Review Article
Percutaneous Intramyocardial Septal Radiofrequency Ablation in Patients with Hypertrophic Cardiomyopathy–A Systematic Review and Meta-analysis
1 University of Mauritius Faculty of Science Department of Medicine.
2 Kasturba Hospital Manipal.
3 Klinikum Aschaffenburg-Alzenau.
4 Dow University of Health Sciences.
*Corresponding Author: Fatema Tashrifwala, Faculty of Science, University of Mauritius, Stamford Health, USA.
Citation: Tashrifwala F, Purushotham M., Sai K.Bhushan, Hameed I. (2023). Percutaneous Intramyocardial Septal Radiofrequency Ablation in Patients with Hypertrophic Cardiomyopathy-A Systematic Review and Meta-analysis. 2(1); DOI: https://www.doi.org/brs/2023/cmi/0007
Copyright: © 2023 Fatema Tashrifwala, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 07, 2023 | Accepted: February 27, 2023 | Published: March 03, 2023
Abstract
Purpose: In this study, we aimed to meta-analyze all available data to provide a holistic, well-powered assessment of the effect of PIMSRA on LVOT gradient, LVEF, and anterior and posterior IVS thickness.
Methods: PubMed, Cochrane Central, Embase, and Scopus were systematically searched from inception till October 2022 for published clinical trials assessing the efficacy of PIMSRA in patients with HCM using the keywords “PIMSRA” OR “Percutaneous Intramyocardial Septal Radiofrequency Ablation” OR “Liwen procedure.” Studies that reported change in either LVOT gradient, IVS thickness, or LVEF were selected. No time or language restrictions were applied. All case reports were excluded, and only clinical trials were included. The search and data extraction were carried out independently by two reviewers (MP, FT). A third reviewer (IH) was consulted to resolve discrepancies. All statistical analyses were conducted on Open Meta-analyst. Trials were pooled using a continuous random effects model (DL: DerSimonian-Laird), and results were presented with 95% confidence intervals (CIs). P value 75% regarded as substantial heterogeneity.
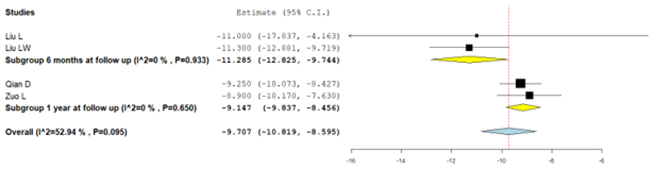
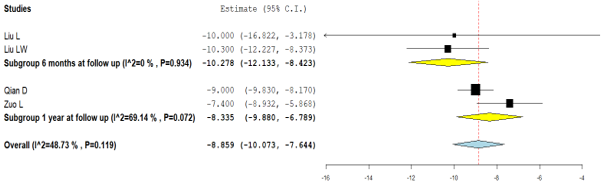
Results: All five studies reported a change in LVOT gradient from the baseline. Integrated analysis showed no significant change from baseline (MD: -69.506; 95% CI: -77.047, -61.966; P = 0.089) (I² = 50.4%). Subgroup analyses based on follow-up revealed that there was no significant difference noted at 6 months according to data from 2 studies (MD: -65.351; 95% CI; -85.253, -45.450; P = 0.181) (I²= 44.1%) however data from 3 studies at one year follow up did reveal a significant difference from baseline (MD: -71.010; 95% CI: -80.262, -61.758; P = 0.047) (I² = 67.2%). Only three studies reported changes in LVEF from the baseline. Integrated analysis Powered by Editorial Manager® and ProduXion Manager® from Aries Systems Corporation showed a significant change from baseline at one-year follow-up in patients who underwent PIMSRA (MD: -1.760; 95% CI: -3.239, -0.282; P = 0.047) (I² = 67.22%). The pooled analysis from four studies that reported anterior IVS thickness showed no significant change from baseline (MD: -9.707; 95% CI: -10.819, -8.595; P = 0.095) (I² = 52.94%). Subgroup analyses based on follow-up revealed that there was no significant difference noted at 6 months (MD: -11.285; 95% CI; -12.825, -9.744; P = 0.933) (I² = 0%) or at one-year follow-up (MD: -9.147; 95% CI: -9.837, -8.456; P = 0.650) (I² = 0%) The combined analysis of the four included studies reporting posterior IVS thickness showed no significant change from baseline (MD: -8.859; 95% CI: -10.073, -7.644; P = 0.119) (I² = 48.73%). Additionally, there was no significant difference noted in the subgroup analysis at 6 months (MD: -10.278; 95% CI; -12.133, -8.423; P = 0.934) (I² = 0%) and at one-year follow-up (MD: -8.335; 95% CI: -9.880, -6.789; P = 0.072) (I² = 69.14%)
