Case Report
Minimally Invasive Lumbar Discectomy with Regional Anesthesia in A Patient At 6 Weeks of Gestation
- Piña R. Jorge Francisco *
- Buenrostro E. María Elena
- Dennis Valenzuela Jesús A
- Alaniz Sida Karmen K
- Chavira Calderon Larry
- Zermeño Díaz de León Paulina
- Vizcarra L. Andrea Natally
Universidad Autónoma De Baja California School of Medicine, Mexico.
*Corresponding Author: Piña R. Jorge Francisco, Universidad Autónoma De Baja California School of Medicine, Mexico.
Citation: Francisco PRJ, Elena BEM, Jesús DV, Karmen AS, Larry CC, et al. (2024). Minimally invasive lumbar discectomy with regional anesthesia in a patient at 6 weeks of gestation. Journal of Neuroscience and Neurological Research. BioRes Scientia Publishers. 3(2):1-6. DOI: 10.59657/2837-4843.brs.24.025
Copyright: © 2024 Piña R. Jorge Francisco, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 22, 2024 | Accepted: August 08, 2024 | Published: August 15, 2024
Abstract
We present the case of a 27-year-old female with a history of L4-L5 lumbar hernia accompanied by radiculopathy that is characterized by pain radiating to the right lower extremity with pain on a Visual Analogue Scale of 9/10 and muscle strength on a Daniels scale of 3/5. She went to the Neurosurgery service where she found a pregnancy at 6 weeks of gestation.
Patient without clinical improvement after conservative management and with progression of neurological motor deficit, so it was decided to perform neurosurgical intervention. Anesthetic management with regional anesthesia plus neuromonitoring using SedLine was decided as an alternative to general anesthesia due to the risk to the product. Management was carried out through the use of a combined subarachnoid block with a 15 mg dose of hyperbaric bupivacaine plus placement of an epidural catheter in the L1-L2 space. Later, the spinal erector block was performed in L4-L5 with 150 mg Ropivacaine without complications. Surgical procedure was performed without complications. Currently, the patient reports a VAS of 2/10, Daniels 5/5 with adequate use of gait and pregnancy of 8 SDG.
Keywords: anesthesia; pregnancy; neurosurgery; discectomy; regional anesthesia; spinal erector block; sedline
Introduction
There are few reports in the literature on spinal surgeries during pregnancy. 56% of women have low back pain during pregnancy. Lumbar disc herniation with features of nerve root compression is extremely rare, occurring in only approximately one in every 10,000 pregnancies; In most cases, the pathophysiological conditions resolve on their own after a few weeks or after delivery, thus avoiding the challenge of performing spine surgery in the prone position with the pregnant patient. On the other hand, more serious spinal conditions, such as cauda equina syndrome or any progressive neurological disease, will require urgent spinal surgery. Like intracranial tumors, preexisting spinal tumors may show accelerated growth and become symptomatic during pregnancy, justifying surgical intervention [1].
In 2016, the FDA (Food and Drug Administration) published that the use of general anesthesia and sedation in patients under 3 years of age and the obstetric population in the 3rd trimester could cause alterations in neurological development [2]. in addition to compromising organogenesis during the 1st trimester pregnancy, recommending the 2nd trimester as ideal for elective non-obstetric surgery; Neuraxial and/or regional anesthesia are considered safe during any trimester of pregnancy, being the most recommended anesthetic techniques for non-obstetric surgery with the aim of avoiding the use of anesthetic drugs associated with affection to the product. In addition to the anesthetic technique used, maintaining normotension and avoiding hypoxia and hypercapnia are critical objectives to achieve favorable outcomes for both the mother and the fetus [3].
