Case Report
Large Concha Bullosa Mucocele: A Case Report
- Hisham Almutawa *
- Aqeel Aloqaili
- Nasser Abdulaziz Alwehaibi
- Alhanouf AlQabbani
- Abdulrahman Alhumaizi
Otolaryngology-Head and Neck Surgery, King Abdulla Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia.
*Corresponding Author: Hisham Almutawa,Otolaryngology-Head and Neck Surgery, King Abdulla Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia.
Citation: H. Almutawa, A. Aloqaili, Nasser A. Alwehaibi, A. Al-Qabbani, A. Alhumaizi. (2024). Large Concha Bullosa Mucocele: A Case Report. Journal of Surgical Case Reports and Reviews. BioRes Scientia Publishers. 2(2):1-4. DOI: 10.59657/2993-1126.brs.24.0018
Copyright: © 2024 Hisham Almutawa, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 07, 2024 | Accepted: February 19, 2024 | Published: February 24, 2024
Abstract
Concha bullosa is the pneumatization of a nasal turbinate, most commonly occurring in the middle turbinate. This represents a prevalent sinonasal variation. While typically asymptomatic, it has the potential to mimic other conditions, including chronic rhinosinusitis, fungal sinusitis, and nasal masses, and may even coexist with orbital or skull base extensions. This study presents a case involving a mucocele within a concha bullosa located in the unilateral middle turbinate, initially manifesting as a nasal mass.
Keywords: concha bullosa; concha bullosa mucocele; middle turbinate mucocele
Introduction
Concha bullosa (CB) is one of the most prevalent sinonasal anatomical anomalies. It is characterized by an abnormal pneumatization of the middle turbinate bone, either unilateral or bilateral. This pneumatization can stem from the pneumatic expansion of anterior ethmoid cells or, less commonly, posterior cells. CB is categorized based on its location and extension into three types: "lamellar CB" involving the turbinate's lamellar portion, "bulbous CB" limited to the bulbous portion of the turbinate bone, and "extensive CB" which encompasses both the lamellar and bulbous portions [1]. CB often remains asymptomatic, often appearing as an incidental discovery on computed tomography (CT) scans [2]. However, in rare cases, CB can lead to a mucocele that induces excessive expansion and obstruction within the osteomeatal complex. This case report details a notable instance of CB mucocele, classified as a unilateral nasal mass.
Case Presentation
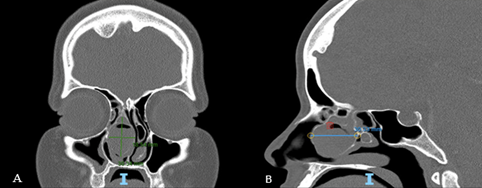
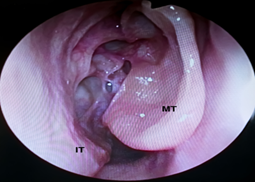
A 29-year-old previously healthy woman presented to a rhinology clinic with a two-year history of progressive, continuous right-sided nasal obstruction. Accompanying symptoms included thick nasal discharge on the right side and frontal headaches. Visual acuity and diplopia remained unchanged. The patient had employed intranasal corticosteroids and normal saline nasal rinses, yielding unsatisfactory improvement. Upon endoscopic nasal examination, a sizable mass was observed on the right side, occupying the middle meatus and extending inferiorly medial to the inferior turbinate. The right middle meatus exhibited purulent discharge due to the mass. Palpation using a Frazier suction indicated a firm origin from the middle turbinate. The left nasal cavity displayed patent characteristics with a superiorly deviated nasal septum. A contrast-enhanced CT scan of the paranasal sinuses unveiled a polypoidal soft tissue density within the expanded right CB. Complete occlusion of the right osteomeatal complex alongside mucosal thickening in the maxillary, anterior ethmoidal, and posterior ethmoidal regions was evident. The nasal septum experienced superior displacement due to the mass on the left side. Measurements of the CB were approximately 30.3 mm craniocaudally, 18.5 mm medial to lateral, and 30.3 mm anterior to posterior. Based on clinical and radiological evaluations, a diagnosis of right-sided CB mucocele was determined. The patient underwent limited functional endoscopic sinus surgery and CB resection under general anesthesia. Postoperative clinic visits documented significant symptom improvement, with endoscopic examination displaying healed surgical sites and normal mucosa.
