Case Report
Role of High-Volume Plasma Exchange (HVPLEX) in Acute Liver Failure (ALF) and Our Experiences in A Tertiary Health Care Center-Few Cases Reports
- Kalyan Broto Roy *
Specialist, Transfusion Medicine Unit, Square Hospitals Ltd, Dhaka, Bangladesh.
*Corresponding Author: Kalyan Broto Roy, Specialist, Transfusion Medicine Unit, Square Hospitals Ltd, Dhaka, Bangladesh.
Citation: Kalyan B. Roy. (2025). Role of High-Volume Plasma Exchange (HVPLEX) in Acute Liver Failure (ALF) and Our Experiences in A Tertiary Health Care Center - Few Cases Reports, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 3(1):1-5. DOI: 10.59657/2997-6103.brs.25.040
Copyright: © 2025 Kalyan Broto Roy, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 25, 2024 | Accepted: December 30, 2024 | Published: January 06, 2025
Abstract
Even if the term plasmapheresis technically refers only to the removal of plasma, it is also widely used to circumscribe therapeutic plasma exchange. Therapeutic Plasma Exchange (TPE) is a procedure where the extracellular component of the blood (Plasma) is separated from the cellular component & replaced with a colloid or crystalloid substitute, reintegrated with cellular component and returned to the patient. TPE was first employed in 1952 in multiple myeloma to control hyper-viscosity. By 1970s TPE had evolved as a treatment modality in number of neurological diseases. One randomized study and a separate case series have demonstrated the safety and potential improvement in Transplant-free survival with the use of High-Volume Plasma Exchange (HVPLEX) in Acute Liver Failure (ALF). Here we have presented three cases of Acute Liver Failure with grade II Hepatic Encephalopathy (HE), who had undergone HVPLEX (1.5 plasma volume/ session, daily 2 sessions for 3 consecutive days) with Plasma & Albumin as replacement fluid (Category I, Grade 1A: ASFA guidelines 2016) and responded dramatically. So, there is a potential value of HVPLEX in the treatment of ALF particularly those do not have the options for Liver Transplantation or other means of Extracorporeal Liver support system such as Single Pass Albumin Dialysis (SPAD) or Molecular Absorbent Recirculating System (MARS).
Keywords: plasma exchange; high volume plasmapheresis; acute liver failure
Introduction
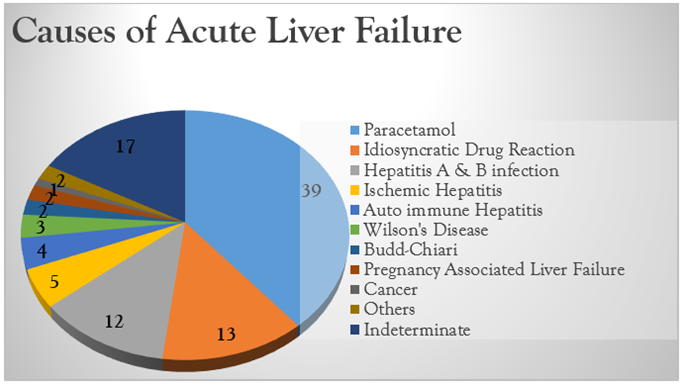
The most widely accepted definition of ALF includes, evidence of coagulation abnormality (INR1.5), any degree of mental alteration (Encephalopathy) in a patient without preexisting cirrhosis and the disease course of ≤26 weeks [1]. Common etiologies of Acute Liver Failure (ALF) include Drug (Acetaminophen) or toxin exposure, viral hepatitis, autoimmune disease and ischemia [2]. ALF can lead to irreversible shock, cerebral herniation or the development of Multi Organ Failure (MOF). The management strategy of ALF patients consists of treatment of underlying etiology if possible and to preserve the vital organ’s function or to limit /prevent the progression of MOF. Even though taking all the possible measures, some patients may develop progressive deterioration and requires Liver Transplantation. In ALF pro inflammatory cytokines and toxic metabolites are largely responsible for the development of MOF. High Volume Plasma Exchange (HVPLEX) is defined as an exchange of 8-12 L or 15% of ideal body weight with fresh-frozen plasma HVPLEX removes these cytokines and toxic substances from the systemic circulation. Therapeutic HVPLEX improves outcome in patients with ALF by increasing liver “Transplant-free” survival. This attenuates the innate immune activation and may help in amelioration of multi-organ failure [3]. Special Issue Writing Committee is charged with reviewing, updating and categorizing indications for the evidence-based use of therapeutic apheresis (TA) in human disease. Since the 2007 JCA Special Issue (Fourth Edition), the committee has incorporated systematic review and evidence-based approaches in the grading and categorization of apheresis indications [4].