Conclusion: This single-arm meta-analysis of 284 patients gathered from 5 clinical trials suggested that overall, after PIMSRA, LVOT gradient was reduced, and LVEF was slightly decreased. Additionally, no significant changes were observed in the anterior and posterior IVS thicknesses. Our results had substantial heterogeneity, which could be explained due to differences in the follow-up periods and studies with small sample sizes. It is important to note that even though no significant difference in follow-up was seen from the baseline at 6 months, there was indeed a significant difference noted at one year when assessing the outcomes of LVOT gradient. This could suggest that longer follow-up periods are imperative to truly observe the procedure's efficacy.
Keywords: HCOM; PIMSRA; LVOT; LVEF; anterior IVS thickness; posterior IVS thickness; efficacy
Introduction
Hypertrophic cardiomyopathy (HCM) is an autosomal dominant intrinsic disease of the myocardium characterized by asymmetric hypertrophy and stiffness of the left ventricle along with the systolic anterior motion of the mitral valve, leading to a left ventricular outflow tract (LVOT) obstruction. It affects one in five hundred people worldwide and is the most common genetic heart disease in the US [1]. The reduced volume of the heart chambers with a reduced capacity of the heart to pump blood results in a decreased stroke volume. LVOT obstruction is present at rest in about one-third of the patients. The symptoms include exertional dyspnea, exercise intolerance, orthopnea, peripheral edema, and syncope [2]. Diagnostic modalities include echocardiography, electrocardiogram (ECG), and cardiovascular magnetic resonance imaging (CMRI). Identification of the HCM phenotype can be made by family screening and genetic testing in affected individuals [3, 4]. The treatment goals are to reduce the severity of symptoms and prevent sudden cardiac death, particularly in young adults. Pharmacological treatment revolves around β-blockers or non-dihydropyridine calcium-channel blockers with the newer generation of drugs, including Mavacamten, Perhexiline, and Trimetazidine. Evaluation and follow-up are done by LVOT gradient, left ventricular ejection fraction (LVEF), and myocyte hypertrophy measured by Interventricular septum (IVS) thickness [5]. In patients who are refractory to maximum dosage (about 40%) or have an intolerance to drugs, surgical options like septal myectomy and trans-catheter mitral valve repair may be considered. The downside to these is the need for a sternotomy. Minimally invasive procedures which can instead be done are high-intensity focused ultrasonography and radiofrequency ablation, or Alcohol septal ablation (ASA), which come with their own risk of complications with chances of occurrence ranging from 0.5-5% [6]. The suitability of ASA is limited by septal coronary anatomy and the risk of alcohol being injected into the wrong site. Advancements in techniques have now led to the use of percutaneous intramyocardial septal radiofrequency ablation (PIMSRA) as a promising technique for such patients. This technique uses a radiofrequency electrode needle inserted under guidance into the hypertrophied IVS to achieve ablation [4,7]. Trials have shown reductions in IVS thickness and LVOT gradients along with improvement in New York Heart Association (NYHA) functional classification following PIMSRA, but these studies have been limited by small sample sizes, thus being underpowered to reliably demonstrate any significant differences in outcomes. In this study, we aimed to meta-analyze all available data to provide a holistic, well-powered assessment of the effect of PIMSRA on LVOT gradient, LVEF, and anterior and posterior IVS thickness.
