Review Article
Update on the Therapeutic Management of Acute Achilles Tendon Rupture with Surgical Versus Conservative Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Bianca Gabriella de Oliveira 1*
- Maria Luíza Costa Severo 2
- Guilherme de Brito Lira Del Monte 3
- Túlio de Almeida Estevão 3
- Caio Lucas Agra de Medeiros 3
- Laís Cristina Pereira da Silva 4
1Medical student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil.
2Medical resident in Orthopedics and Traumatology at Centro Universitário UNIFACISA, Campina Grande, PB.
3Resident in Orthopedics and Traumatology, UNIFACISA University Center, Campina Grande, PB.
4Medical student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil.
*Corresponding Author: Bianca Gabriella de Oliveira, Medical student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil.
Citation: Bianca G. Oliveira, M.L.C. Severo, G.B.L.D. Monte, Túlio A. Estevão, C.L.A. Medeiros, et al. (2024). Update on the Therapeutic Management of Acute Achilles Tendon Rupture with Surgical Versus Conservative Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, Clinical Interventions and Clinical Trials, BioRes Scientia Publishers. 2(2):1-8. DOI: 10.59657/2993-1096.brs.24.022
Copyright: © 2024 Bianca Gabriella de Oliveira, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 24, 2024 | Accepted: March 11, 2024 | Published: March 16, 2024
Abstract
Objective: The aim of this study is to compare the current clinical results of surgical treatment versus conservative management of acute Achilles tendon rupture.
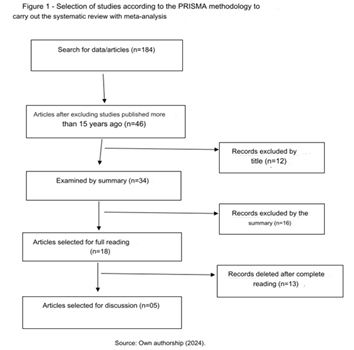
Methodology: This is a systematic review of the literature, structured according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and a PRISMA checklist was subsequently structured to analyze the results.5 A four-phase flow diagram was also used in order to achieve clarity and transparency in execution. Register with prospero under ID CRD42024512029.
Results: The data search started with 184 articles, 138 were eliminated because they had been published for more than 15 years, leaving 46. After evaluating the titles and abstracts, there were 18 articles that corresponded to the study proposal, which were read in full and 13 were eliminated. Finally, 5 articles were selected for analysis and construction of the study. The Achilles Tendon Total Rupture Score (ATRS) is a patient-reported assessment for analyzing the treatment of acute Achilles tendon rupture. The questionnaire consists of 10 questions that assess symptoms and the degree of physical activity performed by the patient. The studies that used this outcome indicated better results for those who underwent surgical treatment rather than non-operative treatment.
Conclusion: It can be concluded that it is still controversial and there is no agreement on which therapeutic approach should be indicated. However, it should be noted that "mini-open" techniques are interesting, as they reduce damage to the soft tissues, deliver a firm and solid repair, enabling functional gain and fewer surgical complications. It should be noted that assistance in post-operative recovery is essential for better functional results and, consequently, greater patient satisfaction.
Keywords: therapeutic management; acute achilles; tendon rupture; surgical versus; conservative management; meta-analysis; randomized controlled trials
Introduction
The Achilles tendon or calcaneal tendon plays a role in body biomechanics, allowing the superficial posterior muscles of the leg to flex the foot and stabilize the ankle joint during the gait cycle. It originates at the distal end of the gastrocnemius muscle and inserts into the posterior surface of the calcaneus. it is innervated by the sural nerve. It is vascularized in its proximal and distal thirds by the posterior tibial artery, while its middle third is vascularized by the fibular artery [1]. The spiral path of the fibers just before their insertion creates an area of concentrated tension transmitted to the calcaneus, thus causing adequate force to be transmitted to the foot during walking, running or jumping. This is the main mechanism of trauma to the anatomical structure in question [2]. Due to its important epidemiology with evidence of high prevalence, it is the most frequently ruptured tendon in the human body, with an annual incidence of 18 per 100,000 people. Constant updates in therapeutic management are necessary in order to reduce sequelae [3].
