Case Report
Uterine Torsion Noted After Fetal Delivery: A Case Report
- Adane Girma Alebachew 1
- Misganaw Abere Worku 1*
- Salh Yalew Mustofa 2
- Eyasu Feleke Yitina 1
- Nigat Amsalu Addis 1
1Department of Obstetrics and Gynecology, College of Medicine and Health Sciences, University of Gondar, Ethiopia.
2Department of Anesthesia, College of Medicine and Health Sciences, University of Gondar, Ethiopia.
*Corresponding Author: Nigat Amsalu Addis, Department of Obstetrics and Gynecology, College of Medicine and Health Sciences, University of Gondar, Ethiopia.
Citation: Adane G. Alebachew, Misganaw A. Worku, Salh Y. Mustofa, Eyasu F. Yitina, Nigat A. Addis. (2024). Uterine Torsion Noted After Fetal Delivery: A Case Report, Clinical Obstetrics and Gynecology Research, BioRes Scientia Publishers. 3(2):1-6. DOI: 10.59657/2992-9725.brs.24.016
Copyright: © 2024 Nigat Amsalu Addis, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 16, 2024 | Accepted: June 28, 2024 | Published: July 06, 2024
Abstract
Introduction: Rotation of the uterus less than 45 degrees along its longitudinal axis is considered physiological. Because of its rare occurrence, and not all cases worldwide have been reported, the prevalence of uterine torsion is not exactly known, and preoperative diagnosis is challenging. The mechanism of uterine torsion remains unknown.
Case Presentation: Our patient, a 28 years old Gravida-II Abortion-I mother presented with Prelabor rupture of the membrane which was prolonged, and labor induction was started. Non-reassuring fetal heart rate pattern with absent beat-to-beat variability and recurrent variable deceleration was detected 2 hours after labor induction, for which cesarean delivery was recommended. Through infra-umbilical midline skin incision and inadvertent posterior hysterotomy, a 3700g live male neonate with APGAR scores of 9 and 10 in the 1 and 5 minutes respectively, was affected within 30 minutes of decision. After the uterus was exteriorized and detorssed, the cavity was cleaned, repaired in two layers, and hemostasis was secured. The mother required three units of blood transfusion and was discharged on the 5 postoperative days with smooth maternal and neonatal conditions.
Conclusion: Uterine torsion is a rare phenomenon that requires a high index of suspicion, even in the presence of acute symptoms. The identified risk factor in our case was a large Uterine fibroid. In our case, the temporal occurrence of uterine torsion couldn’t be defined as she was diagnosed as having a sub serous myoma since 1st trimester of gestation and had no acute symptoms during the time of admission.
Keywords: uterine torsion; uterine fibroids; full term pregnancy; inadvertent posterior hysterotomy
Introduction
Uterine Torsion is the rotation of the uterus beyond 45 degrees along its longitudinal axis at the junction of the uterine corpus, and the cervix is rarely observed in obstetric practice. Most cases of pathological uterine torsion occur at approximately 180 degrees. It is considered physiological if the rotation is less than 45 degrees. The most common symptoms of uterine torsion are abdominal pain [1-8], fetal heart rate abnormality [3-7,9], and poor labor progress [3]. Uterine torsion is a rare but dangerous obstetric complication in both the fetus and the mother. Acute uterine torsion can lead to placental abruption [7,9,10], severe hemorrhage [2,6], maternal death [11], and intrauterine fetal death [4,11]. Uterine torsion can also lead to incarceration if it remains unrecognized [12]. In extremely rare cases, uterine torsion with a higher degree of rotation may be accompanied by bladder torsion [6]. This report describes the risk factors, clinical presentation, and management of uterine torsion during full-term pregnancy.
