case report
Lower Eyelid Avulsion: A Case Report
- Vijay Bhatia 1*
- Deepanjali Kalra 2
- Manisha Singh 2
- Charmi Bodra 2
- Himadari Joshi 2
- Rajvee Gohil 2
- Jay Adeshra 2
1Professor and Head of Department of Burns and Plastic Surgery, Smt NHL Municipal Medical College, Gujarat, India.
2Residents, Smt. NHL Municipal medical college, Sardar Vallabhbhai Patel Institute of Medical Sciences and research, India.
*Corresponding Author: Vijay Bhatia,Professor and Head of Department of Burns and Plastic Surgery, Smt NHL Municipal Medical College, Gujarat, India.
Citation: Bhatia.V, Kalra. D, Singh.M, Bodra.C, Joshi. H et al. (2025). Lower Eyelid Avulsion: A Case Report. Journal of Surgical Case Reports and Reviews. Biores Scientia Publishers. 4(1):1-3. DOI: 10.59657/2993-1126.brs.25.026
Copyright: © 2025 Vijay Bhatia, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 12, 2024 | Accepted: January 28, 2025 | Published: January 07, 2025
Abstract
Introduction: The eyelids, the curtain of eyes the plays an important role in globe protection, lubrication and beautification. The chances of survival of eyelid avulsed flaps with a narrow pedicle is excellent as the arterial and venous blood supply is profuse.
Method: 35-year-old male patient with the avulsion injury to the right lower eyelid at the medial two third. The pedicle of the avulsed part based laterally. Injuries to the globe and lacrimal duct were ruled out. A decision was taken to wait for 48 hours and then to proceed with the surgery as by that time the dead and living tissues would be demarcated. Primary suturing was done in two layers.
Results: The avulsed pedicled flap survived well. The wound healed satisfactorily. Antibiotic ointment was applied to the eyes post operatively. The patient maintained a head-up position with administration of routine anti-inflammatory and antibiotics. The patient was discharged after 24 hours. Sutures were removed after 20 days and there were no epiphora or ectropion.
Conclusion: Knowledge of proper anatomy, systematic approach and appropriate armamentarium of techniques allows optimal surgical results. Simple reconstruction can provide excellent results, as in our case if it is done rightly and at the proper time.
Keywords: eyelid injury; avulsion; primary repair
Introduction
Eyelids are the curtain of eyes, the play an important role in global protection, lubrication. It gives beauty and shape to the face. A well-planned approach and knowledge of detailed anatomy for eyelid reconstruction is of the utmost importance for the best outcomes and decreasing the chances of post operative complications [1,2]. The eyelid comprises the anterior and posterior lamella. The anterior lamella includes orbicularis oculi and the skin while the posterior lamella is composed of the conjunctiva and tarsal plates. In between the two lamella is the grey line. Meibomian gland opening is present posterior to these glands. The skin over the eyelid is extremely thin, overlying very lax subcutaneous tissue. The lower eyelid comprises of the anterior lamella containing the orbicularis oculi muscle and skin whereas the posterior lamella containing the inferior tarsal muscle and the capsulopalpaebral fascia, tarsus and the orbital septum [3,4]. The blood supply to the lower eyelid and cheek area is by facial, angular, infraorbital, zygomatic-orbital, transverse facial terminal branches of external carotid artery and the superficial temporal artery and nerve supply is mainly by the infraorbital nerve, branch of the Trigeminal nerve. The chances of survival of eyelid avulsed flaps with a narrow pedicle is excellent as the arterial and venous blood supply is profuse. Here we present a case report presented to us with medial two third lower eyelid traumatic avulsion underwent primary repair of the avulsed flap after 48 hours.
