Research Article
Identifying Intervention Levels in ICU Drug Therapy: Clinical Pharmacists' Impact on Patient and Prescriber Outcomes
- Okeroghene Aghogho Timipre 1
- Peter A. Owonaro 1*
- Joshua Funsho Eniojukan 1
- Sounyo Adekola Owonaro 1
- Awala E. Daughter 1
- Brisibe F. Seiyefa 2
- Dimie Ogoina 2
1Faculty of Pharmacy, Dept of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
2College of Health Sciences, Dept of Family Medicine, Niger Delta University, Amassoma, Nigeria.
*Corresponding Author: Peter A. Owonaro, Faculty of Pharmacy, Dept of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
Citation: Timipre O.A., Owonaro P.A., Eniojukan J.F., Owonaro S.A., Daughter A.E., et al. (2025). Identifying Intervention Levels in ICU Drug Therapy: Clinical Pharmacists' Impact on Patient and Prescriber Outcomes, Journal of Clinical Research and Clinical Trials, BioRes Scientia Publishers. 4(1):1-9. DOI: 10.59657/2837-7184.brs.25.040
Copyright: © 2025 Peter A. Owonaro, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 18, 2024 | Accepted: January 13, 2025 | Published: January 20, 2025
Abstract
Drug therapy problems (DTPs) are the major challenges in medication management, especially in intensive care units, as critically ill patients are more prone to these because of complicated and multiple medication regimens, as well as unstable conditions. The prospective observational study was conducted in a tertiary hospital in South-South Nigeria. It included 160 intensive care unit (ICU) patients admitted over one year, from July 2023 to July 2024. Data was collected by applying the Pharmaceutical Care Network Europe (PCNE) classification scheme to identify and classify DTPs. Most pharmacist interventions were made at the patient 53.1% and prescriber 40.0% levels, with only 4.4% being at the drug level. Demographic profile: The majority of subjects were in the age group of 65 and above, which comprised 34.4% and the majority were males, that is, 61.9%, and 71.9% were not insured. Interventions that involve patient-level counseling with written information and collaborative decision-making by prescribers involve the exchange of information. Our findings indicate that the clinical pharmacist makes a significant contribution at both the counseling of, and shared decision-making levels, to the pursuit of optimum therapeutic outcomes by the prescriber. Low levels of both drug-class and drug-level interventions indicate barriers that may need further study. It calls for increased multidisciplinary collaboration, insurance coverage for health services in a wider range, and even specialized critical care training by pharmacists.
Keywords: drug therapy problems; intensive care unit; clinical pharmacists; medication management; patient outcomes; pharmaceutical care; critical care; healthcare quality improvement
Introduction
Drug therapy problems (DTPs) are a major challenge in modern healthcare delivery, especially in critical care settings where the complexity of medication management is heightened by patient vulnerability and intricate treatment regimens (Shafiekhani et al., 2018; Tharanon et al., 2022). Defined as events or circumstances that impede optimal therapeutic outcomes, these problems have emerged as a crucial focus area in pharmaceutical care, especially within ICUs where the margin for error is small and the consequences of medication-related issues can be grave (Niriayo et al., 2018). The complexity of the medication management process is even more problematic in a critical care setting, where patients are usually exposed to many drugs at the same time and often need frequent therapeutic adjustments (Krähenbühl-Melcher et al., 2007). Studies have shown that multiple comorbidities, especially in older adults, enhance the risk of DTPs because of polypharmacy and altered drug responses (Adisa & Osoba, 2019; Šola et al., 2020; Hoel et al., 2021). This vulnerability increases in the ICU setting, where the physiological status of the patients is usually unstable and drug interactions may have a rapid and important impact on clinical outcomes.
Global healthcare data underlines this challenge: according to the estimates of the World Health Organization, more than 50% of all medicines are not taken as intended (Kim et al., 2018). The consequence of this is enormous healthcare expenses and many avoidable adverse events. These statistics are a more serious deal in critical care settings since critically ill patients have higher risks for drug-drug interactions, adverse drug events, and therapeutic failures. Some studies proved that unresolved DTP in ICU patients resulted in doubled risks for death and prolongations in days compared to their problem-free counterparts (Jimmy & Jose, 2011; Ofori-Asenso et al., 2016).
