Case Report
Incidental Finding of Interrupted Inferior Venacava During Patent Ductus Arteriosus Device Closure Missed During Echocardiography
1Clinical Fellow in Pediatric Cardiology, Fortis Escorts Heart Institute, New Delhi, India.
2DNB Fellow in Pediatric Cardiology, Fortis Escorts Heart Institute, New Delhi, India.
3Director, Pediatric Cardiology, Fortis Escorts heart Institute, New Delhi, India.
*Corresponding Author: Touseef Ul Ayoub, DNB Fellow in Pediatric Cardiology, Fortis Escorts Heart Institute, New Delhi, India.
Citation: Satish K, Ul Ayoub T, Neeraj A. (2024). Incidental Finding of Interrupted Inferior Venacava During Patent Ductus Arteriosus Device Closure Missed During Echocardiography, Journal of Clinical Cardiology and Cardiology Research, BioRes Scientia Publishers. 3(3):1-3. DOI: 10.59657/2837-4673.brs.24.037
Copyright: © 2024 Touseef Ul Ayoub, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 16, 2024 | Accepted: September 05, 2024 | Published: September 11, 2024
Abstract
Background: An interrupted inferior vena cava (IVC) with azygos continuation represents a rare congenital anomaly. Despite its rarity, it can coexist with other congenital heart diseases. It is frequently overlooked during routine imaging studies. Failure to detect it during pre-procedural echocardiography can pose challenges in the catheterization lab, potentially leading to procedure cancellation. In our case, we successfully performed PDA device closure using an alternative approach.
Case Presentation: We present a case of a 6-year-old female with a history of prematurity and low birth weight, incidentally found to have a moderate-sized patent ductus arteriosus (PDA) during evaluation for a heart murmur. Pre-procedural echocardiography missed the presence of an interrupted IVC, complicating the planned transcatheter closure of the PDA. In the catheterization lab, the inability to advance the catheter into the IVC prompted further evaluation, revealing the anomaly. With Procedural modification utilizing only arterial access, successful PDA closure was performed. This case underscores the importance of comprehensive pre-procedural evaluation and intraoperative vigilance, particularly in patients with congenital anomalies.
Conclusion: Catheter-cardiac procedures are very commonly performed worldwide, and the inferior vena cava (IVC) serves as a primary channel for catheter insertion into the heart. Awareness of interrupted IVC is crucial for optimizing procedural success and patient safety during catheter-based interventions.
Keywords: interrupted inferior venacava (IVC); patent ductus arteriosus (PDA); transcatheter cardiac intervention; congenital heart disease (CHD); case report
Introduction
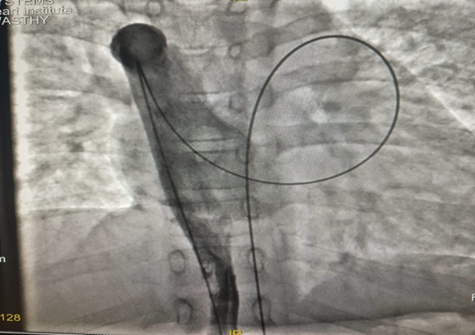
Interrupted inferior vena cava (IVC) with azygos continuation is a rare congenital anomaly. Here, the interruption occurs beneath the hepatic vein, with venous flow subsequently redirected through the dilated azygos and hemiazygos veins, ultimately draining to the superior vena cava (SVC). Reports of isolated congenital anomalies of the IVC are infrequent. The occurrence of this anomaly is estimated to be around 0.6% among individuals with congenital heart defects [1]. The interruption of the IVC accompanied by a well-developed azygos or hemiazygos continuation is frequently missed because of the absence of physiological abnormalities.
This condition becomes important during procedures like catheterization and transcatheter interventions. Additionally, accessing the heart via venous routes becomes challenging in cases of interrupted IVC, primarily due to the sharp angulation at the junction of the azygos vein and superior vena cava (SVC) [2]. Patent ductus arteriosus (PDA) is a common congenital heart defect characterized by the persistence of the fetal ductus arteriosus after birth. Transcatheter closure of PDA has become a widely accepted intervention due to its minimally invasive nature and effectiveness. However, pre-procedural evaluation for associated anomalies is crucial to ensure procedural success and patient safety [3].
Case Presentation
A 6-year-old female weighing 23 kg presented for evaluation due to an incidental finding of a heart murmur noted by her pediatrician. The child was born prematurely with a birth weight of 1.5 kg and had a history of prematurity and low birth weight, requiring a 2-week stay in the Neonatal Intensive Care Unit (NICU). Upon examination, the patient exhibited mild cardiomegaly with a left ventricular apex. The first heart sound (S1) and second heart sound (S2) were normal, and there was a continuous murmur heard in the left infraclavicular area. Chest X-ray revealed mild cardiomegaly. Echocardiography was performed, revealing a moderate-sized patent ductus arteriosus (PDA) measuring 3mm, with dilation of the left atrium and left ventricle. The patient was advised to undergo PDA device closure using an Amplatzer duct occlude sized 6/4.