It has an incidence of 31 per 100,000 per year, and is more common in the young and middle-aged working population, with an average age of between 37 and 44 years [4]. Recent studies indicate that the incidence of tendon rupture will continue to be high due to the more active elderly population [5]. It is one of the most common disabling injuries in the male population, occurring mainly in active individuals who play high-impact sports, especially ball games [6,7]. Some studies suggest that multiple risk factors are correlated with Achilles tendon rupture, involving poor vascularization of the tendon, its degeneration, the use of corticosteroids, previous rupture on the contralateral side and the use of fluoroquinolones [8]. Patients with a rupture of this tendon report pain in the affected leg and the sensation of being hit in the back of the leg, or a clicking sensation in the heel [9]. On clinical examination, there is usually a hematoma and diffuse edema, and a gap is usually palpable along the tendon, most often 2 to 6 cm near its insertion [10]. Inspection and palpation are followed, weakness in plantar flexion of the ankle and a positive Thompson test are observed [11]. With regard to the use of a complete examination, ultrasound (USG) is the first examination required when there is a need for confirmation through imaging [12]. USG can help in the choice of treatment; one study showed that gaps > 10mm at the first examination increased the risk of re-rupture among patients treated conservatively (non-surgically); those with gaps > 5mm who opted for non-invasive therapy had worse functional results at the end of 12 months [13].
When additional alterations are identified on physical examination, magnetic resonance imaging (MRI) may be indicated to better assess the type of rupture, since longitudinal and oblique lesions require greater surgical planning 12 and also in cases of acute dislocation of the posterior tibial tendon at the same time as rupture of the Achilles tendon [14]. However, it is recommended to rely on the physical examination and clinical assessment, and to apply imaging to exclude other possible injuries [15]. When surgery is advised, it can be performed within one or two weeks of the injury, allowing the increased volume to be absorbed and facilitating the positioning of the suture knots. During this period, patients can be immobilized in slight equinus, with or without load on the limb, and elevation should be indicated. In cases where the support is released, a long orthopedic boot with heels on the hindfoot should be used [12]. The literature indicates that surgical treatment can effectively reduce the re-rupture rate and may be a better choice for the treatment of acute Achilles tendon rupture, however, the ideal intervention for acute Achilles tendon rupture remains controversial [4]. It is possible to point to at least a 10% functional deficit with its non-surgical method. The aim of this study is to compare the clinical results of surgical treatment versus conservative management of acute Achilles tendon rupture.
Methodology
This is a systematic literature review study, structured in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and a PRISMA checklist was subsequently structured to analyze the results [5]. A four-phase flow diagram was also used to achieve clarity and transparency in the execution. Registered in prospero under ID CRD42024512029.
The descriptors in health sciences (DECS)/MESH TERMS were used in combination, according to the following structures: Calcaneal tendon OR Achilles tendon AND Rupture OR orthopaedic procedures.
The data search took place on October 5, 2023, in the databases linked to the Medical Literature Analysis and Retrieval System Online (MEDLINE), using the Setting, Perspective, Intervention, Comparison, and Evaluation (SPICE) strategy to identify the relevant studies:
- Setting: hospitalized patients
- Perspective: individuals with acute Achilles tendon rupture
- Intervention: Achilles tendon rupture repair surgery
- Comparison: clinical outcome of conservative versus surgical treatment of acute Achilles tendon rupture
- Evaluation: effectiveness of treatment methods
Inclusion and exclusion criteria
Studies that met the following criteria were included: [1] studies with humans, age group > 18 years [2] patients undergoing surgical treatment for acute Achilles tendon rupture [3] studies dealing with patients with acute Achilles tendon rupture injury [4] studies published between 2008-2023 [5] original studies.
Studies with the following criteria were excluded: [1] experimental studies with animal models [2] non-original studies - literature review [3] opinion studies [4] studies published more than 15 years ago [5] studies that did not meet the other inclusion criteria mentioned above.
The search and selection of studies was carried out by three reviewers who independently analyzed the studies. Initially, using the DECS mentioned, together with Boolean operators, studies published in the last 15 years (2008-2023) were selected, followed by an analysis of titles and abstracts. At this stage, studies using animal models, opinion articles and literature reviews were excluded. Once this stage was completed, the full texts of the articles were retrieved to analyze the other inclusion and exclusion criteria. Duplicate citations and studies not corresponding to the proposed review parameters were also excluded. Possible disagreements were resolved through discussion with a third reviewer, and inclusion was decided after consensus with the two main reviewers. In order to prioritize methodological quality, studies classified as "Good" were included after evaluation.