PubMed, Cochrane Central, Embase, and Scopus were systematically searched from inception till October 2022 for published clinical trials assessing the efficacy of PIMSRA in patients with HCM using the keywords “PIMSRA” OR “Percutaneous Intramyocardial Septal Radiofrequency Ablation” OR “Liwen procedure.” Studies that reported change in either LVOT gradient, IVS thickness, or LVEF were selected. No time or language restrictions were applied. All case reports were excluded, and only clinical trials were included. The search and data extraction were carried out independently by two reviewers (MP, FT). A third reviewer (IH) was consulted to resolve discrepancies. All statistical analyses were conducted on Open Meta-analyst. Trials were pooled using a continuous random effects model (DL: DerSimonian-Laird), and results were presented with 95% confidence intervals (CIs). P value <0> 75% regarded as substantial heterogeneity.
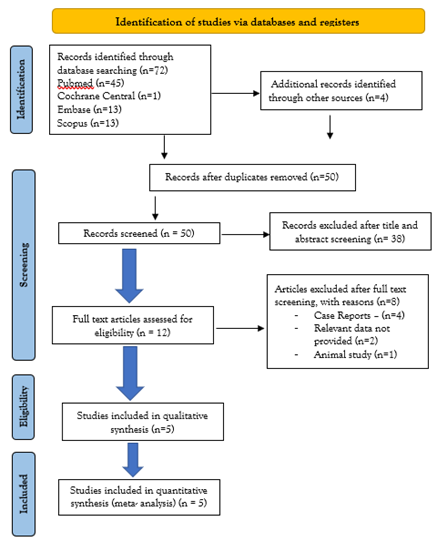
The initial search yielded 72 potential studies. After exclusions, 5 trials remained for analysis [1,3,4,7,8]. The detailed literature search is highlighted in the PRISMA Flow Chart (Supplementary Material Figure 1). The characteristics of the included studies have been summarized in Table 1.
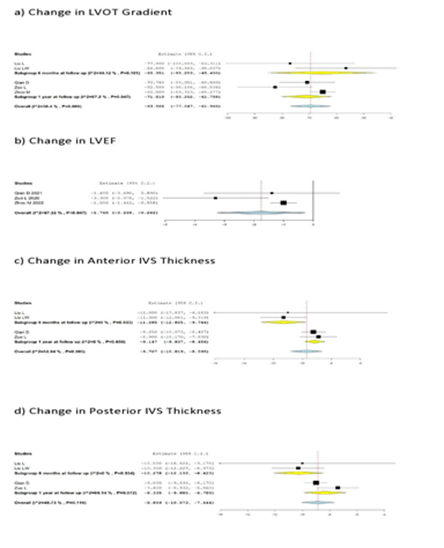
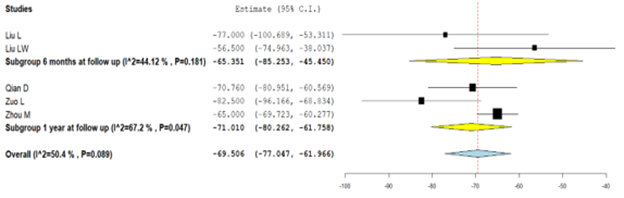
All five studies reported a change in LVOT gradient from the baseline (Figure 1A). Integrated analysis showed no significant change from baseline (MD: -69.506; 95% CI: -77.047, -61.966; P = 0.089) (I² = 50.4%). Subgroup analyses based on follow-up revealed that there was no significant difference noted at 6 months according to data from 2 studies (MD: -65.351; 95% CI; -85.253, -45.450; P = 0.181) (I²= 44.1%) however data from 3 studies at one year follow up did reveal a significant difference from baseline (MD: -71.010; 95% CI: -80.262, -61.758; P = 0.047) (I² = 67.2%).
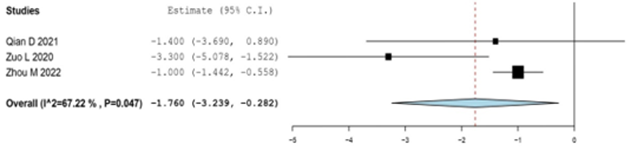
Only three studies reported changes in LVEF from the baseline (Figure 1B). Integrated analysis showed a significant change from baseline at one-year follow-up in patients who underwent PIMSRA (MD: -1.760; 95% CI: -3.239, -0.282; P = 0.047) (I² = 67.22%).