Figure 1: Pie chart showing the causes of ALF.
Category Definitions for Therapeutic Apheresis
| Category | Definitions |
| Disorders for which apheresis is accepted as first-line therapy, either as a primary standalone treatment or in conjunction with other modes of treatment. | |
| Disorders for which apheresis is accepted as second -line therapy, either as standalone treatment or in conjunction with other modes of treatment. | |
| Optimum role of apheresis therapy is not established. Decision making should be individualized. | |
| Disorders in which published evidence demonstrates or suggests apheresis to be ineffective or harmful. IRB approval is desirable if apheresis treatment is undertaken in these circumstances. |
Grading
| Recommendation | Description |
| Grade 1A | Strong recommendation, high quality evidence |
| Grade 1B | Strong recommendation, moderate quality evidence |
| Grade 1C | Strong recommendation, low quality or very low-quality evidence |
| Grade 2A | Weak recommendation, high quality evidence |
| Grade 2B | Weak recommendation, moderate quality evidence |
| Grade 2C | Weak recommendation, low quality or very low-quality evidence |
Case Presentation
Case 1
A 34-year-old-woman was admitted to Square Hospitals Ltd. (SHL)with the complaints of upper abdominal pain, nausea and vomiting, yellow discoloration of skin for the last 10 days. She developed altered level of consciousness for few hours before admission to hospital. She was diagnosed as a case of Hepatitis E virus (HEV) induced Acute Liver Failure with Grade II Hepatic Encephalopathy (HE), was admitted to ICU initially. Despite the conventional treatment her condition was not improving and a plan for HVPLEX was made. We performed Iso-volume HVPLEX (9L/day in 2 sessions) for 3 consecutive days and replacement fluid used were 5% Human albumin (4L) and FFP (5L). ACD-A was used as an anticoagulant in the whole procedure. After getting 3 consecutive sessions of HVPLEX her condition dramatically improved, consciousness regained and she was shifted to cabin and later on discharged at home.
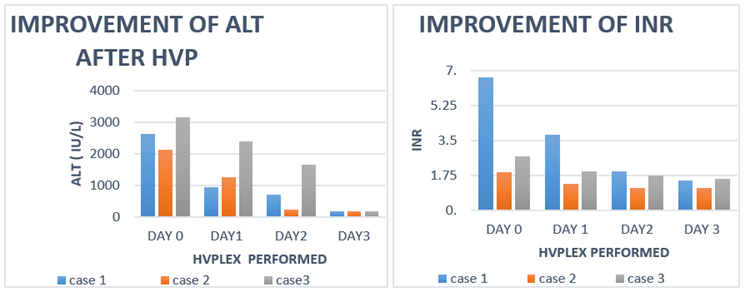
Her Biomarkers before and After HVPLEX is presented below in a tabulated form:
| Bio Markers | Before HVPLEX | After 1st session | After 2nd session | After 3rd session |
| SGPT (ALT) | 2635 U/L | 950 U/L | 715 U/L | 174 U/L |
| S. Bilirubin (Total) | 16.2 mg/dl | 10.6 mg/dl | 7.4 mg/dl | 6.8 mg/dl |
| S. Ammonia | 314 micromole/L | 136 micromole/L | 102 micromole/L | 52 micromole/L |
| INR | 6.66 | 3.77 | 1.94 | 1.50 |
Case 2
A-22-year-old gentleman with no history of co morbid illness was admitted to Square Hospitals Ltd. (SHL) with the complaints of abdominal pain, nausea, vomiting and yellow discoloration of skin for the past 7 days and altered level of consciousness for last 12 hours. Initially he was admitted to a local clinic where he was treated conservatively for 2 days but his general condition was gradually deteriorating and then he was admitted to Square Hospital. He was diagnosed as a case of Hepatitis A virus (HAV) induced ALF with HIM (Grade II) with Rhabdomyolysis and was shifted to ICU. As the patient was not responding optimally with the conventional treatment, a plan for HVPLEX was made. We performed Iso-volume HVPLEX (10L/day in 2 sessions) for 3 consecutive days and replacement fluid used were 5% Human albumin (4L) and FFP (5L), Normal Saline 500ml. ACD-A was used as an anticoagulant in the whole procedure. After HVPLEX his condition was improved dramatically and consciousness regained and he was shifted to cabin.
