Review Article
Juvenile Diabetes
1Department of Chemistry, Sri J.N.M.PG College, Lucknow UP, India.
2Department of Chemistry, Dayanand Girls PG Kanpur, UP, India.
*Corresponding Author: D.K. Awasthi, Department of Chemistry, Sri J.N.M.PG College, Lucknow UP, India.
Citation: D.K. Awasthi, Dixit A. (2023). Juvenile Diabetes. Clinical and Laboratory Research, BioRes Scientia Publishers. 1(1); DOI: 10.59657/clr.brs.23.008
Copyright: © 2023 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 17, 2023 | Accepted: July 31, 2023 | Published: August 07, 2023
Abstract
Diabetes is a condition in which the body can't make enough insulin, or can't use insulin normally. Type 1 diabetes is an autoimmune disorder. The body's immune system damages the cells in the pancreas that make insulin. Insulin is a hormone. It helps sugar (glucose) in the blood get into cells of the body to be used as fuel. When glucose can’t enter the cells, it builds up in the blood. This is called high blood sugar (hyperglycaemia). High blood sugar can cause problems all over the body. It can damage blood vessels and nerves. It can harm the eyes, kidneys, and heart. It can also cause symptoms such as tiredness.
Keywords: juvenile diabetes; glucose; blood test; urine test
Introduction
Juvenile diabetes is mostly an autoimmune disorder and is also referred to as type 1 diabetes As the name suggests, the disease is commonly diagnosed in childhood or adolescence (as opposed to type 2 or “adult-onset” diabetes, which occurs most often in middle age). In truth though, juvenile/type 1 diabetes doesn’t only happen in kids—it’s possible, though less common, for adults to get it, too. Similarly, children can and sometimes do get type 2. According to the most recent figure, about 283,000 kids and teens have diabetes; approximately 244,000 of those cases are juvenile diabetes. People with all types of diabetes share one thing in common: High amounts of sugar, or glucose, in their blood.
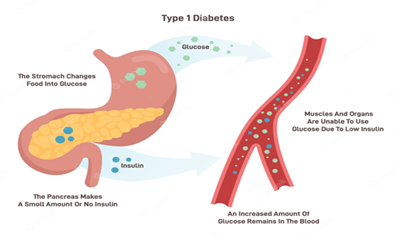
How Glucose Works
After you eat, your body breaks down the food into glucose (a.k.a. sugar) and other substances, which then enter the bloodstream. In response, your pancreas releases insulin, a type of hormone that helps muscle and fat cells suck up the glucose and use it for energy. But in kids with juvenile diabetes, the body’s immune system gets confused and starts attacking the beta cells in the pancreas that make insulin, shutting down production. Without insulin to help guide glucose into the body's cells, sugar starts to build up in the bloodstream, leading to a host of health issues.
Who Gets Juvenile Diabetes?
About 37.3 million people in the United States have been diagnosed with diabetes, and 5% to 10% of those cases are juvenile (type 1). That works out to about one in 250 people; of those, about three-quarters are diagnosed with juvenile diabetes during childhood or young adulthood. The most common age for a juvenile diabetes diagnosis is between 10 and 16, possibly because puberty triggers an increase in hormone production and these hormones, including oestrogen and testosterone can affect blood sugar levels.
Possible factors that play a role in the development of the disease:
Ethnicity and geography: Juvenile diabetes becomes more common the further away you live from the equator. For instance, children in Scandinavian countries have a much higher risk of being diagnosed with the disease. And Caucasians of Northern European ancestry have a higher risk than other ethnicities.
Genetics: Although there is no juvenile diabetes “gene,” there are several genes and mutations that have been identified as increasing your risk for it. In particular, mutations in the human leukocyte antigen (HLA) class of genes, which are related to the immune system, can raise the risk of autoimmune conditions like juvenile diabetes.
Family history: If autoimmune conditions run in your family, that means your child is at higher risk of developing one, too. Some studies suggest that if a sibling or parent has type 1 diabetes, kids have a 15 times higher risk of developing the condition than someone without any family history.
Toxins and infections: Doctors believe that in most cases, a toxin or virus triggers the start of juvenile diabetes. This “foreign invader” kicks the immune system into gear, causing it to mistakenly attack the pancreas and kill off insulin-producing beta cells.