Results
Initially, the data search began with 184 articles, 138 of which were eliminated because they had been published for more than 15 years, leaving 46. After evaluating the titles and abstracts, there were 18 that corresponded to the proposal of the study, which were read in full and 13 were eliminated. Finally, 5 articles were selected for analysis and construction of the study (Figure 1).
Figure 1: Selection of studies according to the PRISMA methodology to carry out the systematic review with meta-analysis.
Table 1 shows the studies selected for analysis and their respective outcomes. [16,17,18,19,20].
Table 1: Studies analyzed and their outcomes.
| Study | Approach | Patients F/M | Results |
| Myhrvold et al | Non-operative treatment Open repair Minimally invasive repair | 135/391 | Total Achilles tendon rupture score; Short Form Health Survey; physical performance; tendon rerupture. |
| Lantto et al | Non-operative treatment Open repair | 5/55 | Leppilahti Achilles tendon performance score, isokinetic calf muscle strength, and RAND 36-Item Health Survey; Tendon rerupture |
| Manent et al | Non-operative treatment Open repair Percutaneous repair | 3/31 | Total Achilles tendon rupture scale (ATRS); Victorian Institute of Sport Assessment (VISA); |
| Willits et al | Non-operative treatment Open repair | 26 / 118 | Rerupture rate; isokinetic strength, Leppilahti score, range of motion, and calf circumference |
| Kosiol et al | Non-operative treatment Open repair | 4/48 | Clinical analysis, ultrasound and magnetic resonance imaging. |
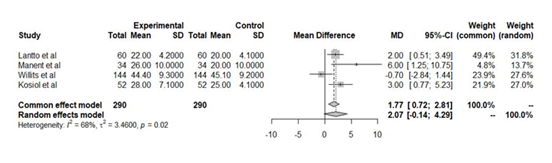
Table 2 shows the plantar flexion range of motion of patients who underwent surgical and non-surgical treatment for calcaneal tendon rupture [16,17,18,19,20].
Table 2: Range of movement of plantar flexion of patients undergoing surgical and non - surgical treatment to correct Achilles’ tendon rupture.
| Study | Sample | Age | Plantar flexion (º) non-operative group | Plantar flexion (th) operative group |
| Myhrvold et. al | 526 patients | 39.9 years | NR | NR |
| Lantto et al | 60 patients | 39.3 years | 22nd +- 4.2 | 20º+- 4.1 |
| Manent et al | 34 patients | 42 years | 26th +- 10 | 20º+- 10 |
| Willits et al | 144 patients | 40.2 years | 44.4° +- 9.3 | 45.1 +- 9.2 |
| Kosiol et al | 52 patients | 41 years | 28 +- 7.1 | 25 +- 4.1 |
Table 3 shows the numbers of calcaneal tendon re-ruptures in patients who underwent operative or non-operative treatment [16,17,18,19,20].
Table 3: Achilles tendon re-rupture numbers in patients undergoing operative or non -operative treatment .
| Study | Sample | Non-operative group | Operating group |
| Myhrvold et al | 526 patients | 11 | 2 |
| Lantto et al | 60 patients | 4 | 1 |
| Manent et al | 34 patients | 0 | 0 |
| Willits et al | 144 patients | 2 | 1 |
| Kosiol et al | 52 patients | 0 | 0 |
Figure 2 contains the forest plot for the meta-analysis of plantar flexion range of motion in patients undergoing treatment for Achilles tendon rupture.
Figure 2: Forest graph for meta-analysis of plantar flexion range of motion of patients undergoing treatment for Achilles tendon rupture.