Case Presentation
A 28 years old Gravida-II Abortion-I mother Admitted to LW with the diagnosis of Full-Term Pregnancy + Term Prelabor Rupture of Membrane + Intramural myoma. The gestational Age from Reliable date is 40w 5d, and from 7w 3d, early Obstetrics ultrasound is calculated to be 40w 3d. She was given a written ultrasound report at 7w 3d gestational age, which mentions the presence of multiple myoma, the largest measuring 10cm x 8cm. She was screened for HIV and syphilis, and the results were negative. Her blood group was B-positive, and antenatal HCT was 34.4% (Hemoglobin=11.8 g/dl). She had five ANC contacts and a smooth antepartum condition. One year prior to conception of the current pregnancy, she had a spontaneous complete abortion and a smooth post-abortal condition.
She initially presented to a labor triage with the complaint of leakage of liquor of 2 hours duration but no fever, pushing down pain, foul-smelling vaginal discharge, vaginal bleeding, or abdominal pain. On admission, the patient was comfortable, hemodynamically stable, and afebrile. Examination revealed a term-sized gravid uterus, longitudinal lie, cephalic presentation, no contraction, or uterine tenderness. The fetal heartbeat was 146 beats per minute. There was an ill-defined, non-tender mass on the right hypochondrium posterior to the uterine fundus. Pelvic Examination showed Liquor-wetted vulva, cervix was closed, uneffaced, and a high station with a ruptured and clear membrane.
Obstetrics Ultrasound examination at admission showed: Singleton Intrauterine pregnancy with Cephalic presentation, Fetal Heart beat positive (146BPM), Estimated Fetal Weight 3600 grams, average gestational age 39w 1d; Gross Body Movement, Breathing Movement and fetal tone seen, placenta was Fundal anterior and no gross fetal congenital anomaly seen. There was a relatively hypoechoic well delineated mass measuring 18cm x 12cm on the posterior fundal part of the uterus.
The patient was admitted to LW for follow up and cross-matched blood preparation made. After an overall 12h with Rupture of Membrane, GBS prophylaxis was started, and labor induction was decided and started with 5 IU oxytocin titrated with 1litre of Normal saline. After 2 hours of labor induction, cervix was dilated by 2cm, effaced at 60%, and station-2, grade II meconium-stained amniotic fluid, and fetal Heart Rate on Cardiotocography showed non-reassuring tracing with absent beat-to-beat variability and recurrent variable deceleration for which emergency Cesarean Delivery was decided.
After informed written consent was obtained, the patient was taken to the OR and under the SA abdomen washed with alcohol and iodine tincture, and entered via infra-umbilical vertical skin incision, which was carried down through the subcutaneous tissue to the fascia. The fascia was opened vertically, approximately 2cm above the symphysis. Layers of the abdominal wall were opened with a combination of sharp and blunt dissection; a 3cm sharp incision was made over the lower uterine segment, which was extended bluntly and delivery of a 3700g male alive neonate with APGAR (Appearance, Pulse, Grimace, Activity, and Respiration) score of 9 and 10 in the 1 and 5 minutes respectively, effected within 30 minutes of decision.
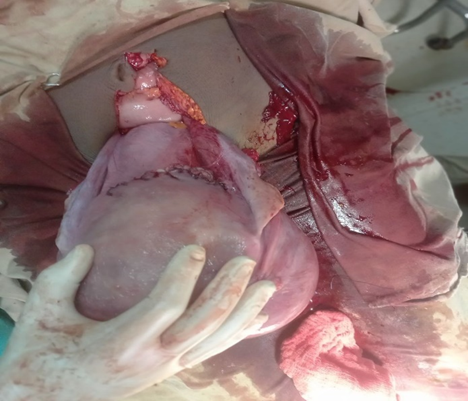
Intraoperatively, a grade-III meconium was noted on delivery, but no nuchal cord or retroplacental clot was observed. The umbilical cord was clamped and cut, oxytocin drip was initiated, and the placenta was delivered by controlled cord traction and complete. At the time of exteriorizing the uterus, it was noted that the uterus had undergone 180-degree torsion and dextro-rotated with the left adnexa well right of the midline, and there was a huge subserous myoma involving the anterior Lower Uterine Segment and anterior fundal uterine wall positioned directly posterior before detorsion, but no uterine anomalies, pelvic adhesion, or ovarian pathologies were seen. Both fallopian tubes and ovaries were healthy. It was surprising for the surgeon to notice uterine torsion after delivery of the neonate via inadvertent posterior hysterotomy (Figures 1-4).