The pooled analysis from four studies that reported anterior IVS thickness showed no significant change from baseline (MD: -9.707; 95% CI: -10.819, -8.595; P = 0.095) (I² = 52.94%). Subgroup analyses based on follow-up revealed that there was no significant difference noted at 6 months (MD: -11.285; 95% CI; -12.825, -9.744; P= 0.933) (I² = 0%) or at one-year follow-up (MD: -9.147; 95% CI: -9.837, -8.456; P = 0.650) (I² = 0%) (Figure 1C).
The combined analysis of the four included studies reporting posterior IVS thickness showed no significant change from baseline (MD: -8.859; 95% CI: -10.073, -7.644; P = 0.119) (I² = 48.73%). Additionally, there was no significant difference noted in the subgroup analysis at 6 months (MD: -10.278; 95% CI; -12.133, -8.423; P = 0.934) (I² = 0%) and at one-year follow-up (MD: -8.335; 95% CI: -9.880, -6.789; P = 0.072) (I² = 69.14%) (Figure 1D).
This single-arm meta-analysis of 284 patients gathered from 5 clinical trials suggested that overall, after PIMSRA, LVOT gradient was reduced, and LVEF was slightly decreased. Additionally, no significant changes were observed in the anterior and posterior IVS thicknesses. Our results had substantial heterogeneity, which could be explained due to differences in the follow-up periods and studies with small sample sizes. It is important to note that even though no significant difference in follow-up was seen from the baseline at 6 months, there was indeed a significant difference noted at one year when assessing the outcomes of LVOT gradient. This could suggest that longer follow-up periods are imperative to truly observe the procedure's efficacy.
Our meta-analysis had some limitations. The number of studies and the sample size available for analysis was limited, and most patients were of Chinese origin. Furthermore, no studies have evaluated the long-term effects on cardiac conduction due to the scar tissue formed following ablation. Therefore, further studies with long-term follow-up having large sample sizes from different patient populations and ethnicities should be done to demonstrate the effectiveness of PIMSRA with more statistical power. Outcomes measuring procedure safety, such as intraoperative and postoperative complications, should also be recorded and compared with a control group.
| Included Studies | Year | Characteristics of Patients | Number of participants | Follow up | |||||
| Age in years | Gender | NYHA Class | LVOT Gradient | IVS Thickness | |||||
| Zhou M[1] | 2022 | 33 - 61 | M-125 F-75 | >50 mmHg | 200 | 1 year | |||
| Qian D [3] | 2021 | >50 mmHg | 15-25 mm | 30 | 1 year | ||||
| Zuo L [7] | 2020 | 15-79 | M-20 F-10 | Chest pain, syncope, NYHA Class Ⅲ/IV | >50 mmHg | 30 | 1 year | ||
| Liu L [6] | 2018 | 24 - 57 | M-13 F-2 | Chest pain, syncope, NYHA Class Ⅲ/IV | 15 | 6 months | |||
| Liu LW [8] | 2019 | Two NYHA class Ⅱ & Seven NYHA class Ⅲ cases | 9 | 6 months | |||||
Table 1: Characteristics of included studies
NYHA- New York Heart Association; LVOT- Left Ventricular Outflow Tract; IVS- Interventricular Septum.
Figure 1
Author Declarations
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Conflict of Interest: The authors have no relevant financial or non-financial interests to disclose.
Author Contribution: All authors had access to the data and a role in writing the manuscript. All authors have reviewed the manuscript and approved it in its current form.
Code Availability: Following PRISMA guidelines. Software used was Open Meta analyst.
Availability of data and material: Transparent.
Ethics approval: This is a review article(metanalysis). According to PRISMA no ethical approval is required.
