Case Report
Significance of Duplicated Internal Jugular Vein in Neck Dissections: A Rare Case Report
1Junior Resident, Department of Community and Family Medicine, All India Institute of Medical Sciences, Patna, India.
2Senior Resident, Department of General Surgery, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India.
*Corresponding Author: Parvati Roy, Junior Resident, Department of Community and Family Medicine, All India Institute of Medical Sciences, Patna, India.
Citation: Roy P., Anto J. (2024). Significance of Duplicated Internal Jugular Vein in Neck Dissections: A Rare Case Report, Journal of BioMed Research and Reports, BioRes Scientia Publishers. 5(5):1-4. DOI: 10.59657/2837-4681.brs.24.115
Copyright: © 2024 Parvati Roy, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 07, 2024 | Accepted: October 21, 2024 | Published: October 28, 2024
Abstract
Introduction: This presentation aims to report an unusually duplicated Internal Jugular Vein that presents a significant surgical difficulty.
Case Presentation: A 45-year-old woman diagnosed with squamous cell carcinoma of the lower gingivo-buccal sulcus on her right underwent right modified radical neck dissection type II with reconstruction using pectoralis major myocutaneous flap, followed by broad local excision of the lesion with right Hemi-mandibulectomy. The right side's IJV duplication into the anterior and posterior divisions was discovered during level IV dissection in MRND. After surgery, nothing unusual happened. To avoid iatrogenic harm to IJV during neck dissections, it is helpful to be aware of the many IJV abnormalities. After a contrast-enhanced CT scan, IJV abnormalities are only described in a few cases.
Conclusion: When dissecting lymph nodes in MRND, a meticulous anatomical delineation combined with a preoperative evaluation of contrast-enhanced CT images of the face and neck is quite helpful.
Keywords: vascular malformations; radical neck dissection; squamous cell cancer
Introduction
The primary vein supplying the head and neck tissues, the internal jugular vein (IJV), has anatomic abnormalities that are not often recognized. To the best of our knowledge, 29 instances of duplicated IJV with a 0.9% prevalence have been documented to date [1]. Based on morphological features, Nayak et al. (2017) divided duplicated IJV abnormalities into Types A, B, and C [2]. Two of the five type C IJVD cases that have been documented are bilateral [2]. We have another example of this kind, which is our case—a type C categorization with unilateral duplication. The purpose of this presentation is to describe an uncommon duplicated IJV that presents significant surgical challenges and necessitates delicate dissection and more time to avoid damage and catastrophic haemorrhage.
Case Report
We report the case of a 45-year-old female patient who came to our institute in July 2024 with squamous cell carcinoma of the right lower gingivo-buccal sulcus in the T4a N2c M0 stage (Figure 1).
Figure 1: squamous cell carcinoma of the right lower gingivo-buccal sulcus in the T4a N2c M0 stage.
She had right hemi-mandibulectomy and right modified radical neck dissection (MRND) type II for extensive local excision of the lesion, conserving the spinal accessory nerve and the inferior ischium, and sacrificing the sternocleidomastoid with reconstruction using the pectoralis major myo-cutaneous flap (PMMC) (Figure 2).
Figure 2: The postoperative image of a patient who underwent wide local excision of the lesion with right Hemi-mandibulectomy and right modified radical neck dissection and pectoralis major myo-cutaneous flap.
Duplicate IJV was not known to our operational staff. On the right side, duplication of IJV into anterior and posterior division was seen after level IV dissection in MRND (Figure 3).
Figure 3: Duplication of IJV into anterior and posterior division was noted on the right side.