Figure 1: Huge sub serous myoma visualized here after uterine exteriorization and detorsion.
Figure 2: A picture taken While mopping/cleaning the posterior cul-de-sac.
Figure 3: After Hemostasis secured and Cul-de-sac cleaned.
Figure 4:Repaired posterior transverse lower uterine segment incision seen with umbilicus seen in the cephalad direction.
After uterus exteriorized and detorssed, uterine cavity cleaned with sterile pack, edges grasped with green Armitage, repaired in two layers and Hemostasis secured. Cul-de-sac and paracolic gutters cleaned with sterile pack, uterus replaced back, Instrument count checked and declared correct. Peripartum myomectomy was abandoned due to the possibility of increased blood. Abdomen closed layer by layer and patient left the Operation Room with stable vital signs. Intraoperative Estimated Blood Loss was 1200ml. The neonate was bonded to the mother for breast feeding. She was put on Maintenance Fluid and Oxytocin drip 40iu in 1litre of Normal Saline for the first 6 hours after delivery. Post operatively her Hematocrit was 26.6% (Hgb=9.3g/dl) for which she was transfused with three units of compatible whole blood and hematocrit after transfusion become 38.3% (Hgb 12.5g/dl), SGOT 31.5u/L, SGPT=17.3u/L, Urea=12.3mg/dl and Creatinine=0.45mg/dl. Subsequently both the mother and the baby were doing fine and discharged improved from the hospital on the 5th postoperative date and she was linked to Postpartum follow up clinic and Gynecologic OPD. She had one visit at postnatal clinic at the 6-week following delivery, but she didn’t appear at Gynecologic OPD later on. Upon phone communication which was registered on her card revealed that she was moved to another nation 9 months after delivery.
Discussion
Pathological uterine torsion occurs when the uterus rotated more than 45 degrees along its longest axis at the level of cervical-isthmic junction. Uterine torsion occurs in the nongravid uterus and in any month of gestation. It is difficult to know the actual epidemiology of this obstetric emergency due to its rare occurrence. To date, there is no known association between torsion and maternal age, parity or gestational age [6]. In fact, there is no proven mechanism responsible for the development of pathological uterine torsion. Based on available literature review, the most important risk factors are Abnormal fetal presentations [1,6] uterine fibroids [3] Connective tissue disorder [4] Polyhydramnios [6] Ovarian cyst or other adnexal mass [8] Mullerian anomalies [5,11,13] Retroverted uterus [12] and Pelvic adhesions [14]. In our case; Uterine fibroid might be risk factor for uterine torsion though the temporal occurrence cannot be defined as she was diagnosed to have intramural myoma since 1st trimester gestation.
Clinical presentation of a woman with uterine torsion may be variable. It can be asymptomatic [10,12,14,15], poor progress of labor and/or non- reassuring fetal heart rate pattern [6,13,16] or with different extent of abdominal pain and shock [2-4,8,9]. In our case possibility of fetal distress was considered due to the presence of non-reassuring fetal heart rate pattern and grade-II meconium-stained amniotic fluid. Ultrasound may be helpful in the diagnosis of uterine torsion if the placental location is known prior to clinical presentation. A Change in the localization of placenta, abnormal localization of the ovary, and loss of flow in the uterine artery dopplers can potentially be detected during ultrasound scanning [17]. The x-shaped configuration on the bladder may be indicated on MRI in asymptomatic cases where urgent intervention is not required [18]. Our case is diagnosed intraoperative as in most cases reported in the literature.