Myhrvold et al. demonstrated in their study a total Achilles tendon rupture score (ATRS) for patients undergoing non-surgical treatment of 93.9 ± 15.1 and surgical treatment of 94.2 ± 12.9, representing mean changes of -17.0 points in the non-surgical group, -16.0 points in the open repair group and -14.7 points in the minimally invasive surgery group (P = 0.57). 256 of the 526 cases of calcaneal tendon ruptures were in the right tendon, there were 11 re-ruptures in the non-operative group (6.2% of patients), 1 in the open repair group (0.6%) and 1 in the minimally invasive surgery group (0.6%). With regard to the SF-36 (36-Item Short Form Health Survey) score, which assesses quality of life, there were no significant differences between the groups [16]. For Lantto et al, the Leppilahti score was used as a parameter to assess pain, stiffness, muscle weakness, footwear restriction in addition to ankle range of motion and muscle strength scores. Values of 79.5 +- 10 and 75.7 +- 11.2 were recorded for surgical and non-surgical patients, respectively. 04 re-ruptures occurred in the non-surgical group and 01 in the surgical group. Surgery was related to a better restoration of leg muscle strength and ankle joint range of motion, with a description of a 10% to 18% difference in strength between the study groups. In terms of range of movement, post-operative plantar flexion in the surgical group was 20º+- 4.1 versus 22º +- 4.2 for the non-surgical group [17].
Manent et al. also used the ATRS as a way of evaluating the patients, by analyzing the forest plot, the open surgery group showed a lower evolution in the questionnaires applied when compared to the conservative and percutaneous treatment groups. No serious adverse events were reported during follow-up and there were no cases of total rupture. Regarding the imaging evaluation, MRI was performed on 3 patients, 1 in each selected group, who reported pain 24 weeks after the injury. Partial micro-ruptures were identified at the level of the calcaneal tendon and at the musculotendinous junction [2]. patients reported hyperalgesia in the sural nerve territory, in the surgical groups, and there was no wound infection during follow-up. At 1-year follow-up, 5 patients (3 percutaneous surgeries and 2 open surgeries) had a fibrous and hardened scar. When assessing the amplitude of plantar flexion, the conservative treatment group obtained a result of 26° +- 10 in the injured limb; 20° +- 10 in the percutaneous surgery group; and 15° +- 10 in the open surgery group [18]. Willits et al presented a Leppilahti score of 78.5 ± 10.9 points in the operative group and 76.3 ± 15.8 points in the non-operative group (-2.2 points; 95% CI, -9.1 to 4.7 points; p = 0.53). When assessing range of motion, the mean dorsiflexion range was 16.4° ± 6.5° in the surgical group and 17.2° ± 7.8° in the non-surgical group. The mean plantar flexion range was 44.4° ± 9.3° versus 45.1° ± 9.2° for the non-operative group. There were 13 complications (18%) in the operative group and 6 (8%) in the non-operative group, with the main difference being the greater number of soft tissue-related complications in the operative group. With regard to re-ruptures, 02 occurred in the non-operative group and 01 in the operative group [19].
Kosiol et al used the ATRS with records of 78.7 +- 14.9 for the conservative group and 88.2 +- 8.3 for the surgical group. Deficits in dorsiflexion and plantar flexion of - 1.7 +- 7.1 in the conservative group and -3.7 +- 4.1 in the surgical group were recorded. There were no cases of re-ruptures. A comparison of all the injured tendons showed considerable lengthening and thickening of the tendon, regardless of whether the treatment was conservative or operative. When comparing the measurements taken in the conservative group and the operative group, the length of the Achilles tendon on the injured side was seen to increase by 50.9% at rest and by 44.4% under load. The diameter of the tendon on the injured side was increased to 113.0% at rest and to 124.5% under load [20].
Discussion
In fact, most of the individuals showed greater loss of plantar flexion when treated conservatively. 13 In addition, numerous studies have shown that non-surgical treatment is linked to high re-rupture rates and long periods of immobilization in plaster casts, which lead to stiff ankles and weak posterior leg muscles. 24 However, this difference does not interfere with their activities of daily living, especially in patients who are treated functionally and not as athletes [21,25,26]. The surgical approach, on the other hand, has been associated with a lower re-rupture rate. 13 Traditional open repair involves a 5 to 8 cm longitudinal posteromedial incision over the focus of the injury, with dissection of the paratendon, removal of the hematoma, debridement of the tendon stumps, and Krackon-type sutures to join the wires and coopt the stumps. Even though this repair technique is biomechanically strong and shows good results overall, it has been associated with a higher risk of other complications, including wound infection, scar adhesion, keloid formation, skin peeling, patient dissatisfaction with the scar and soft tissue injury [27,28,29].