Clinical pharmacy has evolved as a specific discipline, in a very privileged position to address such challenges through expertise in the optimization of medication therapy and the enhancement of patient safety. In the context of the ICU, clinical pharmacists are valuable members of the healthcare team, offering unique knowledge on pharmacokinetics, drug interactions, and therapeutic monitoring (Gubbins et al., 2014; Carter, 2016; Urbańczyk et al., 2023). This role further extends beyond the traditional functions of medication dispensing into comprehensive management of medication therapies, optimization of doses, prevention of adverse events, and therapeutic drug monitoring (Lin et al., 2020).
This study explores a very important need indicated by current literature on understanding the impacts of clinical pharmacist interventions within the ICU and has thus been conducted in a tertiary hospital in South-South Nigeria. The study aims to ascertain the main levels of intervention at which clinical pharmacists are likely to have the greatest impact on patient outcomes and prescriber practices. The research study looks to avail the necessary insight for improved pharmaceutical care delivery and optimized therapeutic outcomes in critical care settings through an analysis of these intervention patterns. The importance of the study involves informing evidence-based practices in ICU pharmaceutical care, especially in resource-limited settings where optimization of healthcare delivery becomes important. The pattern and impact of pharmacist interventions should be known to guide and develop better protocols and training programs that will contribute to improved patient care and reduced medication-related complications in critical care. The objective of this study was to identify the level within the ICU treatment process where interventions are most commonly made by clinical pharmacists.
Methods
Setting and Design
This was a prospective observational study on drug therapy problems and their management carried out at the Intensive Care Unit in a tertiary health facility in South-South, Nigeria.
Study Population and Duration
The target population will consist of all patients who will be admitted to the ICU from July 1, 2023, to July 1, 2024. No sampling will be done since the population will consist of all the patients who will be admitted into the ICU within the period.
Data Collection Methodology
The major data collection tool utilized was the PCNE Classification Scheme, Version 9.1 (Foppe van Mil et al., 2020; Ahmed et al., 2021). It had five major sections with specific domains and subdomains which allowed the appropriate categorization of DTPs. The tool was indeed handy in capturing the complexities within DTPs in medication management for ICU patients with multi-comorbidities receiving complex therapeutic regimens. Demographic information was collected on a systematic basis for all participants.
Quality Assurance
The data collection instrument was evaluated for face validity by senior clinical pharmacists with academic and research experience. This will provide the appropriateness of the tool in measuring intended parameters.
Ethical Issue
The study was mounted following approval from the health research ethics committee of the tertiary hospital, hence assured of observing established protocols on research and protection of patients.
Results
Demographics of Sampled Patients
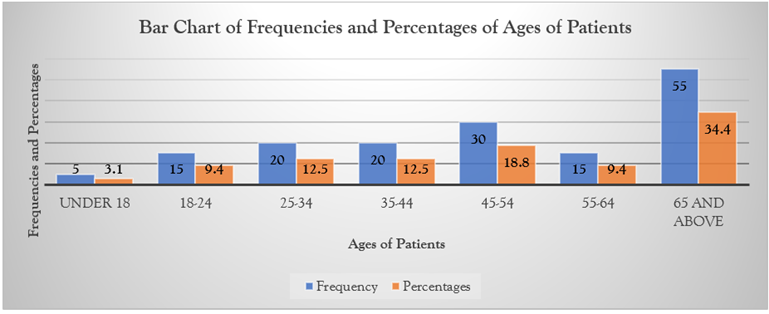
Figure 1: Bar Chart of Ages of Respondents.
The analysis of age distribution in 160 study participants showed that the study population was diversified across various age groups. Most of the patients were elderly, as evidenced by 55 (34.4%) aged 65 years and above; middle-aged patients were also well represented, with 30 patients (18.8%) between 45-54 years and 20 patients (12.5%) between 35-44 years. The age group comprising young adults from 18-24 years consisted of 15 patients, 9.4%, the same number as the 55-64 age bracket, 15 patients, and 9.4%. Pediatric patients below 18 years were the least represented, constituting a total of 5 individuals, 3.1% of the study population.
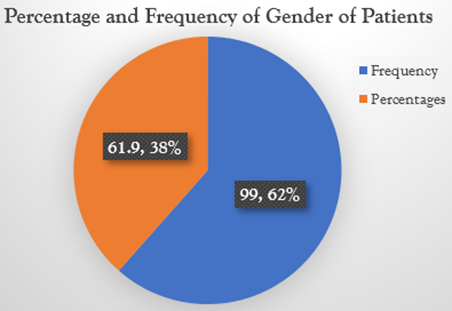
Figure 2: Gender of Patient.