Currently, the use of general anesthesia in pregnant patients continues to be avoided to prevent the complications described. In 2021, the British Journal of Anaesthesia published a meta-analysis that demonstrates the effects of general anesthesia during pregnancy on the neurocognitive development of the fetus in rodents. It was only possible to demonstrate that concentrations of inhaled anesthetics greater than 1 MAC or with surgeries greater than 3 hours during pregnancy were associated with some alteration in neurodevelopment, information prescribed by the FDA in 2016 [4].
Currently, the use of regional anesthesia has been increasing due to a decrease in intraoperative hypertension, tachycardia, and sedation and analgesia requirements during and postoperatively, respectively. Perez-Roman performed a meta-analysis of the use of regional anesthesia in lumbar spine surgery where this technique could offer benefits compared to general anesthesia, including duration of anesthesia, surgical times, total cost, and postoperative complications [5]. Ardaillon and collaborators created a guide for the general management of pregnant women with herniated discs. Through a review of cases, they found 17 patients managed surgically during pregnancy, of which 3 were administered regional anesthesia in the first trimester. They only reported minimal hypoesthesia in the postoperative follow-up with satisfactory pregnancy progression 17.
Based on these findings, it was decided to perform regional anesthesia in the following case.
Clinical case
Clinical case
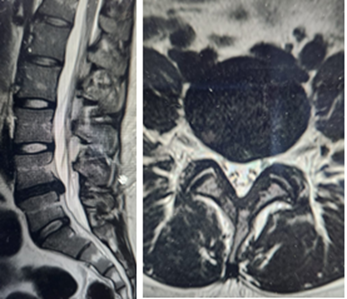
We have a 27-year-old female patient with no significant family history. He denies any personal pathological or gynecological or obstetric history. She reported the onset of low back pain 4 months ago, which increased until she reported a VAS score of 9/10, causing limitation in walking, which is why she went for evaluation with the Neurosurgery service. The physical examination revealed an alteration in mobility in the right lower extremity with a Daniels Scale of 3/5, and generalized deep tendon reflexes of 2++. Lumbar Magnetic Resonance was requested detecting lumbar hernia at the L4-L5 level, so a surgical protocol was initiated and in the preoperative laboratories a pregnancy of 8 weeks of gestation was observed (Figure 1).
Figure 1: Magnetic resonance imaging sagittal and axial sections respectively where a hernia can be seen at the lumbar level at L4-L5.
Neurosurgery recommends surgery once the pregnancy is over. A week later, the patient reported no improvement after conservative management, so it was decided to perform a minimally invasive lumbar discectomy.
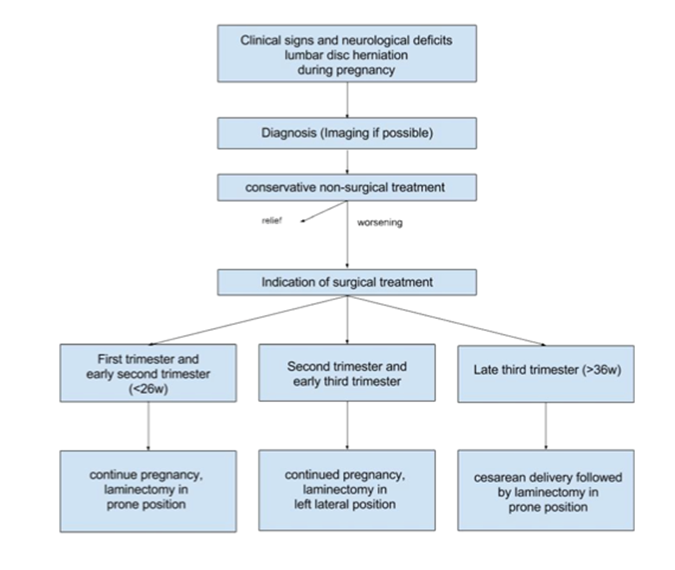
Table 1: Algorithm proposed by Ardailon et al for the management of patients with lumbar disc herniation during pregnancy [17].