In order to reduce these types of complications, some authors have suggested percutaneous techniques. Percutaneous repair is said to have a low complication rate and a high degree of satisfaction. The Achilles tendon is repaired percutaneously, and is less thick than that repaired with an open procedure, so it often has better aesthetic healing. However, some studies have observed a higher rate of re-rupture compared to the open approach, due to insufficient sutures without direct visual control. Furthermore, it is associated with iatrogenic injuries to the sural nerve caused by entrapment in the suture, with complaints of persistent paresthesia and, in some cases, the need for surgical exploration to remove the suture and free the nerve [27,28,29,30,31,32,33,34,35]. For this reason, minimally invasive tenorrhaphy has been indicated to improve these results. The aim is to reduce the skin and wound complications of open surgery, while guaranteeing the safety characteristics of the suture in terms of the re-rupture rate. Its main advantages are direct visualization of the lesion and less surgical invasion. In 1996, Assal developed a device suitable for the minimally invasive technique, called "Achillon", which is recommended when the subcutaneous rupture is more than 2 cm or less than 8 cm from the posterior calcaneal tuberosity and when the procedure is performed up to 10 days after the trauma. As already mentioned, the Achillon1 suture system has a low re-rupture rate and few soft tissue complications, less than those seen after open surgery. [27,28,29,30,31,32,33,34,35].
In the post-operative management of open surgery, a short-leg plaster cast is used without weight-bearing in gravitational equinus for four weeks after surgery. Serial casting is then started with a hinged brace to gradually adjust the ankle to 90 degrees until 8 weeks after the procedure. The patient is then allowed to bear weight in a functional position blocked by the cast or brace for 4 weeks. They are then finally allowed full, free weight-bearing with a 2.5cm heel up to six months after surgery. In the minimally invasive Achillon tenorrhaphy, a short leg cast is used without weight bearing in gravitational equinus for 20 days after surgery. This is followed by active mobilization without weight bearing, with gradual recovery of the functional position by the sixth week, after which loading is allowed with a splint locked at 90 degrees or a plaster cast until 60 days after the procedure. Subsequently, gradual full weight-bearing is resumed, with a 2.5cm jump up to 6 months post-operatively [27,28,29,30,31,32,33,34,35]. It is therefore up to the orthopaedic surgeon to decide which surgical technique should be used, based on their individual and personal analysis of each patient, their experience, knowledge and technical ability. However, consideration should be given to the growing scientific evidence that less invasive techniques may be superior to classical treatment. [35,36,37,38,39,40].
Open tenorrhaphy was performed using the typical Kessler suture method. The patient is positioned in the prone position with a tourniquet on the thigh. A 6-8cm long incision is made at the medial edge of the Achilles tendon. The subcutaneous tissue and fat are desiccated; this exposes the lesion. The ankle is then flexed plantarly to expose and hold the tendon stumps. Subsequent to the main suture with absorbable braided wires, the repair is completed by tubing with absorbable braided wires. This is followed by precise closure to reduce and avoid scar tissue adhesions. The skin is closed with a monofilament nylon suture [35,36,37,38,39,40]. In the Achillon group1, a medial longitudinal skin incision is made along the lesion and extended by 1.5 to 3cm. The subcutaneous tissue is dissected, the device is inserted and pushed proximally, with two internal arms below, surrounding the tendon stump. When the device reaches a safe area of the tendon, three sutures are inserted in succession, through the skin, the membrane and the tendon, via the holes in the device. The device is then extracted from the skin access, pulling the sutures into the tendon and then exiting the skin access at the site of the injury. The procedure is repeated on the distal stump, and then the tendon is sutured to the correct length under visual control. Finally, the skin incision is closed and sutured [35,36,37,38,39,40].
Conclusion
In conclusion, it is still controversial and there is no agreement on which therapeutic approach should be indicated. However, it should be noted that the "mini-open" techniques are interesting, as they reduce damage to the soft tissues, deliver a firm and solid repair, enabling functional gain and fewer surgical complications. It should be noted that assistance in post-operative recovery is essential for better functional results and, consequently, greater patient satisfaction.
