Case Report
Surgical Challenge in Facial Arteriovenous Malformations: Case Reports
- López-Vázquez M.E 1
- García-García L.G 1
- Cisneros-Tinoco MA 2
- Hernández-Reyes A 2
- Grave-Díaz M.C2, Flores-Othón S 2
- Jiménez-Martínez C 2
- Torres-Hernández Rosa Maria 2*
1Instituto Mexicano del Seguro Social. UMAE 14, Mexico. 2Universidad Veracruzana UV-CA-477, Mexico.
*Corresponding Author: Torres-Hernández Rosa Maria, Instituto Mexicano del Seguro Social. UMAE 14, Mexico. 2Universidad Veracruzana UV-CA-477, Mexico.
Citation: Cite this article: López VME, García LG, Hernández RA, Grave DMC, Flores OS. Jiménez MC, Torres HRM et al. (2024). Surgical Challenge in Facial Arteriovenous Malformations: Case Reports. Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(5):1-6. DOI: 10.59657/2837-2565.brs.24.204
Copyright: © 2024 Rosa María Torres Hernández, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 09, 2024 | Accepted: November 23, 2024 | Published: November 30, 2024
Abstract
Introduction: Arteriovenous malformations (AVMs) are a subtype of congenital vascular malformation due to a failure in angiogenesis. They are present from birth, become more evident during individual growth, and their management depends on the case and impact, with options for conservative, surgical, endovascular, or hybrid interventions.
Objectives: To describe the surgical approach in patients with facial arteriovenous malformations at our care center.
Materials and Methods: Observational, descriptive, retrospective study of case series. We analyzed diagnostic methodology, therapeutic strategies, complications, and patient-reported outcomes.
Results: Two patients underwent exclusion of facial arteriovenous malformations via open surgical intervention in conjunction with plastic and reconstructive surgery, achieving complete exclusion of lesions, adequate postoperative recovery, and no recurrence of lesions after one year of follow-up. The only complication noted was the presence of ptosis in one patient.
Conclusion: Treatment of arteriovenous malformations is challenging due to the need to replace diseased tissue with flap rotation, which is a therapeutic option for anatomically accessible lesions.
Keywords: arteriovenous malformation; exclusion of malformation; flap rotation; vascular surgery; congenital
Introduction
Congenital vascular malformations (CVMs) and vascular tumors exhibit different anatomical, histological, pathophysiological, and clinical presentation behaviors. CVMs result from a failure in angiogenesis, becoming evident at birth and correlating with patient growth. Arteriovenous malformations (AVMs) are rare, representing 1.5% of all vascular anomalies, with 50% located in the oral and maxillofacial regions. The distinction between CVMs and vascular tumors was described by Mulliken and Glowacky (1982), who classified them based on the predominant endothelial characteristics and hemodynamic status as low-flow and high-flow lesions, assessed through physical examination and natural evolution. Hamburg's classification (1988) is based on anatomical and pathophysiological characteristics, distinguishing between trunk malformations and extraarticular malformations. The former are large-caliber vessels, while the latter consist of small vessels infiltrating adjacent tissues [1,2].
An AVM is an abnormal connection between nourishing arteries and draining veins, resulting in a constant alteration in the normal capillary bed. The draining veins appear dilated and tortuous, with increased arterial pressure in the beds and high flow, dilating normal and latent arteriovenous shunts. Local ischemia and minor trauma play roles in the growth of these malformations. In the facial area, these defects are typically limited to a small region; however, when multiple and large, systemic hereditary conditions should be considered. The approach to these patients is based on a clinical history detailing the evolution of the lesion and clinical presentation, along with adequate physical examination and imaging studies such as Doppler ultrasound, contrasted tomography, or magnetic resonance imaging to provide information about blood flow and lesion extent [3-6].
Case Reports
Case 1
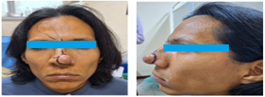
A 34-year-old male patient, referred by the otolaryngology service, had a relevant medical history of positive serology for HIV, currently under control, and a history of treated pulmonary tuberculosis. In 2012, he presented with a progressively growing, painful nasal tumor that showed a change in coloration. Doppler ultrasound revealed a continuous monophasic flow (Figure 1).