Tests for Juvenile Diabetes: The first step in getting a diabetes diagnosis is a blood test to look for elevated glucose levels. If your child is diagnosed with high blood sugar, then the doctor will want to perform additional tests to identify the specific type of diabetes. Correct diagnosis is very important since treatment is different for each type. Your child may need one or more of the below:
Blood Tests
A1C (or glycated hemoglobin) test: This test measures what percentage of red blood cells have been coated with glucose over the past two to three months and is the most common test for diabetes. The higher a child’s blood sugar, the higher his score. An A1C result below 5.7 is considered normal; 5.7 to 6.4 is prediabetic; 6.5 or above suggests diabetes.
Fasting blood sugar test: Blood will be drawn first thing in the morning before your child eats or drinks anything other than water. A result under 100 milligrams per deciliter is normal; 100 to 125 mg/dL is prediabetic; 126 mg/dL indicates diabetes. The doctor will likely want to do the test twice before officially diagnosing your child.
Random blood sugar test: Blood is drawn at any time of day, whether your child has eaten recently or not. A result of 200 mg/dL indicates diabetes.
Antibody test: To help differentiate between juvenile diabetes and other types, a doctor may also want to draw blood for an “autoantibody” test. This test will show if your child’s immune system is attacking the pancreas. Kids with juvenile diabetes often test positive for several specific autoantibodies, while those with type 2 don’t.
Urine Test
Your child’s doctor may want to test his urine for ketones. The test can generally be done at home or in a doctor’s office by peeing into a specimen cup. If you’re doing the test at home, it will come with paper test strips to dip into the urine. Extremely high levels of ketones are a sign of ketoacidosis, a potentially fatal complication of diabetes that requires immediate treatment.
Treatment
Treatment for Juvenile Diabetes
All children with juvenile diabetes need to regularly check their blood glucose levels,take insulin daily, and be mindful of what they eat—not because diet can cure juvenile diabetes (it can’t), but because large meals or those high in carbohydrates rely on high doses of insulin to manage blood sugar levels, and your child’s body isn't able to produce that insulin.
Checking Glucose Levels
Kids with juvenile diabetes may need to check (or have someone help check) their blood glucose four to 10 times a day in order to make decisions about insulin dosages, food, and exercise choices. This can be done with a home glucose meter. To use it, the child’s fingertip is pricked with a specialized lancet “pen,” then blood is dropped onto a test strip in the meter. In some cases, a doctor might suggest a continuous glucose monitor, a tiny sensor that is inserted under the skin of the abdomen, arms, or thigh to check glucose levels regularly. The sensor will alert your child if levels fall too low.
Taking Insulin
Insulin, which people with juvenile diabetes need daily, can’t be taken as a pill because it would be broken down and digested before getting into your blood.
There are a couple of different ways insulin can be delivered to the body:
Injection: This is the most common way to take insulin. Your child (or someone helping him) will use a syringe or “pen” to inject the drug, usually in the belly, upper arm, thigh, or butt. Kids may need four or more injections a day.
Insulin Pump: Children who need multiple injections per day or are high risk of ketoacidosis may prefer an insulin pump, which automatically delivers insulin throughout the day through a tiny catheter that’s worn on the body.
Insulin Types
The type of insulin your child take depends on several factors, including how long it takes the body to absorb insulin; your child’s diet and exercise habits; and tolerance for injections. A pediatrician will help determine what’s best for your child. These are the common options:
Rapid-Acting Insulin: This medication starts to work within about 15 minutes of taking it (often just before a meal to prevent blood glucose from rising). It works for two to four hours. Examples include Humalog (lispro) and Novolog (aspart).
Short-Acting Insulin: Also called “regular” insulin, this med takes about 30 minutes to kick in. It is taken before a meal to help lower increased levels of blood sugar while eating. It works for three to six hours. Examples include Humulin R and Novolin R.
Intermediate-Acting Insulin: Often combined with rapid-acting insulin, this med starts working about two to four hours after taking and balances the body’s glucose levels for 12 to 18 hours. Examples include Humulin N and Novolin N (NPH).
Long-Acting Insulin: These meds can take up to six hours to reach the bloodstream. They work to maintain lower blood sugar levels for up to 26 hours. Examples include Lantus (insulin glargine) and Levemir (insulin detemir).
Ultra-long-acting Insulin: Reaches the blood stream in 6 hours, does not peak, and lasts about 36 hours or longer. Examples include Degludec (Tresiba), Glargine u-300 (Toujeo).