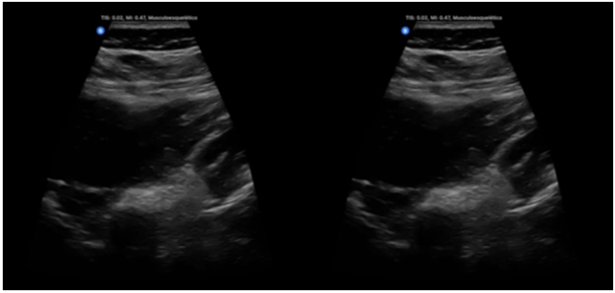
A subarachnoid block was performed at the L2-L3 level with administration of 15 mg hyperbaric bupivacaine using a 25 trans Touhy whitacre needle without complications, and a cephalic epidural catheter was left in place without alterations. Subsequently, ultrasound-guided spinal erector block was placed with Ropivacaine 3.75% bilaterally at the L4-L5 level without complications (Figure 2).
Figure 2: Performing spinal erector block placement
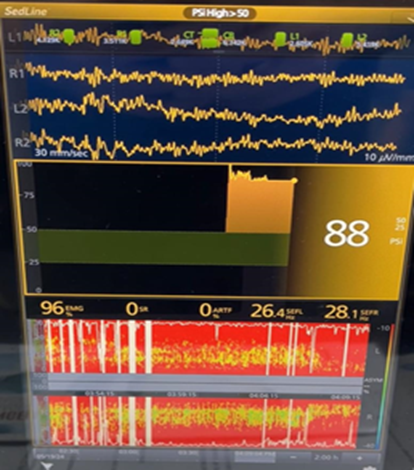
The patient was placed in a prone position, beginning the surgical procedure. As an adjuvant, dexmedetomidine was maintained in intravenous perfusion at a dose of 0.2-0.7 ug/kg/hr as well as Paracetamol 1 g and Ondansetron 8 mg. During the trans anesthetic, neuromonitoring was performed through SedLine, demonstrating SEF 95% with a predominance of gamma waves throughout the surgery (figure 3).
Figure 3: Monitoring under SedLine. The presence of Betta and Gamma waves can be observed, indicating that the patient is awake during the surgical procedure. The presence of SEFL and SEFR can be observed at 26.4 and 28.1 Hz respectively.
The patient remained normotensive throughout the surgery with mean arterial pressures between 80-90 mmHg. The neurosurgery service managed to successfully perform the surgical procedure and the patient recovered without complications. Immediate consultation was requested from the Gynecology service, which reported the presence of the product through ultrasound. The patient attended neurosurgery follow-up one week after the operation and a VAS score of 2/10 was reported, with improvement in the right lower extremity with a Daniels scale of 5/5 and complete recovery of walking.
Discussion
Ikonomidou was the first to report alterations in neurodevelopment after demonstrating neuronal apoptosis mediated by N-methyl-D-aspartate (NMDA) receptors for glutamate during the fetal and immediate postnatal stages, reporting that the inactivation of these receptors would be lethal for some neurons. in rats, affecting development and contributing to long-term neuropsychiatric disorders [6].
Other data from animal studies and in vitro investigations demonstrate that under experimental conditions, all general anesthetics tested, including NMDA receptor antagonists and gamma-aminobutyric acid (GABA) agonists, have immediate neuroanatomical consequences and functionally associated functional effects. chronic, if not permanent, in species ranging from roundworms to non-human primates. The only drugs in clinical use for sedation and anesthesia that do not cause neurodegeneration in animal models are dexmedetomidine and opioids [7]. Dexmedetomidine has been shown to protect against isoflurane-induced neuronal apoptosis and resulting cognitive impairments in young and adult animals; Furthermore, it is also reported that dexmedetomidine protects against propofol-induced neurodegeneration in developing rat brains, a protective effect that may be due to its inhibitory effect on neuronal gap junctions [8]. The disadvantage of these options is that both dexmedetomidine and opioids are not sufficient anesthetic agents to support general anesthesia and do not represent a feasible option on their own.