Figure 1: Patient with a nasal tumor approximately 2 cm in size, with evident aesthetic compromise in the region, showing skin discoloration in the tumor area.
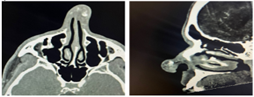
Figure 2: Angio tomography in arterial phase, transverse and coronal planes, showing a predominantly left nasal tumor due to an AVM classified as Yakes I, Schobinger II.
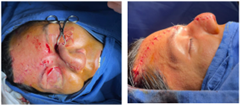
During external diagnostic evaluation, an Angio tomography in the arterial phase of the facial area was performed, revealing a subcutaneous lesion in the soft tissues of the nose, composed of tortuous and dilated vascular structures, supplied by the left lateral nasal branch of the facial artery (Figure 2). A multidisciplinary approach with the plastic and reconstructive surgery service was decided for the exclusion of the malformation, aiming to preserve the structure and aesthetics of the facial region. A fusiform incision was made at the nasal tip, with dissection revealing the vascular malformation measuring 2.5 x 3 cm. The nourishing artery, 1.5 mm in diameter, was identified, ligated, and sectioned. The plastic and reconstructive surgery team performed a rotation flap from the frontal region to the nasal tip, followed by layered closure (Figures 3 and 4).
Figure 3: Intraoperative image showing nasal approach where the nasal AVM, approximately 2.5 x 3 cm in diameter, was excluded.
Figure 4: Rotation of the frontal flap towards the nasal tip performed by the plastic and reconstructive surgery team.
In a second surgical session, the previously mentioned flap was released (Figure 5). Postoperatively, the patient maintained good overall conditions during hospitalization and was discharged shortly after.
Figure 5: Release of the frontal flap.
During follow-up in outpatient consultation, the patient showed complete recovery, with surgical wounds healed, maintaining facial aesthetics and no signs of mass or tumor recurrence. Histopathological reports described an AVM with lesion at the nasal tip (Figure 6).
Figure 6: Image of the patient at 12 months post-surgery.
Case 2
A 25-year-old female patient, with no known chronic-degenerative diseases, a history of cesarean section three years ago, and chronic hormonal contraceptive therapy, was referred by the general surgery service. She began experiencing symptoms at age 20, reporting an increase in volume in the right malar region, with pain alleviated by analgesics, which intensified with heat exposure and during her menstrual cycle (Figure 6). Upon examination, a soft, pulsatile nodular lesion was identified, with continuous monophasic flow on Doppler ultrasound. The Doppler ultrasound confirmed a facial AVM (Figure 7).
Figure 6: Female patient with increased volume in the right malar region.
The patient was hospitalized for further extension studies and to identify the affected vascular bed. Right external carotid arteriography revealed an AVM in the right hemiface dependent on the maxillary artery, with tortuous nourishing branches approximately 2 mm in diameter draining into the internal jugular vein, confirming the diagnosis of AVM, classified as Yakes 2a, Schobinger II (Figure 7).
Figure 7: Selective diagnostic arteriography of the right external carotid artery showing an AVM dependent on the maxillary artery with venous return through the internal jugular vein.
The case was discussed with the plastic and reconstructive surgery team for a joint approach to the facial area, and a Mustardé-type flap rotation was scheduled for the right hemiface. During the procedure, the AVM dependent on the maxillary artery measuring 3 x 4 cm and two nourishing arteries—one 2 mm and another 3 mm in diameter—were identified, ligated, and sectioned. The contents included abundant fibrous, muscular, and bony tissue (Figure 8).
Figure 8: Intraoperative images showing AVM dependent on the right maxillary artery, which was excluded and exposed beneath the Mustardé facial flap.
Postoperative control in outpatient consultation showed adequate healing of wounds without recurrence of tumor formations, and the patient resumed daily activities. Right palpebral ptosis was observed, leading to a referral to rehabilitation and ophthalmology services, with recovery of symmetry at six months. Histopathology reports revealed fibroadipose tissue with the AVM completely resected (Figure 9).
Figure 9: Patient in postoperative follow-up with adequate evolution of surgical wounds and facial symmetry.