case
Patient presented to our department 24 hours after the trauma aged 35 years. While he was working in tube light repair in a hotel, a steel wire got hooked accidentally in the right lower medial eyelid and avulsed the medial two third portion of the eyelid. There was an avulsion of the right lower eyelid over the medial two third part which was attached to the lower eyelid as a laterally based pedicled flap. The patient was admitted. General routine blood and radiological investigations were done. The 3D CT face reveals normal results. Vision and fundus were normal. Injuries to the globe and lacrimal duct were ruled out. A decision was taken to wait for 48 hours as by that time the dead and living tissues would be demarcating. The avulsed portion of the medial 2/3rd lower eyelid flap remained viable even after 48 hours. Preoperatively injectable Augmentin was given. The patient was taken in operation theatre. Under general anaesthesia, parts are painted and draped. Primary suturing was done in two layers. The posterior lamella was sutured using prolene 5-0 in a simple interrupted manner, burring the knot outside, followed by suturing of the anterior lamella with 5-0 prolene in a simple interrupted manner with edges everted and lash line in alignment.
Results
Avulsed pedicled flap survived well. Wound healed satisfactorily. Antibiotic ointment was applied to the eyes post operatively patient maintained head up position with administration of routine ant inflammatory and antibiotics. Patient was discharged after 24 hours. Sutures were removed after 20 days and there was no epiphora and ectropion.
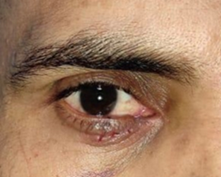
Figure 1: Preoperative picture of medial 2/3 lower eyelid avulsion
Figure 2: Post operative picture at POD 1
Figure 3: Postoperative picture of lower eyelid repair after suture removal
Discussion
The goal of eyelid reconstruction is restoration of form and function, while minimizing surgical morbidity. [5,6,7,8] There are various methods to close the lower eyelid defects well described in literature, which range from direct closure to Hughes tars conjunctival flap and mustard cheek flap. The advancement, rotation flaps and skin and mucosa grafting remain the mainstay for eyelid reconstruction [9]. The decision of the reconstruction will take into account of the defect, ranging from small (20%) to large defect (50%), location of defect, medial and lateral canthus involvement, lacrimal drainage system involvement, age of the patient, condition of the opposite eyelid and laxity of the surrounding tissue. A well-planned approach always gives optimum surgical results and minimizes complication rates. Global injuries must be ruled out before proceeding with the reconstruction. Thorough examination of the eye must be done and injuries to lacrimal duct and canthal tendons should be noted. In our case, patient presented with right lower medial two third eyelid avulsions due to the hook of the rod The medial canthus with lacrimal duct system was intact, and global injury was ruled out prior to reconstruction. After deliberately waiting for 48 hours, primary suturing of the lower eyelid avulsed flap was done in 2 layers. Flap survived well and post operatively no epiphora and ectropion were present in the postoperative period. It usually takes 48 hours for the demarcation of the dead tissue. Hence, patients waiting for this time usually saves patients from a greater number of procedures. Once a clear line of demarcation is present, it is easy to assess the level of debridement and save the patient from repeated surgery. In our case, and avulsed flap survived well and no blackening, skin colour changes was noted. Minimal debridement in the form of trimming of the edges was done with primary suturing. The wound healed satisfactorily well with no epiphora or ectropion.
Conclusion
Knowledge of proper anatomy, systematic approach and appropriate armamentarium of techniques allows optimal surgical results. Timing of repair is important with the type of reconstruction. Waiting for demarcation of the dead and live tissues saves patients from repeated surgery. An old school thought, simplicity is the ultimate sophistication. Simple reconstruction can provide excellent results, as in our case if it is done rightly and at the proper time.
Declarations
Author Contributions
Vijay Bhatia. is the chief surgeon in our study who has performed the operations. Deepanjali Kalra wrote the manuscript. Manisha. Singh., Charmi Borda, Himadri Joshi, Rajvee Gohil, and Jay Aesha has assisted in operation
Conflicts of Interest
The authors declare that there are no relevant conflicts of interest.
Sources of Funding
NIL
Acknowledgements
NIL
Consent to Participate
Identity of the patient is not revealed in any of images hence it is not applicable
Consent for Publication
Identity of the patient is not revealed in any of images hence it is not applicable
References
-
-->