Case Report
Pregnancy On Caesarean Scar: Conservative Treatment: In A Case and Literature Review
- R. Sabiri *
- H. Said
- FZ. El-Hachami
- M. Zein
- A. Assal
- M. Jalal
- A. Lamrissi
- S. Bouhya
Service de maternité gynecologie obstetrique hôpital mère enfant Abderahim El Harouchi, Casablanca, Morocco.
*Corresponding Author: R. Sabiri, Service de maternité gynecologie obstetrique hôpital mère enfant Abderahim El Harouchi, Casablanca, Morocco.
Citation: Sabiri R., Said H., El-Hachami FZ., Zein M., Assal A., et al. (2024). Pregnancy On Caesarean Scar: Conservative Treatment: In A Case and Literature Review, International Journal of Clinical and Surgical Pathology, BioRes Scientia Publishers. 1(2):1-5. DOI: 10.59657/3067-0462.brs.24.007
Copyright: © 2024 R. Sabiri, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 01, 2024 | Accepted: August 08, 2024 | Published: August 15, 2024
Abstract
Caesarean section scar pregnancy is an ectopic pregnancy of cervico-isthmic and cicatricial localization. It corresponds to implantation of the gestational sac in the scar or dehiscence of a previous caesarean section. In this article, we present the case of a patient diagnosed with scar pregnancy in the first trimester who benefited from conservative treatment. Pregnancy on a caesarean section scar is no longer an exceptional event. The advantage of early diagnosis lies in the possibility of choosing an appropriate treatment based on the clinical context, radiological data, technical resources and the patient's wishes.
Keywords: caesarean section scar pregnancy; conservative treatment; ectopic pregnancy
Introduction
Caesarean section scar pregnancy is an ectopic pregnancy of cervico-isthmic and cicatricial localization. It corresponds to implantation of the gestational sac in the scar or dehiscence of a previous caesarean section. The incidence is estimated at between 1/1800 and 1/2216 pregnancies [1]. This is a pregnancy at major risk of massive hemorrhage, requiring active management as soon as it is diagnosed. Analysis of the literature reveals limited series, with an increase in the number of publications relating to this subject since the 2000s and especially since 2006 [2]. The outcome of the first cases described was often hemostasis hysterectomy in the face of hemorrhage caused by treatment with primary curettage, or spontaneous metrorrhagia without etiological diagnosis. Ignorance or late diagnosis could be associated with major complications such as uterine rupture, often leading to hysterectomy [3]. We present here a case of pregnancy on a Caesarean section scar, and through a review of the recent literature, we will highlight the diagnostic and therapeutic features of this condition, which practitioners' familiarity with will help improve its prognose.
Case Report
Mrs. AS, aged 43, 4th gesture, 2nd pare, carrier of a double scarred uterus: the 1st caesarean section was due to a non-reassuring fetal condition, the 2nd was due to an overdue delivery, and an aspiration following a terminated pregnancy. She came to the gynecological emergency department with pelvic pain and light blackish metrorrhagia, which had been progressing for three days in a 9-week amenorrhea. On clinical examination, hemodynamics was stable, abdominal palpation revealed no tenderness, and speculum examination confirmed the endo-uterine origin of the pain. Vaginal touch combined with abdominal palpation revealed a slightly enlarged uterus with no latero-uterine mass or signs of peritoneal irritation. An initial ultrasound performed in the emergency department revealed the presence of a gestational sac opposite the uterine isthmus, with no embryonic echo, whose implantation appeared to be invading the myometrium (Figure 1,2).
Figure 1
Figure 2
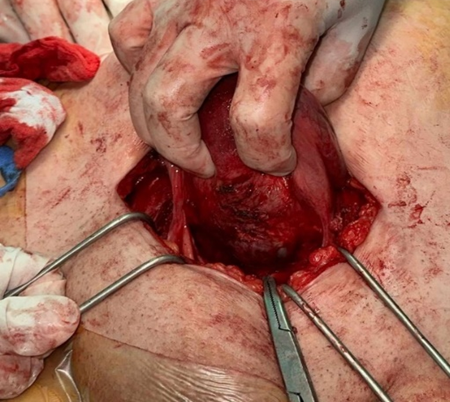
A laparotomy was performed. On exploration, we noted the presence of a left isthmic bluish swelling visible through the visceral peritoneum, whose incision after detachment and lowering of the bladder (Figure 3) revealed the exit of the product of conception (Figure 4). This was resected, along with the scar, before the hysterography was performed. Post-operative management was straightforward. The βHCG level came back negative after 2 weeks.