Discussion
Facial and neck AVMs are rare, congenital, high-flow lesions characterized by abnormal communication between nourishing arteries and draining veins without intervening capillaries. They represent the most dangerous type of vascular malformation due to their progressive symptoms and infiltration that can have potentially fatal consequences. Focusing specifically on AVMs, they are described within the Yakes classification and categorized based on their morphology into nidus and fistula types, useful for directing specific therapeutic methods. Determining the origin of the afferent vessels in the arterial system and drainage into the normal venous system is part of a mapping process to identify the extent of arterialized flow within the venous system and document associated tissue hypertrophy or atrophy alongside adjacent normal structures, such as muscles and nerves [7-9].
The Schobinger classification for AVMs is valuable for the clinical evaluation of the actual state of the vascular anomaly. Characteristics include Stage I (Quiescence): redness, pinkish/blue coloration, Doppler flow; Stage II (Expansion): growth, pulsation, thrill, murmur, tortuous veins; Stage III (Destruction): dystrophic skin changes, ulceration, bleeding, pain; and Stage IV (Decompensation): heart failure. In the early stages of the lesion, surface moisture may be employed to prevent ulcerative lesions, reducing pain and edema. If bleeding occurs, local compression can control it. Estrogen intake, being proangiogenic, can stimulate progression, making progesterone-based contraceptives advisable [10,11].
The treatment of AVMs is complex; despite successful surgical or endovascular resection, there remains a possibility of recurrence, even at a larger size than the original, with blood supply from technically inaccessible vessels. Various therapeutic modalities exist—surgical, endovascular, or hybrid—with heterogeneous outcomes reported. In facial interventions, flap rotation is recommended to avoid deformity. The surgical approach alone poses multiple technical challenges, including the risk of bleeding, difficulty in determining the natural extent of the lesion, resulting in excessive tissue resection, and potential recurrence risk in areas distant from the central nidus. Surgical eradication of AVMs primarily involves ligation of nourishing arteries and draining veins, followed by subsequent exclusion of the corresponding bed. In some instances where endovascular therapy is considered first-line, embolization alone may be insufficient for extensive malformations, necessitating a multimodal approach for peripheral lesions. Endovascular therapy should be preferred as a first option in lesions not accessible by conventional surgery and as initial therapy when resources are available. However, endovascular therapy also poses risks when intervening in facial regions, as communications may access the external carotid artery and subsequently the internal carotid artery, with a high risk of embolization, similarly concerning the ophthalmic artery [12-15].
In the two cases presented with facial AVMs, surgical intervention was performed in conjunction with the plastic and reconstructive surgery service, preceded by thorough imaging studies, including Angio tomography, diagnostic arteriography, and tomography. These represent a fundamental pillar in managing these patients, as they identify the magnitude of the malformation, nourishing arteries, and inflow veins, the nidus, and the relationship with other structures, establishing a basis for the intervention, whether endovascular, surgical, or hybrid [16].
In the case of facial AVMs, they represent a technical challenge for the vascular surgeon, with the importance of preserving facial aesthetics. A multidisciplinary approach with the plastic and reconstructive surgery team is essential to obtain adequate and extensive exposure of the area to be treated while preserving anatomy and aesthetics, optimizing surgical procedure outcomes, which was the primary focus of our approach [17].
Conclusion
Congenital arteriovenous malformations are a subgroup of vascular malformations causing abnormal flow from the arterial to the venous system, generating an aberrant vascular bed that, despite being present from birth, becomes evident only as the individual grows, influenced by certain extrinsic factors. The treatment of arteriovenous malformations in the head and neck requires a multidisciplinary approach to achieve the best clinical outcomes, particularly given the anatomical localization of lesions in the facial region. An appropriate therapeutic approach is essential for optimal function and aesthetics, with positive outcomes reflected from planning, surgical intervention, discharge, outpatient follow-up, and the patient's reintegration into daily activities.
Declarations
Conflict of Interest
The authors declare no conflicts of interest regarding this publication.
Ethical Responsibilities
None
Protection of Persons and Animals
The authors declare that no experiments were conducted on humans or animals for this research.
Confidentiality of Data
The authors declare that they have followed the protocols of their work center regarding the publication of patient data.