If known initially with preoperative or intraoperative diagnosis just before hysterotomy incision; It is quite prudent to determine the degree of torsion to avoid bladder and ureter injury at the back of the uterus during operations where detorsion cannot safely be performed. In such cases, delivery can be affected in three ways: vertical uterine fundal incision, posterior uterine wall incision or high transverse incision on the anterior wall of the uterus while observing and protecting the bladder plication [19]. Uterine torsion can be a surprise finding for the surgeons noted first even after delivery of the baby with in advertent posterior hysterotomy [2,3]. In our case uterine torsion was noticed after in advertent posterior lower uterine segment incision and delivery of the neonate.
The long-term implication of delivery after uterine torsion is not known [2]. It is recommended to do round ligament plication in the early postpartum period [20] and uterosacral ligament plication in the late postpartum period [21] to reduce the recurrence rate of uterine torsion. In our case due to consideration of late postpartum myomectomy and plication of uterosacral ligament, we didn’t do during cesarean delivery and patient had no early post-partum complications.
Conclusion
It is extremely difficult to diagnose uterine torsion preoperatively due to varied clinical presentation and its rare occurrence. However, it is quite prudent to consider uterine torsion as one of the differential diagnoses in cases presented with acute abdominal pain. It’s important to determine the degree of torsion before uterine incision in order to avoid potential complications. Clinical diagnosis of uterine torsion was difficult in our case as she presented with rupture of membrane subsequently labor induction started followed by Cesarean section performed for the obvious indication of non-reassuring fetal heart rate pattern. In our case; the temporal occurrence of uterine torsion cannot be defined as she was diagnosed to have intramural myoma since 1st trimester gestation.
Abbreviations
ANC: Antenatal care
APGAR: Appearance, Pulse, Grimace, Activity and Respiration
BPM: Beats per minute
CARE: Case Report
GBS: Group B streptococcus
HCT: Hematocrit
IU: International units
MRI: Magnetic Resonance Imaging
OPD: Outpatient Department
Declarations
Ethical Approval
Draft of this case report has been submitted to the School of Medicine at University of Gondar for Ethical Board Review and approved as ethically sound report.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflict of Interest Statement
All Authors of this manuscript declared there is no conflict of interest.
Consent for Publication
Written informed consent was taken from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review for the editor-in-chief of this journal.
Author Contributions
All authors contributed to the conception, writing and editing of the case report. All authors are agreed to be accountable for all aspects of work.
Funding
No funding was received for this research.
Acknowledgments
Not applicable.
References
- Bui TTK, Le TV, Nguyen OTK, Tran HTB, Nguyen TDP. (2024). Uterine Torsion in Pregnancy: A Case Report. Int J Surg Case Rep. 116:109441.
Publisher | Google Scholor - Fatih FF, Gowri V, Rao K. (2012). Uterine Torsion in Second Trimester of Pregnancy Followed by A Successful-Term Pregnancy. BMJ Case Rep.
Publisher | Google Scholor - Yin FL, Huang HX, Zhang M, Xia XK, Xu H, et al. (2020). Clinical Analysis of Uterine Torsion and Fibroids in Full-Term Pregnancy: A Case Report and Review of The Literature. J Int Med Res. 48(6).
Publisher | Google Scholor - Ghalandarpoor-Attar SN, Ghalandarpoor-Attar SM. (2022). Uterine Torsion as An Elusive Obstetrical Emergency in Pregnancy: Is There an Association Between Gravid Uterus Torsion and Ehlers-Danlos Syndrome? A Case Report. J Med Case Rep. 16(1):210.
Publisher | Google Scholor - Ghosh MD, Singh V, Datta MR. (2022). Torsion of Uterus Didelphys at Term: Once-In-A-Lifetime Experience for An Obstetrician. Cureus. 14(11):31996.
Publisher | Google Scholor - Kilicci C, Sanverdi I, Bostanci E, Abide CY, Eser SK. (2018). Uterine Torsion Of 720 Degrees in The Third Trimester of Pregnancy and Accompanying Bladder Torsion: A Case Report. Pan Afr Med J. 29:175.