Figure 3
Figure 4
Discussion
Caesarean scar pregnancy is a very uncommon and potentially fatal form of abnormal implantation of a gestational sac within the myometrium and fibrous tissue of the scar.3 Prevalence ranges from 1/1800 to 1/2226 pregnancies, and corresponds to only 6.1% of ectopic pregnancies in women with early caesarean section [4]. The incriminating risk factors are similar to those for placenta accrete: on the one hand, the number of previous caesarean sections and endo-uterine procedures (curettages, manual uterine revision); on the other, in vitro fertilization (IVF) techniques with embryo transfer have also been incriminated [1,5], as the less solicited and less mature lower segment would not allow optimal quality of healing and would favor ectopic implantation of the egg [6]. Clinical manifestations include abdominal pain and bleeding, which can range from simple spotting to life-threatening haemorrhage [1]. However, clinical manifestations can sometimes be asymptomatic. All this underlines the importance of rapid and accurate diagnosis [7] in improving vital and functional prognosis. Two-dimensional endo-cavity ultrasonography is the first-line radiological examination for making the diagnosis. The latter is based on the criteria established by Vial in 2000 [8] associating firstly: an empty uterus; an empty cervical canal; the existence on a sagittal section of the uterus, of a disruption of the gestational sac on the anterior uterine wall.
is based on the criteria established by Vial in 2000 [8], which include: an empty uterus; an empty cervical canal; and, on a sagittal section of the uterus, a disruption of the gestational sac on the anterior uterine wall. Other imaging examinations may be carried out, such as three-dimensional ultrasound or MRI, which allow anatomical relationships to be determined, specifying the depth of trophoblastic invasion in the myometrium, potential involvement of the serosa or bladder, and the exact position of the gestational sac [9]. At present, there are no formal recommendations concerning treatment modalities. At present, treatment, whether medical or surgical, remains conservative, except in cases of therapeutic failure. Medical treatment in hemodynamically stable patients is feasible for many teams. It is based on the administration of methotrexate locally (injection in situ, possibly under ultrasound or co Elio guidance) or systemically, or a combination of the two, at a dose of 1mg/kg [10]. This treatment requires daily monitoring of the BHCG decrease during hospitalization, then weekly until negotiation, with ultrasound monitoring until complete disappearance of the ovarian sac, with an average time to BHCG negotiation of 4 to 6 weeks. Prognostic factors for failure of medical treatment would be: BHCG level greater than 10,000 IU/L, GA greater than 9 SA, presence of fetal cardiac activity on ultrasound, craniocaudal length of embryo greater than 10mm on ultrasound.
The need for surgical treatment is debatable. Two important clinical problems 7 may arise after poor healing of Caesarean incisions. The first is the reservoir effect of the defect, which may be linked to symptoms of post-menstrual spotting, infertility and pelvic pain with an unidentified mechanism. The second is the residua thickness of the myometrium at the site of the defect, which is a potential risk factor for uterine scar dehiscence in a subsequent pregnancy. The first clinical condition can be managed by hysteroscopic resection of the defect, but this approach obviously cannot increase the thickness of the myometrial wall, and may present a potential risk of decreased myometrial strength. residual myometrial tissue at the level of the repair and may furthermore lead to rupture in a subsequent pregnancy. The laparoscopic approach restores both conditions by eliminating the reservoir and concomitantly strengthening the myometrial wall. Most studies on hysteroscopic management of caesarean sections have provided no information on residual myometrial thickness before or after surgery [11-14].
Conclusion
Pregnancy on a caesarean section scar is no longer an exceptional event. It is now an integral part of the long-term complications of Caesarean section. It can be classified at the same level of severity as placenta accrete. The advantage of early diagnosis lies in the possibility of choosing an appropriate treatment based on the clinical context, radiological data, technical resources and the patient's wishes. This could limit the serious haemorrhagic complications that very often accompany total hysterectomy, compromising the patient's subsequent fertility when maternal death has been avoided.