Discussion
CB signifies the pneumatization of nasal turbinates, a common variant of nasal anatomy. It can manifest in the superior, middle, or inferior turbinate, with the middle turbinate variant being particularly frequent [1,3,4]. Prevalence rates for middle turbinate concha bullosa (MTCB) range from 11.5% to 73%, and within the Saudi population, it's reported at 55.5% [5]. MTCB subtypes include lamellar, bulbous, or extensive CB [1]. Massive MTCB can lead to ipsilateral sinusitis, while CB mucocele can develop within, affecting all age groups (pediatric, adolescence, and adult). [6,7,8,9]. A rare case of CB pyocele in a 25-year-old male has also been documented [9]. Fungal infections in MTCB have been reported with various presentations, including incidental findings, headaches, and symptoms resembling chronic rhinosinusitis [10,11,12]. Alromaih et al. reported a case of fungal infection in MTCB that mimicked a bony tumor lesion [2]. They noted that CB has also been documented in both the superior and inferior turbinates. Homsioglou et al. reported a case of superior turbinate CB causing headaches with minimal nasal symptoms [13]. Alkhaldi et al. reported two cases of unilateral inferior turbinate CB where symptoms improved with medical management alone [3]. Other reports described unilateral and bilateral inferior turbinate CB that did not respond to medical therapy but showed positive outcomes with surgical management [4,14]. In the bilateral inferior tubinates CB case report, interestingly, the left inferior turbinate featured two conchae, one communicating with the natural ostium of the ipsilateral maxillary sinus [14]. In this study, a patient presented with unilateral maxillary sinusitis but no extension to the orbital or skull base areas. Intra-operatively, a mucocele was identified, and no pus was observed in the CB. During the postoperative follow-up period, the patient remained asymptomatic with no evidence of recurrence.
Figure 1: CT scan of the paranasal sinuses coronal (A) and sagittal (B) sections showing a larger concha bullosa 30.3 × 30.3 × 18.5 mm with soft tissue density contents.
Figure 2: Postoperative endoscopic view of the right nasal cavity showing healed mucosa. IT: inferior turbinate. MT: middle turbinate.
Conclusion
CB constitutes a natural variance in paranasal sinus pneumatization. However, the extent of pneumatization can contribute to a spectrum of sinonasal pathologies, ranging from nasal obstruction to sinus drainage obstruction. Recognizing that CB can manifest as a nasal mass underscores the necessity of pre-operative imaging. Given the middle turbinate's connection to the skull base, inadvertent manipulation of CB as a simple nasal mass can result in adverse outcomes, such as skull base trauma and cerebrospinal fluid leakage.
Conflict of Interest Statement
The authors declare no conflicts of interest.
References
- Bolger, W. E., David S. Parsons & Clifford A. Butzin. (1991). Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope, 101:56-64.
Publisher | Google Scholor - Alromaih, S. R., Aloraini, N. S. & Alqaryan, S. K. (2021). Huge Concha Bullosa Involved with Allergic Fungal Sinusitis and Mimicking a Bony Tumor.
Publisher | Google Scholor - Alkhaldi, A. S., Alhedaithy, R. & Alghonaim, Y. (2021). Concha Bullosa of the Inferior Turbinate: Report of Two Cases.
Publisher | Google Scholor - Pittore, B., Al Safi, W. & Jarvis, S. J. (2011). Concha bullosa of the inferior turbinate: an unusual cause of nasal obstruction Concha bullosa del turbinato inferiore: inusuale causa di ostruzione nasale, 31.
Publisher | Google Scholor - El-Din, W. A. N., Madani, G. A., Fattah, I. O. A., Mahmoud, E. & Essawy, A. S. (2021). Prevalence of the Anatomical Variations of Concha Bullosa and its Relation with Sinusitis Among Saudi Population: A Computed Tomography Scan Study. Anat Cell Biol, 54:193-201.
Publisher | Google Scholor - Lee, J. S., Ko, I. J., Kang, H. D. & Lee, H. S. (2008). Massive Concha Bullosa with Secondary Maxillary Sinusitis. Clin Exp Otorhinolaryngol, 1:221.
Publisher | Google Scholor - Aslan, G., Ugur, M. B. & Başsüllü, N. (2013). Giant mucocele originating from the middle concha in a 5-year-old child: A case report. J Med Case Rep, 7.
Publisher | Google Scholor - Abdel-Aziz, M. (2011). Mucopyocele of the Concha Bullosa Presenting as a Large Nasal Mass. J Craniofac Surg, 22:1141-1142.
Publisher | Google Scholor - Okuyucu, Ş., Akoǧlu, E. & Daǧli, A. Ş. (2008). Concha bullosa pyocele. European Archives of Oto-Rhino-Laryngology, 265:373-375 (2008).
Publisher | Google Scholor - Spatola, A. et al. (2022). Fungal ball in concha bullosa as incidentaloma: A case report and the review of the literature. Radiol Case Rep, 17:997-1001.
Publisher | Google Scholor - Bulut, F. & Kazikdas, K. C. (2018). An unusual case of headache: Isolated fungus ball in Concha bullosa. Journal of Craniofacial Surgery, 29: e551–e552.
Publisher | Google Scholor - Balasubramaniam, G. K., Thirunavukarasu, R., Kalyanasundaram, R. B. & Narendran, G. (2014). An Unusual Presentation of Fungal Mass in Concha Bullosa. International Journal of Otolaryngology and Head & Neck Surgery, 03:263-266.
Publisher | Google Scholor - Homsioglou, E. et al. (2007). Pneumatized superior turbinate as a cause of headache. Head Face Med 3.
Publisher | Google Scholor - Koo, S. K., Moon, J. S., Jung, S. H. & Mun, M. J. (2018). A case of bilateral inferior concha bullosa connecting to maxillary sinus. Braz J Otorhinolaryngol 84, 526-528.
Publisher | Google Scholor