Living With
Type 1 diabetes, also called juvenile diabetes, occurs when the body’s immune system destroys cells in the pancreas that create insulin. Insulin is a hormone that takes sugar (known as glucose) from your bloodstream and delivers it into your cells to be used for energy. Without insulin, your blood sugar levels remain high -- which can lead to serious health complications over time. Because their bodies don’t make insulin, children with Type 1 diabetes must get insulin from multiple daily injections or an insulin pump. They also must test their blood sugar levels throughout the day and pay special attention to eating, drinking, and exercising. Managing your child’s Type 1 diabetes can sometimes seem overwhelming. The Duke Children’s diabetes care team can help you overcome these challenges. We offer expert medical guidance and give you and your child information, support, and encouragement to manage and live well with diabetes.
Type 1 diabetes is a life-threatening, life-long disease that is characterized by the lack of insulin, causing excessively elevated glucose in a person's blood (called hyperglycemia). Type 1 diabetes is the most common form of diabetes in childhood. About 1 in every 350 children in the United States has type 1 diabetes. It can appear in children as young as 6 months of age, although the most common age is around 12. Type 1 diabetes is becoming more frequent than before, particularly among children younger than 5 years of age. Adults can also develop type 1 diabetes.
Around 95% of cases of type 1 diabetes are caused by autoimmunity, that is, the body's defense system (called immune system) attacking its own cells, in this case, the insulin-producing cells in the pancreas (beta-cells). The ultimate reason for this attack is unknown. However, we know that there are inherited (genetic) and environmental factors. Relatives of a patient with type 1 diabetes have increased risk of developing the disease: about 70% for identical twins, 6% of siblings and non-identical twins, 6% for children of a father with type 1 diabetes and 4% for a mother with type 1 diabetes. Certain genes (HLA types) make type 1 diabetes more likely. addition to genes and family history. Research studies are ongoing with the ultimate goal of finding safe and effective treatments to prevent to type 1 diabetes in individuals at risk. Type 1 diabetes mellitus is a long-term (chronic) condition. It may start at any age. Insulin from the pancreas must be replaced with insulin injections or an insulin pump.
There are two forms of type 1 diabetes:
Immune-mediated diabetes. This is an autoimmune disorder in which the body's immune system damages the cells in the pancreas that make insulin. This is the most common kind of type 1 diabetes.
Idiopathic type 1. This refers to rare forms of the disease with no known cause.
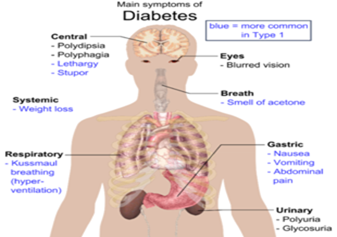
Symptoms & Types
Symptoms of diabetes include increased urination (caused by the kidneys flushing excessive blood glucose), increased thirst (the body's compensatory mechanism of the fluid loss through urine) and weight loss (caused by the loss of glucose through the kidneys, among other factors). Other symptoms include tiredness and mood changes, bedwetting (consequence of increased urination), blurry vision and infections (skin, urine, vaginal). If left untreated, increased glucose levels lead to additional complications, such as diabetic ketoacidosis (DKA), which is life-threatening. At this stage, patients have nausea, vomiting, abdominal pain and abnormal breathing followed by loss of consciousness and potentially death. Early diagnosis of type 1 diabetes is critical to prevent development of this fatal complication. Type 1 diabetes often appears suddenly. In children, type 1 diabetes symptoms may be like flu symptoms. Symptoms can occur a bit differently in each child. They can include:
- High levels of glucose in the blood and urine when tested.
- Unusual thirst.
- Dehydration.
- Frequent urination (a baby may need more diaper changes, or a toilet-trained child may start wetting his or her pants).
- Extreme hunger but weight loss.
- Loss of appetite in younger children.
- Blurred vision.
- Nausea and vomiting.
- Belly (abdominal) pain.
- Irritability and mood changes.
- Serious diaper rash that does get better with treatment.
- Fruity breath and fast breathing.
Yeast infection in girls.
Diagnosis & Tests
Diagnosis of type 1 diabetes requires a test of blood glucose. Patients with clearly elevated glucose in blood will also have glucose in their urine; however, glucose in urine can be normal at certain times of the day and therefore a normal urine test does not rule out diabetes. At the early stages of diabetes, blood glucose can be normal at certain times of the day, and a special test called oral glucose tolerance test (OGTT), which is done by measuring blood glucose 2 hours after drinking a glucose load may be necessary to demonstrate that someone has diabetes. Once a patient is diagnosed with diabetes, several tests are conducted to diagnose the type of diabetes (for example, diabetes autoantibodies are typical of type 1 diabetes) and the presence of complications (for example, DKA) and other conditions that are present more frequently (for example, thyroid abnormalities). To diagnose risk of type 1 diabetes, islet autoantibodies are measured in blood. Genetic tests and measurement of the ability to produce insulin help better estimate the risk and establish the stage of the progression.