Right to Privacy and Informed Consent
The authors declare that no patient data appear in this article. Furthermore, patients signed informed consent prior to intervention.
References
- Rendón-Elías, F. G., Hernández-Sánchez, M., Albores-Figueroa, R., Montes-Tapia, F. F., & Gómez-Danés, L. H. (2016). Congenital vascular malformations Update. Revista Medicina Universitaria, 16(65):184-198.
Publisher | Google Scholor - Shabbir F, Rashid M. Khan I, Sarwar R. (2024). Our Experience in the Surgical Management of Arterio-Venous Malformations of the head and neck. JPRAS Open, 40: 59-67.
Publisher | Google Scholor - Steiner, J., & Drolet, B. (2017). Classification of vascular anomalies: An update. Seminars in interventional radiology, 34:225-232.
Publisher | Google Scholor - Kim, E. T., Lee, Y., Park, D. W., & Lee, S. R. (2010). Arteriovenous Fistula at Scalp: Rapid Progression After Embolization of Contralateral Facial Arteriovenous Malformation. Neurointervention. 5:36.
Publisher | Google Scholor - Hunasgi, S., Koneru, A., Vanishree, M., & Manvikar, V. (2019). Giant arteriovenous malformation of the face and upper lip. Journal Of Oral And Maxillofacial Pathology. 23:32.
Publisher | Google Scholor - Park, H., Kim, J. S., Park, H., Kim, J. Y., Huh, S., Chung, H. Y. et al. (2019). Venous malformations of the head and neck: A retrospective review of 82 cases. Archives of Plastic Surgery, 46:23-33.
Publisher | Google Scholor - Chi C, Minh LM, Luu NG, Anh NN. (2023). Recurrent head and neck arteriovenous malformations: A case report. Radiology Case Reports, 18:766-770.
Publisher | Google Scholor - De Carvalho, M. F., De Oliveira, N. K., Duailibi, E., Da Graça Naclério Homem, M., et al. (2014). Extensive arteriovenous malformation in the face of a pediatric patient – Case report. Rev Port Estomatol Med Dent Cir Maxilofac, 55:250-255.
Publisher | Google Scholor - Dawkins, D., Motiwala, M., Peterson, J., Gleysteen, J., Fowler, B., (2022). Head and neck arteriovenous malformations: University of Tennessee experience, 2012–2022. Neurosurg Focus, 53:E17.
Publisher | Google Scholor - Lee, B. B., Baumgartner, I., Berlien, P., Bianchini, G., Burrows, P., et al. (2015). Diagnosis and treatment of venous malformations. Consensus document of the international union of phlebology (IUP): Int Angiol, 34:97-149.
Publisher | Google Scholor - Mohr, J. P., Parides, M. K., Stapf, C., Moquete, E., Moy, C. S. (2014). Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. The Lancet, 383:614-621.
Publisher | Google Scholor - Kumar, S., Kumar, V., Kumar, S., & Kumar, S. (2014). Management strategy for facial venous malformations. Natl J Maxillofac Surg., 5:93-6.
Publisher | Google Scholor - Bhandari, P. S., Sadhotra, L. P., Bhargava, P., Bath, A. S., Mukherjee, M. K., & Maurya, S. (2008). Management strategy for facial arteriovenous malformations. Indian J Plast Surg, 41:183-189.
Publisher | Google Scholor - Shoukr, T., Khalek, H. A., & Sadaka, M. (2023). Extensive Facial Arterio-Venous Malformations; Combined Approach, Embolization Followed by Surgical Reconstruction. Deleted Journal. 47:165-171.
Publisher | Google Scholor - Jia, H., Jin, Y., Hua, C., Yang, X., & Lin, X. (2022). Multimodal treatment for a giant unresectable peripheral arteriovenous malformation. Journal of Vascular and Interventional Radiology: JVIR, 33:1443-1445.
Publisher | Google Scholor - Ornelas-Flores, M. C., Rojas-Reyna, G. A., Hinojosa-Gutiérrez, C. (2021). Endovascular management of a complex high-flow lower limb arteriovenous malformation: Case report and literature review. Cirugia y Cirujanos, 89(S1):14-19.
Publisher | Google Scholor