His biomarkers before and after HVPLEX is presented below in a tabulated form:
| Bio Markers | Before HVPLEX | After 1st session | After 2nd session | After 3rd session |
| SGPT (ALT) | 2122 U/L | 1264 U/L | 234 U/L | 187 U/L |
| S. Bilirubin (Total) | 10.4 mg/dl | 7.4 mg/dl | 5.5 mg/dl | 4.8 mg/dl |
| S. Ammonia | 112 micromole/L | 107 micromole/L | 78 micromole/L | <9> |
| INR | 1.89 | 1.34 | 1.13 | 1.10 |
| CPK | 5298 mcg/L | 660 mcg/L | 300 mcg/L | 286 mcg/L |
Case 3
A-37-year-old gentleman who was a known case of Non-alcoholic fatty liver disease (NAFLD) was admitted to Square Hospitals Ltd. (SHL). HDU with the complaints of upper abdominal pain, nausea, vomiting for several times daily for the last 7 days associated with yellow discoloration of skin and sclera. He was diagnosed as a case of Hepatitis A virus (HAV) induced Acute on Chronic Liver Failure (ACLF). The day after his admission to the HDU he developed altered level of consciousness and was shifted to ICU. As his condition was not improving a plan for HVPLEX was made. We performed 10L/day in 2 sessions for 3 consecutive days. Replacement fluid used were 5% Human albumin (4L) and FFP (5L), Normal Saline 500ml. Acd-A was the anticoagulant of choice. After getting 3 consecutive sessions he was shifted to cabin as his condition was improved and later on discharged at home.
Her biomarkers before and after HVPLEX is presented below in a tabulated form:
Figure 2: Lab parameters showing improvement with HVPLEX – ALT and INR.
Discussion
Patient monitoring is a curtail part in any Apheretic procedure. Pre-procedure checking of CBC, Electrolytes, and Coagulation profile is a must. Ensuring the patient comfort and monitoring the vitals are a must during procedure. The rate of adverse event during therapeutic apheresis is 4% to 5%, with the risk being slightly higher during the first procedure. Per procedure we did not encounter any major complications like vasovagal attack, anaphylactic reaction, Hypovolaemia or hypocalcaemia. Inj. Calcium Gluconate was given to maintain the calcium homeostasis. Frequent observation of QTC in the EKG was helpful to mitigate any feature of hypocalcaemia. To gain the vascular access we performed the procedures through Femoral or Central venous catheter. In our cases we used group specific FFPs which is safest but, in a condition, where group specific FFP is not available we can use AB group safely. We used a Cell separator of continuous centrifugation. Blood flow (Draw and return) was maintained to 50ml/min. Frequent monitoring of the vitals was done. Significant necrosis of the hepatocytes following release of cytokines and adhesion molecules which results in a large scale pro-inflammatory cascade occurs in Acute Liver Failure [5]. HVPLEX falls under the term of Extracorporeal Liver Support Systems (ECLS) where it replaces the patient’s plasma with the fresh frozen plasma and albumin [6,7]. The objective is to detoxify and regulate the serum chemistry functions or the relevant bio-markers related to ALF. By extracting the pro-inflammatory cytokines, toxins and adhesion molecules and replacing the plasma factors, this procedure helps modulating the immune system.8 The success of the HVPLEX depends on the distribution of the disease mediators and amount of the plasma removed. The more the plasma removed the more is the disease mediators be removed. One volume plasma exchange extract 63% and 1.5 plasma volume extracts 78%. 9Kaplan's equation [0.065 x weight (kg)] x (1-Hct) is the handiest equation for estimating the amount of plasma to be removed. In a prospective multicenter RCT trail by Larson et al. in 2016, 182 randomized patients of ALF were selected to receive Standard Medical Therapy (SMT) or SMT plus HVPLEX for three days. Biomarkers like bilirubin, ammonia and INR levels all dropped down significantly following HVPLEX. They found that overall hospital survival was 58.7 % for patients treated with HVPLEX vs. 47.8% for SMT group alone [8]. So, they concluded that there are benefits in transplant free survival with HVPLEX in ALF patients. In the same study a sub group of 30 patients with ALF treated with HVPLEX were shown to have significant reduction of the Damage Associated Molecular Patterns (DAMPs), such as TNF alpha, circulating histone-associated DNA, IL-4, IL-8, IL-10, CD62L, level of pro-inflammatory cytokines associated with decrease in neutrophil activation. That means reducing the systemic inflammation associated with ALF. Presently the patients with ALF whom spontaneous recovery does not occur, Liver Transplantation is the only definitive treatment. HVPLEX can allow some time to those patients until the patient becomes suitable for Transplantation [8].