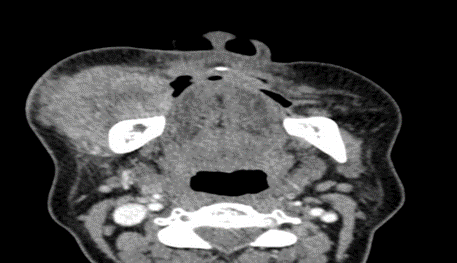
IJV duplication began in the vicinity of the hyoid bone. The anterior and posterior divisions of the IJV initially flowed into the right subclavian vein, but the two divisions remained distinct. The vagus nerve and accessory nerve both continued along their regular anatomical paths. Even after the IJV's anterior and posterior divisions were preserved, adequate lymph node clearance was still achievable. Determining the architecture and course of IJV took longer than normal because the duplication was previously unknown. Recovery from surgery went smoothly. There was no incident throughout the recovery time. On the fourteenth postoperative day, the patient was released with satisfactory clinical progress. To prevent damage to the vascular structures in the neck, a preoperative examination of a contrast-enhanced CT scan of the face and neck is required (Figure 4).
Figure 4: Preoperative CT scan of face showing lesion of size 7.3 x 5.2 x 3.1 cm involving right lower gingivobuccal sulcus.
Discussion
| Reference | Study Type | Study Objective | Methodology | Findings | Relevance to Current Case |
| Wang et al. (2020) | Case Report | To determine the prevalence and clinical significance of IJV duplication | Clinical case review of IJV duplication in surgical patients | Reported a prevalence of 0.9%, highlighting the surgical challenges posed by IJV abnormalities | Confirms rarity and emphasizes need for careful preoperative planning to avoid iatrogenic injury during neck dissections |
| Nayak et al. (2017) | Anatomical Study | To classify IJV duplications based on morphological patterns | Categorization of IJV duplications into Types A, B, C based on anatomical differences | Describes type C IJV duplication, which begins at the level of the hyoid bone | Relevant as the current case involves Type C IJV duplication; provides basis for understanding the surgical complexity |
| Prades et al. (2002) | Case Series | To assess anatomical variations in IJV in a clinical setting | Retrospective analysis of neck surgeries, focusing on vascular variations | Reported a prevalence of 0.4% for IJV duplications | Highlights importance of recognizing anatomical variations during neck surgery |
| Gupta et al. (2015) | Case Report | To present a rare case of bilateral IJV duplication | Presentation of surgical challenges and outcomes in managing bilateral IJV duplication | Emphasized the risk of injury and complications in bilateral IJV duplication cases | Though unilateral in this case, provides context on how duplicated IJVs can complicate surgery |
| Suh et al. (2014) | Surgical Review | To examine the importance of preoperative imaging in neck dissections | Review of cases requiring preoperative contrast-enhanced CT scans | Found that preoperative imaging significantly reduces intraoperative complications | Supports the conclusion that contrast-enhanced CT should be standard practice in planning neck dissections to avoid complications |
Head and neck procedures often include the vascular structures such as the carotid artery and internal jugular vein (IJV). When performing preventative or therapeutic lymph node dissections in the neck, the anatomical path of the IJV is used as a point of reference. For medication delivery, volume resuscitation, and central venous pressure monitoring following the implantation of the central venous catheter, anesthetists also consider the location of the IJV to be clinically relevant. It is even more difficult to prevent harm and catastrophic bleeding in these cases when there is anatomic variance such as IJV duplication. Case reports and case series are used to calculate the prevalence of IJV duplication. According to recent research by Wang et al. (2020) [3,1], it is around 0.9% and 0.4% in Prades et al. (2002). Understanding the various IJV abnormalities can help to prevent iatrogenic damage to the IJV during neck dissections. Additionally, it guards against damage to the spinal accessory nerve during its passage through the IJV duplication [2]. These IJV abnormalities lack a well-defined Aetiology [1]. To explain these abnormalities, however, a number of vascular, neurological, skeletal, and muscular theories have been put forth [4,5]. IJV duplication abnormalities were categorized by Nayak et al. (2017) according to their morphological patterns, each of which has a unique set of possible clinical consequences [2].
Type A
Beginning above the level of the inferior border of the posterior belly of the digastric muscle, the IJV is visible. Duplicate veins unite above or near the level of the omohyoid muscle's central tendon. For the duration of their journey, duplicated IJVs were contained in the carotid sheath.