Publisher | Google Scholor - Liu S, Zhou L, Song B, Liu D, Zheng C, et al. (2023). Uterine Torsion Complicated by Severe Placental Abruption in The Second Trimester: A Case Report and Literature Review. BMC Pregnancy Childbirth. 23(1):51.
Publisher | Google Scholor - Moores KL, Wood MG, Foon RP. (2014). A Rare Obstetric Emergency: Acute Uterine Torsion in A 32-Week Pregnancy. BMJ Case Rep.
Publisher | Google Scholor - Ulu I, Gunes MS, Kiran G, Gulsen MS. (2016). A Rare Cause of Placental Abruption: Uterine Torsion. J Clin Diagn Res. 10(1):6-7.
Publisher | Google Scholor - Cook KE, Jenkins SM. (2005). Pathologic Uterine Torsion Associated with Placental Abruption, Maternal Shock, And Intrauterine Fetal Demise. Am J Obstet Gynecol. 192(6):2082-2083.
Publisher | Google Scholor - Wang B, Zhou JH, Jin HM. (2011). Torsion of A Rudimentary Uterine Horn At 22 Weeks of Gestation. J Obstet Gynaecol Res. 37(7):919-920.
Publisher | Google Scholor - Kocher M, Hirsig L. (2020). A Case of Uterine Incarceration with Unrecognized Uterine Torsion. Radiol Case Rep. 15(10):1943-1947.
Publisher | Google Scholor - Gao Q, Xiong J, Zhu Y. (2023). Uterine Torsion in Twin Pregnancy with Complete Bicorporeal Uterus, Double Cervix, Longitudinal Non-Obstructing Vaginal Septum - A Case Report. Front Surg. 10:1082955.
Publisher | Google Scholor - Kim S, Bae HJ, Lee EJ, Kwak DW, Yang J. (2024). A Case Report of Torsion of The Gravid Uterus Caused by Pelvic Adhesion. Clin Case Rep. 12(1):8384.
Publisher | Google Scholor - Boogaerts M, Wuyts K, Joos H. (2022). Two Successive Cesarean Deliveries Through Separate Posterior and Anterior Hysterotomy Due to Asymptomatic Uterine Torsion. A Case Report. Case Rep Womens Health. 36:00435.
Publisher | Google Scholor - Huynh K, Andersen H. (2021). Uterine Torsion in A Full-Term Pregnancy Presenting as Prolonged Latent Phase and Fetal Intolerance of Labor: A Case Report. Case Rep Womens Health. 32:00353.
Publisher | Google Scholor - Kremer J, Van Dongen P. (1989). Torsion of The Pregnant Uterus with A Change in Placental Localization on Ultrasound; A Case Report. European Journal of Obstetrics & Gynecology and Reproductive Biology. 31(3):273-275.
Publisher | Google Scholor - Nicholson WK, Coulson CC, McCoy MC, Semelka RC. (1995). Pelvic Magnetic Resonance Imaging in The Evaluation of Uterine Torsion. Obstetrics & Gynecology. 85(5):888-890.
Publisher | Google Scholor - Karavani G, Picard R, Elami-Suzin M, Mankuta D. (2017). Complete Uterine Torsion Diagnosed During an Elective Caesarean Section Following Failed External Cephalic Version: A Case Report. Journal of Obstetrics and Gynaecology. 37(5):673-674.
Publisher | Google Scholor - Pelosi 3rd M, Pelosi M. (1998). Managing Extreme Uterine Torsion at Term. A Case Report. The Journal of Reproductive Medicine. 43(2):153-157.
Publisher | Google Scholor - Mustafa M, Shakeel F, Sporrong B. (1999). Extreme Torsion of The Pregnant Uterus. Australian and New Zealand Journal of Obstetrics and Gynaecology. 39(3):360-363.
Publisher | Google Scholor