikami T, et al. (2020). Preoperative prediction of communication difficulties during awake craniotomy in glioma patients: a retrospective evaluation of 136 cases at a single institution. Neurologia medico-chirurgica, 61:21-32.
Publisher | Google Scholor - Eseonu CI, ReFaey K, Garcia O, John A, Quiñones-Hinojosa A, Tripathi P. (2017). Awake craniotomy anesthesia: a comparison of the monitored anesthesia care and asleep-awake-asleep techniques. World neurosurgery, 104:679-686.
Publisher | Google Scholor - Lee CZ, Poon CCM. (2022). An Update of Neuroanesthesia for Intraoperative Brain Mapping Craniotomy. Neurosurgery, 90:1-6.
Publisher | Google Scholor - O'neill M, Henderson M, Duffy OM, Kernohan WG. (2020). The emerging contribution of speech and language therapists in awake craniotomy: a national survey of their roles, practices and perceptions. International Journal of Language & Communication Disorders, 55:149-162.
Publisher | Google Scholor - Natalini D, Ganau M, Rosenkranz R, et al. (2022). Comparison of the asleep-awake-asleep technique and monitored anesthesia care during awake craniotomy: a systematic review and meta-analysis. Journal of neurosurgical anesthesiology, 34:e1-e13.
Publisher | Google Scholor - Meng L, McDonagh DL, Berger MS. (2017). Anesthesia for awake craniotomy: a how-to guide for the occasional practitioner. Canadian Journal of Anesthesia, 64:517.
Publisher | Google Scholor - Manninen PH, Balki M, Lukitto K, Bernstein M. (2006). Patient satisfaction with awake craniotomy for tumor surgery: a comparison of remifentanil and fentanyl in conjunction with propofol. Anesthesia & Analgesia, 102:237-242.
Publisher | Google Scholor - Prontera A, Baroni S, Marudi A, et al. (2017). Awake craniotomy anesthetic management using dexmedetomidine, propofol, and remifentanil. Drug Design, Development and Therapy, 593-598.
Publisher | Google Scholor