Type B
The inferior omohyoid tendon is the continuation of the caudal portion of duplicated IJV. The sole distinction between type B and type A is this.
Type C
At the level of the hyoid bone is where the duplication begins. The posterior component travels via the posterior triangle of the neck, passes lateral to the omohyoid muscle, and then enters the carotid sheath near the root of the neck.
Based on Nayak et al.'s categorization, our case falls within Type C. Before neck dissections, preoperative planning requires the utilization of a three-dimensional, surface-rendered CT scan [6]. IJV abnormalities, however, are only reported in a small number of instances following a contrast-enhanced CT scan, which illustrates how little consideration is given to the venous system when a pathologic adenopathy is present [1]. Intraoperative direct visualization is the most widely used diagnostic technique documented in the literature for the identification of duplicated IJV [7]. The path of a duplicated IJV is comparable to a bullet's unusual trajectory in gunshot wounds [8]. As a result, working close to vascular structures shouldn't be done in the dark.
Conclusion
Hence, knowledge of the various courses of duplicated IJV and meticulous, impartial anatomical delineation are required for lymph node dissection in MRND. In every case where a neck dissection is planned, we also advise a preoperative examination of a contrast-enhanced CT scan of the face and neck.
Patients’ Perspective
I am thankful to the surgery team for saving my life. I was helpless after diagnosing it as carcinoma oral cavity.
Declarations
Funding
The authors did not receive support from any organization for the submitted work.
Conflicts of Interest/Competing Interests
There are no conflicts of interest and the authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
This is a case report. The Institutional Research Committee has confirmed that no ethical approval is required.
Consent to Participate
Not applicable.
Written Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Availability of Data and Material
The data and materials used in this case report is an original work done by the authors.
Code Availability
Not applicable.
Declaration of Generative AI and AI-Assisted Technologies in the Writing Process
During the preparation of this work the author(s) used Quillbot.com in order to paraphrase. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
References
- Wang X, Peng L, Guo H, Hernesniemi J, Xiong X, et al. (2020). Internal Jugular Vein Fenestration and Duplication: Anatomical Findings, Prevalence, and Literature Review. Front Surg. 7:593367.
Publisher | Google Scholor - Nayak SP, Ashraf M, Dam A, Biswas J. (2017). Internal Jugular Vein Duplication: Review and Classification. Indian J Surg Oncol. 8(2):222-226.
Publisher | Google Scholor - Prades J, Timoshenko A, Dumollard J, Durand M, Merzougui N, et al. (2002). High Duplication of The Internal Jugular Vein: Clinical Incidence in The Adult and Surgical Consequences, A Report of Three Clinical Cases. Surg Radiol Anat. 24(2):129.
Publisher | Google Scholor - Downie SA, Schalop L, Mazurek JN, Savitch G, Lelonek GJ, et al. (2007). Bilateral Duplicated Internal Jugular Veins: Case Study and Literature Review. Clin Anat. 20:260-266.
Publisher | Google Scholor - Contrera KJ, Aygun N, Ward BK, Gooi Z, Richmon JD. (2016). Internal jugular vein duplication and fenestration: case series and literature review. Laryngoscope. 126:1585-1588.
Publisher | Google Scholor - Wong BYW, Strachan DR, Loney EL. (2010). Duplication of Internal Jugular Veins: Case Report. J Laryngol Otol. 124(3):341-344.
Publisher | Google Scholor - Mumtaz S, Singh M. (2019). Surgical Review of The Anatomical Variations of The Internal Jugular Vein: An Update for Head and Neck Surgeons. Ann R Coll Surg Engl. 101(1):2-6.
Publisher | Google Scholor - Anto J, Kumar A, Kumar A, Anwer M, Kumar S, et al. (2022). Gunshot Injury to The Chest Wall with An Unusual Bullet Trajectory: A Rare Case Report. Int J Surg Case Rep. 96:107343.
Publisher | Google Scholor