Procedure and Findings
The child was taken to the cath lab with a plan to perform PDA device closure using the conventional approach (via arterial and venous access). Right femoral artery and right femoral venous access were obtained. However, when attempting to pass the catheter from the femoral vein to the inferior vena cava (IVC), the catheter was unable to reach the right atrium. Instead, it took an unusual path to the left innominate vein, and a hand injection of the IVC was performed, confirming the diagnosis of interrupted IVC. This anomaly, which had been missed in earlier imaging, was carefully evaluated during catheterization, prompting a change in the procedural approach.
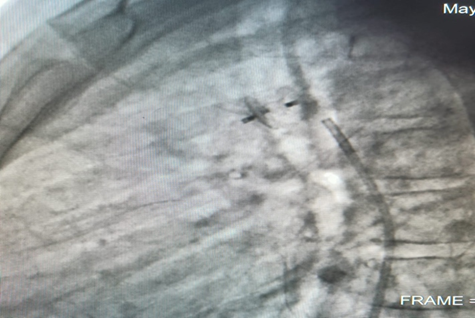
Given the presence of the interrupted IVC, it was decided to perform PDA closure only from the right femoral artery (only arterial approach) using Konnar MF VSD device closure (6mm X 4mm). The intervention was successful, with complete closure of the PDA achieved.
Figure 1: Fluroscopy Image showing Interrupted IVC With IVC continuing as Azygous vein and draining in SVC.
Figure 2: Fluoroscopy Image showing Konnar MF device post deployment.
Outcome and Follow-up
Post-procedural recovery was uneventful and the patient was discharged on the 2nd day post-procedure and remained asymptomatic during subsequent follow-up visits. Follow-up echocardiography confirmed successful closure of the PDA without residual shunt.
Discussion
The interruption of the IVC is a relatively uncommon anomaly, with an estimated incidence of 1 in 5,000 cases [4] During embryonic development, the IVC typically forms between the 6th and 8th weeks of gestation. If there is a failure in the fusion between the hepatic and prerenal segments during this process, it results in intrahepatic interruption of the IVC with azygos continuation. Consequently, blood diverts from the supra-sub cardinal anastomosis through the mildly dilated retrocrural azygos vein [5,6].
Children or adults with any congenital heart disease should undergo thorough echocardiography to rule out other associated anomalies. Those undergoing surgical or catheterization procedures should have systemic venous anomalies ruled out. The indirect evidence of increased flow through the superior vena cava (SVC) and findings of an azygous and hemiazygous channel on echocardiography provide valuable clues that hint towards the presence of an interrupted IVC.
Conclusion
This case highlights the importance of thorough pre-procedural evaluation and intraoperative vigilance in patients undergoing catheter-based interventions, particularly in the presence of congenital anomalies such as interrupted inferior vena cava. Despite being a rare finding, interrupted IVC should be carefully evaluated to avoid unnecessary chaos and unwanted complications in the catheterization lab. Awareness of such variations and their potential implications is crucial for optimizing patient outcomes and ensuring procedural success.
Declarations
Conflict of Interests
No financial or non-financial competing interests
Funding
No funding was secured for this case report
References
- Giang do TC, Rajeesh G, Vaidyanathan B. (2014). Prenatal Diagnosis of Isolated Interrupted Inferior Vena Cava with Azygos Continuation to Superior Vena Cava. Ann Pediatr Cardiol. 7:49-51.
Publisher | Google Scholor - Koh GT, Ai Mokthar S, Hamzah A, Kaur J. (2009). Transcatheter Closure of Patent Ductus Arteriosus and Interruption of Inferior Vena Cava with Azygous Continuation Using an Amplatzer Duct Occluder II. Ann Pediatr Cardiol. 2:159-161.
Publisher | Google Scholor - Backes CH, Hill KD, Shelton EL, Slaughter JL, Lewis TR, et al. (2022). Patent Ductus Arteriosus: A Contemporary Perspective for the Pediatric and Adult Cardiac Care Provider. J Am Heart Assoc. 11(17):e025784.
Publisher | Google Scholor - Akhtar S, Samad SM, Atiq M. (2010). Transcatheter Closure of a Patent Ductus Arteriosus in A Patient with An Anomalous Inferior Vena Cava. Pediatr Cardiol. 31:1093-1095.
Publisher | Google Scholor - Mandato Y, Pecoraro C, Gagliardi G, Tecame M. (2019). Azygos And Hemiazygos Continuation: An Occasional Finding in Emergency Department. Radiol Case Rep. 14:1063-1068.
Publisher | Google Scholor - Subramanian V, Mahadevan KK, Sivasubramonian S, Tharakan J. (2014). Pseudo Interruption of The Inferior Vena Cava Complicating the Device Closure of Patent Ductus Arteriosus: Case Report and Short Review of Venous System Embryology. Ann Pediatr Cardiol. 7(6):4-6.
Publisher | Google Scholor