Fasting plasma glucose: The blood is tested after at least 8 hours of not eating.
Random plasma glucose: The blood is tested when there are symptoms of increased thirst, urination, and hunger.
Children with type 1 diabetes must have daily injections of insulin to keep the blood glucose level within normal ranges. Insulin is given either by injection or insulin pump. Your child’s healthcare provider will show you how to give your child insulin with either method.
Treatment will also include:
Eating the right foods to manage blood glucose levels. This includes timing meals and counting carbohydrates.
Exercise, to lower blood sugar.
Regular blood testing to check blood-glucose levels.
Regular urine testing to check ketone levels.
Type 1 diabetes can cause
Ketoacidosis: This is when blood sugar levels are very high and the body starts making ketones. This is a very serious condition that needs to be treated right away in the hospital, sometimes in the intensive care unit. If your child is not treated right away, they are at risk for diabetic coma. A child with a diabetic coma loses consciousness because of brain swelling. The brain swells because of the very high blood sugar levels.
Low blood sugar (hypoglycaemia): This is also sometimes called an insulin reaction. This occurs when blood glucose drops too low.
Your child’s healthcare provider will tell you how to avoid these problems.
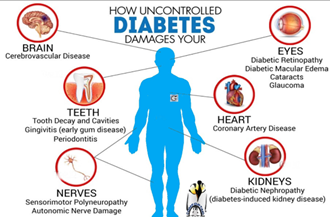
Over time, high blood sugar levels can damage blood vessels. Balancing insulin, diet, and activity can help keep blood sugar levels in the target range and help prevent complications such as:
Eye problems, Kidney disease, Nerve damage, Tooth and gum problems, Skin and foot problems, Heart and blood vessel disease.
Treatment & Care
Treatment & Care
Type 1 diabetes requires treatment with insulin. Today, insulin must be delivered via injection (usually, intravenous in the hospital setting and subcutaneous at home), pump (a device that delivers insulin subcutaneously in a continuous fashion) and, recently, inhaled. To give the right dose of insulin, patients check their blood glucose several times daily. Some patients also wear a continuous glucose monitor that provides additional information.
Children with type 1 diabetes need to have frequent adjustments of the dose and require visits to their diabetes doctor and team (diabetes educator, dietitian and psychologist) every 3 months. It is very important to screen for potential complications (eye, kidney and cardiovascular diseases, depression, eating disorders, obesity, etc.) as well as other autoimmune conditions (thyroid and celiac diseases among others). Screening and early treatment help decrease the risk of complications. Patients with well controlled type 1 diabetes can lead normal lives.
Conclusion
Type 1 diabetes mellitus is a long-term (chronic) condition. It may start at any age. Only 5% of people with diabetes have type 1, Type 1 diabetes is a condition in which blood glucose levels are abnormally high. It is most frequently caused by an autoimmune disorder in which the body's immune system destroys the cells in the pancreas that produce insulin. Children with type 1 diabetes must have daily injections of insulin to keep the blood glucose level within normal ranges. Without insulin, blood glucose levels continue to rise and death will occur. With the administration of insulin, and other management activities, children with type 1 diabetes can lead active, healthy lives.
References
- Lucier J, Weinstock RS, Doerr C. (2021). Diabetes Mellitus Type 1 (Nursing).
Publisher | Google Scholor - Goodman CC, Snyder TEK. (2013). Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier, 425-432.
Publisher | Google Scholor - (2021). Diabetes SA Diabetes type 1
Publisher | Google Scholor - (2016). American Diabetes Association. Type 1 Diabetes.
Publisher | Google Scholor - (2021). Diabetes aus.
Publisher | Google Scholor - Franc S, et al. I (2016). Insulin-based strategies to prevent hypoglycaemia during and after exercise in adult patients with type 1 diabetes on pump therapy: the DIABRASPORT randomized study. Diabetes, Obesity, and Metabolism.
Publisher | Google Scholor - Alarcón-Gómez J, Chulvi-Medrano I, Martin-Rivera F, Calatayud J. (2021). Effect of High-Intensity Interval Training on Quality of Life, Sleep Quality, Exercise Motivation and Enjoyment in Sedentary People with Type 1 Diabetes Mellitus. International Journal of Environmental Research and Public Health. Tips Tuesday and The Latest Physiopedia updates.
Publisher | Google Scholor