In a Tertiary Center of Dhaka, Bangladesh (SQUARE HOSPITALS LTD.) since 2019 we have performed 94 successful sessions of HVPLEX in 12 ALF patients of variety of reasons. Presented below in a tabulated form.
Successfully done (HVP) (since 2019).
| Cases | Age (y) | Gender | Diagnosis | Number of Sessions |
| 1 | 55 | Male | Acute Liver Failure (HAV) | 6 |
| 2 | 50 | Male | Leptospirosis Following ALF | 8 |
| 3 | 23 | Male | Acute Liver Failure (Dapsone Induced) | 8 |
| 4 | 37 | Male | Acute Liver Failure (HAV) | 4 |
| 5 | 32 | Female | Acute Liver Failure (HEV) | 6 |
| 6 | 22 | Male | Acute Liver Failure (HAV) | 4 |
| 7 | 26 | Male | Acute Liver Failure (extended dengue syndrome) | 10 |
| 8 | 58 | Male | Leptospirosis Following ALF | 14 |
| 9 | 35 | Female | Acute Liver Failure (HAV) | 14 |
| 10 | 25 | Female | Multi Drug Overdose Induced ALF | 8 |
| 11 | 26 | Female | Multi Drug Overdose Induced ALF | 6 |
| 12 | 33 | Female | Acute Liver Failure (HEV) | 6 |
| Total | 94 Sessions |
Conclusion
Very few studies have looked at the role of HVPLEX treatment in Acute Liver Failure and also in ACLF. Further studies require to assess the benefits of HVPLEX in specific etiology of ALF. Our experience is HVPLEX is really an effective therapy mitigating the ALF and reducing the mortality as well as the chances of Liver Transplantation.
References
- Karvellas, Constantine J. et al. (2016). High Volume Plasma Exchange in Acute Liver Failure: Dampening the Inflammatory Cascade? Journal of Hepatology, 64(1):10-12.
Publisher | Google Scholor - Acute Liver Failure.
Publisher | Google Scholor - Tam L, Karvellas C, Sy E. (2020). The Use of High-Volume Plasmapheresis in Acute Liver Failure. Cureus. 12(6):e8721.
Publisher | Google Scholor - Schwartz, J., Padmanabhan, A., Aqui, N., Balogun, R.A., Connelly-Smith, L., et al. (2016). Guidelines on The Use of Therapeutic Apheresis in Clinical Practice-Evidence-Based Approach from The Writing Committee of The American Society for Apheresis: The Seventh Special Issue. J. Clin. Apheresis, 31:149-338.
Publisher | Google Scholor - Antoniades CG, Berry PA, Wendon JA, Vergani D. (2008). The Importance of Immune Dysfunction in Determining Outcome in Acute Liver Failure. J Hepatol. 49(5):845-861.
Publisher | Google Scholor - Cardoso FS, Marcelino P, Bagulho L, Karvellas CJ. (2017). Acute Liver Failure: An Up-To-Date Approach. J Crit Care. 39:25-30.
Publisher | Google Scholor - Macdonald AJ, Karvellas CJ. (2018). Emerging Role of Extracorporeal Support in Acute and Acute-On-Chronic Liver Failure: Recent Developments. Semin Respir Crit Care Med. 39(5):625-634.
Publisher | Google Scholor - Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, et al. (2016). High-Volume Plasma Exchange in Patients with Acute Liver Failure: An Open Randomized Controlled Trial. J Hepatol. 64(1):69-78.
Publisher | Google Scholor - Practical Aspects of Therapeutic Plasma Exchange (PLEX / TPE) For Neurologists. (2014).
Publisher | Google Scholor