Declarations
Patient Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical Approval
I declare on my honor that my establishment has exempted the ethical approval.
Sources of Funding
None.
Author’s Contribution
All authors have read and approved the final version of the manuscript.
Declaration of Competing Interest
The authors declare having no conflicts of interest in this article.
References
- Belinga E, Mbo AJ, Hanen C, Ali EH, Voulgaroupoulos M, et al. (2014). Grossesse Sur Cicatrice De Césarienne: Apport De L’échographie Dans Le Diagnostic Et La Prise En Charge. Health Sci Dis. 15(2).
Publisher | Google Scholor - Timor-Tritsch IE, Monteagudo A. (2012). Unforeseen Consequences of The Increasing Rate of Cesarean Deliveries: Early Placenta Accreta and Cesarean Scar Pregnancy. A Review. Am J Obstet Gynecol. 207(1):14-29.
Publisher | Google Scholor - Shen L, Tan A, Zhu H, Guo C, Liu D, et al. (2012). Bilateral Uterine Artery Chemoembolization with Methotrexate for Cesarean Scar Pregnancy. Am J Obstet Gynecol. 207(5):386.e1-e6.
Publisher | Google Scholor - Patel MA. (2015). Scar Ectopic Pregnancy. J Obstet Gynaecol India. 65(6):372-375.
Publisher | Google Scholor - Aymon R, Halperin R, Mendlovic S, Schneider D, Vaknin Z, et al. (2004). Ectopic Pregnancies in Cesarean Section Scars: The 8-Years’ Experience of One Medical Center. Hum Reprod. 19(2):278-284.
Publisher | Google Scholor - Maymon R, Halperin R, Mendlovic S, Schneider D, Herman A. (2004). Ectopic Pregnancies in A Caesarean Scar: Review of The Medical Approach to An Iatrogenic Complication. Hum Reprod Update. 10(6):515-523.
Publisher | Google Scholor - Rotas MA, Haberman S, Levgur M. (2006). Cesarean Scar Ectopic Pregnancies: Etiology, Diagnosis and Management. Obstetrics and Gynecology. 107(6):1373-1381.
Publisher | Google Scholor - Vial Y, Petignat P, Hohlfeld P. (2000). Pregnancy in A Cesarean Scar. Ultrasound Obstet Gynecol. 16(6):592-593.
Publisher | Google Scholor - Seow KM, Hwang JL, Tsai YL, Huang LW, Lin YH, et al. (2004). Subsequent Pregnancy Outcome After Conservative Treatment of a Previous Cesarean Scar Pregnancy. Acta Obstet Gynecol Scand. 83(12):1167-1172.
Publisher | Google Scholor - Nawroth F, Foth D, Wilhelm L, Schmidt T, Warm M, et al. (2001). Conservative Treatment of Ectopic Pregnancy in A Cesarean Section Scar with Methotrexate: A Case Report. Eur J Obstet Gynecol Reprod Biol. 99(1):135-137.
Publisher | Google Scholor - Gubbini G, Centini G, Nascetti D, et al. (2011). Surgical Hysteroscopic Treatment of Cesarean23 Induced Isthmocele in Restoring Fertility: Prospective Study. J Minimally Invasive Gynecol. 18:234-237.
Publisher | Google Scholor - Ofili-Yebovi D, Ben-Nagi J, Sawyer E, et al. (2008). Deficient Lower-Segment Cesarean Manuscript Accepted 1 Section Scars: Prevalence and Risk Factors. Ultrasound Obstet Gynecol. 31:72-77.
Publisher | Google Scholor - Florio P, Filippeschi M, Moncini I, et al. (2012). Hysteroscopic Treatment of The Cesarean Induced Isthmocele in Restoring Infertility. Curr Opin Obstet Gynecol. 24:180-186.
Publisher | Google Scholor - Wang CJ, Huang HJ, Chao A, et al. Challenges in The Transvaginal Management of Abnormal Uterine Bleeding Secondary to Cesarean Section Scar Defect. Eur J Obstet Gynecol Reprod Biol. 154:218-222.
Publisher | Google Scholor