Similarly, Wuang H. and collaborators carried out an investigation in 48 pregnant rats divided into 3 study groups where 1.3% isoflurane was received for 3 hours (group 1), 2% isoflurane for 3 hours (group 2) and 50 % of O2 isolated in for 3 hours (control group. The pups were subjected to the Morris water maze on day 28 and day 90 after birth to evaluate learning and memory. The expression of the response element binding protein cAMP (CREB) and phosphorylated cAMP response element binding protein (p-CREB) were detected in the dentate gyrus of the hippocampus. It was found that fewer offspring of group 2 were able to cross the platform than those of the control group (. p less than 0.05) and, consequently, the pups of group 2 expressed p-CREB mainly in the subgranular zone in contrast to the entire granule cell layer of the dentate gyrus of the hippocampus as was detected in the pups of group 1 and the control group This information reinforces the fact that a higher concentration of inhaled anesthetic (isoflurane 2.0%) is associated with damage to spatial memory related to the inhibition of CREB phosphorylation in the granule cell layer of the dentate gyrus of the hippocampus [9].
On the other hand, Zuo Y.'s work group published the association of cognitive impairment with prenatal exposure to sevoflurane by causing iron deficiency and inhibiting myelinogenesis in animals [10].
In the case of intravenous anesthesia, Lin Z. and collaborators demonstrated that the offspring of pregnant rats exposed to propofol during the 3rd trimester of pregnancy had impaired learning and memory due to the inhibition of histone acetylation in the hippocampus, vital in participation in neurosynaptic plasticity [11]. Many limitations have been noted because all of these reviews were performed on animals.
Despite accumulating evidence from animal studies demonstrating that general anesthesia leads to neurodegeneration and cognitive impairment, a clear consensus on the impact of anesthetics in humans remains elusive to date. Several retrospectives have evaluated the potential risk of general anesthesia on the cognitive behavior of young children. A 2009 study by Wilder et al. used a cohort of 5,357 children aged four years or younger who received general anesthesia once or several times, compared to their untreated control cohort. In contrast, dexmedetomidine has been shown to protect against isoflurane-induced neuronal apoptosis and resulting cognitive impairments in young and adult animals. Furthermore, dexmedetomidine has also been shown to protect against propofol-induced neurodegeneration in developing rat brains. This protective effect may be due to an inhibitory effect of this compound on neuronal gap junctions [12].
A dose-dependent relationship was observed between the duration of exposure to the anesthetic and the frequency of learning difficulties, in addition to increasing the risk with subsequent exposures, demonstrating that those exposed to general anesthesia only once [1]. reinforcing the idea that an exposure A single, brief anesthesia may not be harmful.
The brains of children born prematurely or with cyanotic congenital heart disease may have been damaged by inflammation or chronic hypoxia before the children underwent surgery that required general anesthesia. Recently, interim analysis of the General Anesthesia vs. Spinal Anesthesia (GAS) study and the Pediatric Anesthesia and Neurodevelopment Assessment (PANDA) study, which involved formal neurodevelopmental testing, revealed in a brief analysis that single exposure to general anesthesia was not associated with worse outcomes in neurological development. [14, 15]. At present, there are no data specifically evaluating any association of in utero anesthetic exposure in human fetuses with postnatal neurodevelopmental outcomes.
Conclusion
The use of regional anesthesia in neurosurgery is a procedure that remains under study; Currently, the FDA maintains the recommendation to avoid the use of general anesthesia in pregnancy whenever possible and, if necessary, opt for this technique, the use of inhaled agents with MAC less than 1.0 and surgical times less than 3 hours would be the best option. widely recommended combination [16]. The review by Ardaillon reflects an adequate overview of how to approach pregnant patients with herniated discs; however, many studies are needed to establish anesthetic guidelines for non-obstetric surgical management in pregnant patients and, therefore, the anesthetic technique should selected according to other considerations based on the risk of low birth weight of the product, alterations associated with neurodevelopment, risk of preterm birth, risk of closure of the ductus arteriosus (associated with the use of NSAIDs), patient comorbidities, etc.