References
- Sajko SS. (2006). Gray’s Anatomy for Student’s. J Can Chiropr Assoc, 50(4):290.
Publisher | Google Scholor - Yang X, Meng H, Quan Q, Peng J, Lu S. et.al. (2018). Management of acute Achilles tendon ruptures: A review. Bone Joint Res, 7(10):561-569.
Publisher | Google Scholor - Miller CP, Chiodo CP. (2017). Open Repair of Achilles Tendon Ruptures. Tech Foot Ankle Surg, 16:62-67
Publisher | Google Scholor - Deng S, Sun Z, Zhang C, Chen G, Li J. (2017). Surgical Treatment Versus Conservative Management for Acute Achilles Tendon Rupture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Foot Ankle Surg, 56(6):1236-1243.
Publisher | Google Scholor - Ganestam A, Kallemose T, Troelsen A, Barfod KW. (2016). Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc, 24:3730 -737.
Publisher | Google Scholor - Egger AC, Berkowitz MJ. (2017). Achilles tendon injuries.Curr Rev Musculoskelet Med. 10:72-80.
Publisher | Google Scholor - Gwynne-Jones DP, Sims M, Handcock D. (2011). Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int, 32:337-343.
Publisher | Google Scholor - Nyyssonen T, Luthje P, Kroger H. (2008). The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987-1999. Scand J Surg, 97:272-275.
Publisher | Google Scholor - Kraemer R, Wuerfel W, Lorenzen J, Busche M, Vogt PM, Knobloch K. (2012). Analysis of hereditary and medical risk factors in Achilles tendinopathy and Achilles tendon ruptures: a matched pair analysis. Arch Orthop Trauma Surg, 132:847-853.
Publisher | Google Scholor - Egger A.C, Berkowitz M.J. (2017). Achilles tendon injuries. Curr. Rev. Musculoskelet. Med, 10:72-80.
Publisher | Google Scholor - Amendola, Francesco, et al. (2022).
Publisher | Google Scholor - Longo U.G, Petrillo S, Maffulli N, Denaro V. (2013). Acute Achilles Tendon Rupture in Athletes. Foot Ankle Clin, 18:319-338
Publisher | Google Scholor - MANSUR, Nacime Salomão Barbachan et al. (2021). Achilles Tendon Lesions–Part 2: Ruptures. Revista Brasileira de Ortopedia, 55:665-672.
Publisher | Google Scholor - Westin O, Nilsson Helander K, Grävare Silbernagel K, Möller M, Kälebo P. et.al. (2016). Acute Ultrasonography Investigation to Predict Reruptures and Outcomes in Patients with an Achilles Tendon Rupture. Orthop J Sports Med, 4(10):2325967116667920.
Publisher | Google Scholor - McCullough KA, Shaw CM, Anderson RB. (2014). Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv, 23(04):179-183.
Publisher | Google Scholor - Dams O.C, Reininga I.H, Gielen J.L, Akker-Scheek I.V.D, Zwerver J. (2017). Imaging modalities in the diagnosis and monitoring of Achilles tendon ruptures: A systematic review. Injury, 48:2383-2399.
Publisher | Google Scholor - Liberati A, Altman DG, Tetzlaff J, et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med, 6(7):1000100
Publisher | Google Scholor - Myhrvold SB, Brouwer EF, Andresen TKM, Rydevik K, Amundsen M. et.al. (2022). Nonoperative or Surgical Treatment of Acute Achilles' Tendon Rupture. N Engl J Med, 386(15):1409-1420.
Publisher | Google Scholor - Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Siira P.et. al. (2016). A Prospective Randomized Trial Comparing Surgical and Nonsurgical Treatments of Acute Achilles Tendon Ruptures. Am J Sports Med, 44(9):2406-2414.
Publisher | Google Scholor - Manent A, López L, Corominas H, Santamaría A, Domínguez A. et.al. (2019). Acute Achilles Tendon Ruptures: Efficacy of Conservative and Surgical Treatment (Percutaneous, Open) - A Randomized, Controlled Clinical Trial. Ankle surg with foot J, 58(6):1229-1234.