Consent to participate: N/A
Consent to publish: N/A
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Supplementary Information
Search Strategy
"PIMSRA"[All Fields] OR (("percutaneous"[All Fields] OR "percutaneously"[All Fields] OR "percutanous"[All Fields]) AND ("intramyocardial"[All Fields] OR "intramyocardially"[All Fields]) AND ("septal"[All Fields] OR "septally"[All Fields] OR "septals"[All Fields]) AND ("radiofrequency ablation"[MeSH Terms] OR ("radiofrequency"[All Fields] AND "ablation"[All Fields]) OR "radiofrequency ablation"[All Fields])) OR ("Liwen"[All Fields] AND ("methods"[MeSH Terms] OR "methods"[All Fields] OR "procedure"[All Fields] OR "methods"[MeSH Subheading] OR "procedures"[All Fields] OR "procedural"[All Fields] OR "procedurally"[All Fields] OR "procedure s"[All Fields]).
Single arm study
P – Hypertrophic Cardiomyopathy; I – Intramyocardial Septal Radiofrequency Ablation; C – NA; O – Left Ventricular Outflow Gradient; Interventricular Septum Thickness (Anterior and Posterior); Left Ventricular Ejection Fraction (LVEF).
| Database | Strategy | Articles |
| Pubmed | "PIMSRA"[All Fields] OR (("percutaneous"[All Fields] OR "percutaneously"[All Fields] OR "percutanous"[All Fields]) AND ("intramyocardial"[All Fields] OR "intramyocardially"[All Fields]) AND ("septal"[All Fields] OR "septally"[All Fields] OR "septals"[All Fields]) AND ("radiofrequency ablation"[MeSH Terms] OR ("radiofrequency"[All Fields] AND "ablation"[All Fields]) OR "radiofrequency ablation"[All Fields])) OR ("Liwen"[All Fields] AND ("methods"[MeSH Terms] OR "methods"[All Fields] OR "procedure"[All Fields] OR "methods"[MeSH Subheading] OR "procedures"[All Fields] OR "procedural"[All Fields] OR "procedurally"[All Fields] OR "procedure s"[All Fields])) | 45 |
| Cochrane CENTRAL | ("PIMSRA" OR "Percutaneous Intramyocardial Septal Radiofrequency Ablation" OR "Liwen procedure") | 1 |
| SCOPUS | TITLE-ABS-KEY ((“PIMSRA” OR “Percutaneous Intramyocardial Septal Radiofrequency Ablation” OR “Liwen procedure”)) | 13 |
| Embase | ("PIMSRA" OR "Percutaneous Intramyocardial Septal Radiofrequency Ablation" OR "Liwen procedure") | 13 |
Raw Data
| Study ID | Sample size | Mean SD/Quartiles | ||||
| Baseline | 1 month | 3 months | 6 months | 1 year | ||
| Qian D 2021 | 30 | 82.45+-30.83 | N/A | N/A | N/A | 11.69+-5.5 |
| Zuo L 2020 | 30 | 95.0 (57.2) | 15.5(22.2) | 13(26) | 12(13.7) | 12.5(14.3) |
| Liu L 2018 | 15 | 88(66) | 14(8) | 13(6) | 11(6) | N/A |
| Zhou M 2022 | 200 | 79(53) | N/A | N/A | N/A | 14(24) |
| Liu LW 2019 | 9 | 83.3±32.4 | 26.8±19.6 | |||
LVOT (Left Ventricular Outflow Tract) Gradient
| Study ID | Sample size | Mean SD/Quartiles | ||||
| Baseline | 1 month | 3 months | 6 months | 1 year | ||
| Qian D 2021 | 30 | 68.95 ± 6.46 | 68.30 ± 6.54% | N/A | N/A | 67.55 ± 6.35% |
| Zuo L 2020 | 30 | 62.6 ± 5.5 | 62.0 ± 6.9 | 60.2 ± 5.2 | 60.2 ± 3.8 | 59.3 ± 4.2 |
| Liu L 2018 | 15 | N/A | N/A | N/A | N/A | N/A |
| Zhou M 2022 | 200 | 60.2 (4.7) | N/A | N/A | N/A | 59.2 (3.8) |
| Liu LW 2019 | 9 | N/A | N/A | N/A | N/A | N/A |
LVEF (Left Ventricular Ejection Fraction)