References
- Singh S, Sethi N. (2019). Neuroanesthesia and pregnancy: Uncharted waters. Med J Armed Forces India, 75(2):125-129.
Publisher | Google Scholor - FDA (2016). FDA Drug Safety Communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women.
Publisher | Google Scholor - E. Haggerty, J. Daly. (2021). Anaesthesia and non-obstetric surgery in pregnancy. BJA Educ, 21(2):42-43.
Publisher | Google Scholor - Bleeser T, Van Der Veeken L, Fieuws S, Devroe S, Van de Velde M, Deprest J, et al. (2021). Effects of general anaesthesia during pregnancy on neurocognitive development of the fetus: a systematic review and meta- analysis. Br J Anaesth, 126(6):1128-40.
Publisher | Google Scholor - Perez-RomanRJ, GovindarajanV, BryantJP, WangMY (2021). Spinalanesthesia in awake surgical procedures of the lumbar spine: a systematic review and meta-analysis of 3709 patients. Neurosurg Focus, 51(6):1-10.
Publisher | Google Scholor - Ikonomidou C, Bosch F, Miksa M, et al. (1999). Blockade of NMD Areceptors and apoptotic neurodegeneration in the devel- oping brain. Science, 283:70e4.
Publisher | Google Scholor - Sanders RD, Hassell J, Davidson AJ, Robertson NJ, Ma D. (2013). Impact of anaesthetics and surgery on neurodevelopment: an update. Br J Anaesth, 110:S 1:153--172.
Publisher | Google Scholor - BleeserT, Devroe T, Lucas N, Debels T, Van de Velde M, et al. (2023). Neurodevelopmental outcomes after prenatal exposure to anaesthesia for maternal surgery: a propensity-score weighted bidirectional cohort study. Anesthesia, 78(2):159-169.
Publisher | Google Scholor - Huan W, et. al. (2018). Influence of isoflurane exposure in pregnant rats on the learning and memory of offsprings. BMC Anesthesiol, 11;18(1):5.
Publisher | Google Scholor - Zuo Y, Chang Y, Thirupathi A, Zhou C, Shi Z. (2021). Prenatal sevoflurane exposure: Effects of iron metabolic dysfunction on offspring cognition and potential mechanism. Int J Dev Neurosci, 81(1):1-9.
Publisher | Google Scholor - Lin J, et. al. (2018). Propofol exposure during early gestation impairs learning and memory in rat offspring by inhibiting the acetylation of histone. Journal of Cellular and Molecular Medicine, 22(5):2600-2611.
Publisher | Google Scholor - Armstrong R, Xu F, Arora A, et al. (2017). General anesthetics and cytotoxicity: possible implications for brain health. Drug Chem Toxicol, 40(2):241-249.
Publisher | Google Scholor - Wilder RT, Flick RP, Sprung J, et al. (2009). Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology, 110:796-804.
Publisher | Google Scholor - Davidson AJ, Disma N, de Graaff JC, et al. (2016). Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lan- cet, 387:239-250.
Publisher | Google Scholor - Sun LS, Li G, Miller TL, et al. (2016). Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA, 315:2312-2320.
Publisher | Google Scholor - ACOG Committee Opinion No. 775: (2019). Nonobstetric Surgery During Pregnancy. Obstet Gynecol, 133(4):285-286.
Publisher | Google Scholor - Ardaillon H, Laviv Y, Arle JE, Kasper EM. (2018). Lumbar disk herniation during pregnancy: a review on general management and timing of surgery. Acta Neurochir (Wien), 160(7):1361-1370.
Publisher | Google Scholor