Publisher | Google Scholor - Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR. et.al. (2010). Surgical versus nonsurgical treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am, 92(17):2767-2775.
Publisher | Google Scholor - Kosiol J, Keiler A, Loizides A, Gruber H, Henninger B, Bölderl A, Gruber L. (2023). Surgical versus conservative treatment of acute Achilles tendon ruptures: preliminary results of clinical outcome, kinematic MRI, and contrast-enhanced ultrasound. Arch Orthop Trauma Surg, 143(5):2455-2465.
Publisher | Google Scholor - Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. (2012). Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am, 94(23):2136-2143
Publisher | Google Scholor - Kocher MS, Bishop J, Marshall R, Briggs KK, Hawkins RJ. (2002). Operative versus nonoperative management of acute Achilles tendon rupture: expected-value decision analysis. Am J Sports Med, 30:783-790.
Publisher | Google Scholor - Keating JF, Will EM. (2011). Operative versus non-operative treatment of acute rupture of tendo Achillis: a prospective randomised eva- luation of functional outcome. J Bone Joint Surg Br, 93(08):1071-1078.
Publisher | Google Scholor - Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. (2010). Acute achilles tendon rupture: a randomized, controlled study comparing sur- gical and nonsurgical treatments using validated outcome mea- sures. Am J Sports Med, 38(11):2186-2193.
Publisher | Google Scholor - Wong J, Barrass V, Maffulli N. (2002). Quantitative review of operative and nonoperative management of Achilles tendon ruptures. Am J Sports Med, 30:565-575.
Publisher | Google Scholor - Khan RJ, Fick D, Brammar TJ, Crawford J, Parker MJ. (2004). Inter- ventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev.
Publisher | Google Scholor - Tejwani NC, Lee J, Weatherall J, Sherman O. (2014). Acute Achilles tendon ruptures: a comparison of minimally invasive and open approach repairs followed by early rehabilitation. Am J Orthop (Belle Mead NJ), 43:221-225.
Publisher | Google Scholor - Aracil J, Pina A, Lozano JA, Torro V, Escriba I. (2016). Percutaneous suture of Achilles tendon ruptures. Foot Ankle, 13:350-1351.
Publisher | Google Scholor - Gorschewsky O, Pitzl M, Putz A, Klakow A, Neumann W. (2004). Per- cutaneous repair of acute Achilles tendon rupture. Foot Ankle Int, 25:219-224.
Publisher | Google Scholor - Henríquez, Hugo, et al. (2012).
Publisher | Google Scholor - Haji A, Sahai A, Symes A, Vyas JK. (2004). Percutaneous versus open tendo Achilles repair. Foot Ankle Int, 25:215-218.
Publisher | Google Scholor - Daghino W, Enrietti E, Sprio AE, di Prun NB, Berta GN, Masse A (2016) Subcutaneous Achilles tendon rupture: a comparison between open technique and mini-invasive tenorrhaphy with Achillon((R)) suture system. Injury, 47(11):2591-2595.
Publisher | Google Scholor - Fitz Gibbons RE, Hefferon J, Hill J. (2016). Percutaneous Achilles tendon repair. Am J Sports Med, 21:724-727.
Publisher | Google Scholor - Maes R, Copin G. (2006). Is percutaneous repair of the Achilles tendon a safe technique? A study of 124 cases. Acta Orthop Belg, 72:179-183.
Publisher | Google Scholor - Majewski M, Rohrbach M, Czaja S, Ochsner P. (2006). Avoiding sural nerve injuries during percutaneous Achilles tendon repair. Am J Sports Med, 34:793-798.
Publisher | Google Scholor - Assal M, Jung M, Stern R, Rippstein P, Delmi M, Hoffmeyer P. (2002). Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am, 84:161-70.
Publisher | Google Scholor - Bartel AFP, Elliott AD, Roukis TS. (2014). Incidence of complications after Achillon1 mini-open suture system for repair of acute midsubstance Achilles tendon ruptures: a systematic review. J Foot Ankle Surg, 53:744-746.
Publisher | Google Scholor - Del Buono A, Volpin A, Maffulli N. (2014). Minimally invasive versus open surgery for acute Achilles tendon rupture: a systematic review. Br Med Bull, 109:45-54.
Publisher | Google Scholor