Anterior interventricular septum thickness
| Study ID | Sample size | Mean SD/Quartiles | ||||
| Baseline | 1 month | 3 months | 6 months | 1 year | ||
| Qian D 2021 | 30 | 22.03+-2.55 | N/A | N/A | N/A | 12.78+-1.95 |
| Zuo L 2020 | 30 | 23.3+-4.1 | 19.3+-2.9 | 16.6+-2.5 | 15+-2.7 | 14.4+-2.3 |
| Liu L 2018 | 15 | 25(21) | 20(17) | 16(14) | 14(12) | N/A |
| Zhou M 2022 | 200 | N/A | N/A | N/A | N/A | N/A |
| Liu LW 2019 | 9 | 24.7±2.7 | 13.4±2.0 | |||
Posterior interventricular septum thickness
| Study ID | Sample size | Mean SD/Quartiles | ||||
| Baseline | 1 month | 3 months | 6 months | 1 year | ||
| Qian D 2021 | 30 | 21.2+-2.36 | N/A | N/A | N/A | 12.2+-2.29 |
| Zuo L 2020 | 30 | 21.8+-4.9 | 18.5+-2.7 | 16+-3 | 14.9+-3 | 14.4+-1.9 |
| Liu L 2018 | 15 | 24(21) | 18(16) | 15(12) | 14(11.5) | N/A |
| Zhou M 2022 | 200 | N/A | N/A | N/A | N/A | N/A |
| Liu LW 2019 | 9 | 22.6±3.3 | 12.3±2.4 | |||
References
- Zhou M, Ta S, Hahn RT, Hsi DH, Leon MB. et al. (2022). Percutaneous Intramyocardial Septal Radiofrequency Ablation in Patients with Drug-Refractory Hypertrophic Obstructive Cardiomyopathy. JAMA Cardiol, 1;7(5):529-538.
Publisher | Google Scholor - Marian AJ, Braunwald E. (2017). Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy. Circ Res., 121(7):749-770.
Publisher | Google Scholor - Qian D, Zhou X, Liu H, Cao L. (2021). Clinical value of 2D speckle tracking imaging in evaluating the effect of percutaneous intramyocardial septal radiofrequency ablation in patients with hypertrophic obstructive cardiomyopathy. J Clin Ultrasound, 49(6):554-562.
Publisher | Google Scholor - Zhonghua Xin Xue Guan Bing Za Zhi. (2019). Efficacy and safety of transthoracic echocardiography-guided percutaneous intramyocardial septal radiofrequency ablation for the treatment of patients with obstructive hypertrophic cardiomyopathy. Chinese 24;47(4):284-290.
Publisher | Google Scholor - Tuohy CV, Kaul S, Song HK, Nazer B, Heitner SB. (2020). Hypertrophic cardiomyopathy: the future of treatment. Eur J Heart Fail, 22(2):228-240.
Publisher | Google Scholor - Burstein Waldman C, Owens A. (2021). A plain language summary of the EXPLORER-HCM study: mavacamten for obstructive hypertrophic cardiomyopathy. Future Cardiol. Oct;17(7):1269-1275.
Publisher | Google Scholor - Liu L, Li J, Zuo L, Zhang J, Zhou M. (2018). Percutaneous Intramyocardial Septal Radiofrequency Ablation for Hypertrophic Obstructive Cardiomyopathy. J Am Coll Cardiol, 2018 Oct 16;72(16):1898-1909.
Publisher | Google Scholor - Zuo L, Hsi DH, Zhang L, Zhang Q, Shao H. et al. (2020). Electrocardiographic QRS voltage amplitude improvement by intramyocardial radiofrequency ablation in patients with hypertrophic obstructive cardiomyopathy and one year follow up. J Electrocardiol, 61:164-169.
Publisher | Google Scholor - Liu LW, Zuo L, Zhou MY, Li J, Zhou XD et al. (2019). Efficacy and safety of transthoracic echocardiography-guided percutaneous intramyocardial septal radiofrequency ablation for the treatment of patients with obstructive hypertrophic cardiomyopathy. Chinese, 24;47(4):284-290.
Publisher | Google Scholor