In this, gender distribution analysis showed ICU admissions with the preponderance of males where 99 male patients account for 61.9% against 61 females, which amount to 38.1%. This almost constitutes a two-thirds majority in the study population.
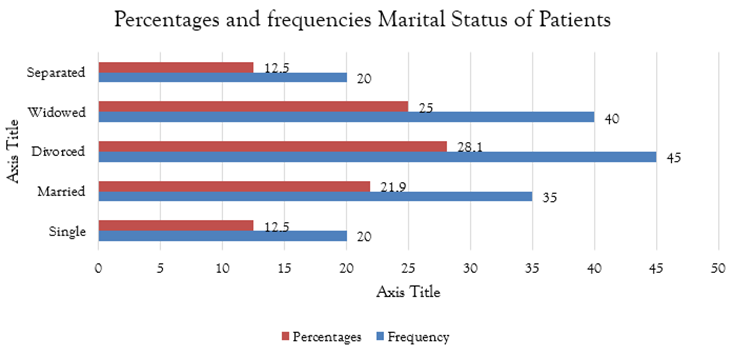
Figure 3: Marital Status.
In this study, 160 ICU patients were analyzed by marital status, showing that the most prevalent status was divorced, with 45 patients comprising 28.1%, closely followed by widowed status at 40 patients or 25.0%. Married patients were 35 cases or 21.9%, while single and separated patients were each 20 cases or 12.5%. Patients in a status of marital dissolution-which included divorced, widowed, and separated-comprised the majority of the subjects in this study.
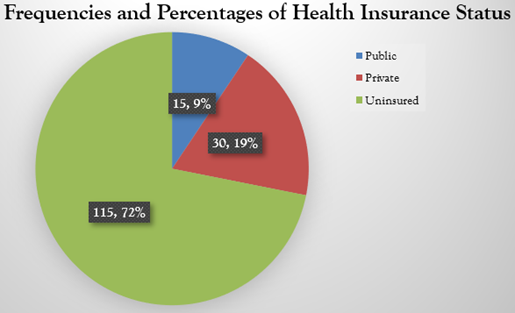
Figure 4: Health Insurance Status.
Health insurance status analyses showed that there was a steep variation in the insurance status of the selected 160 patients in ICUs. Most of them had no health insurance, 115 equated to 71.9%, followed by those with private insurance, where 30 stood at 18.8%, while those with public health insurance totaled 15 or 9.4%. From this, there is a visible significant lack of health insurance for patients, showing a greater level of vulnerability in the face of accessibility barriers and increased costs.
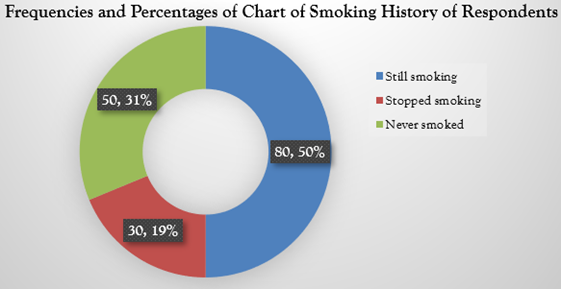
Figure 5: Smoking History.
This distribution of smoking status among the 160 ICU patients has presented alarming patterns: 80 currently smoking, which amounts to 50.0%, and 30 patients, 18.8%, were former smokers. A total of 50, or 31.3%, did not have any history of smoking. The high number of active smokers may indicate complications in the therapeutic management and increased risk for DTPs, considering the interference of smoking with the effectiveness of treatment and outcomes for the patients.
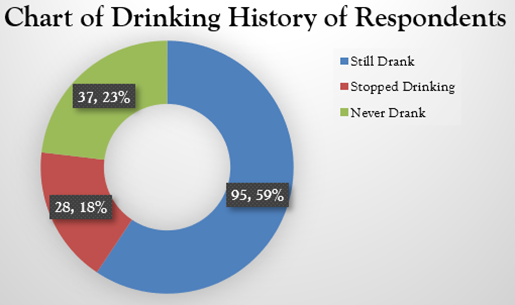
Alcohol consumption pattern analysis showed that out of the 160 ICU patients, 95 patients were current drinkers and accounted for 59.4%. The number of former drinkers was 28 (17.5%), and 37 patients reported lifetime abstinence, accounting for 23.1%. The preponderance of active alcohol users in the study population shows potential therapeutic complications and heightened susceptibility to DTPs, considering that alcohol may have a considerable influence on treatment effectiveness and patient outcome.
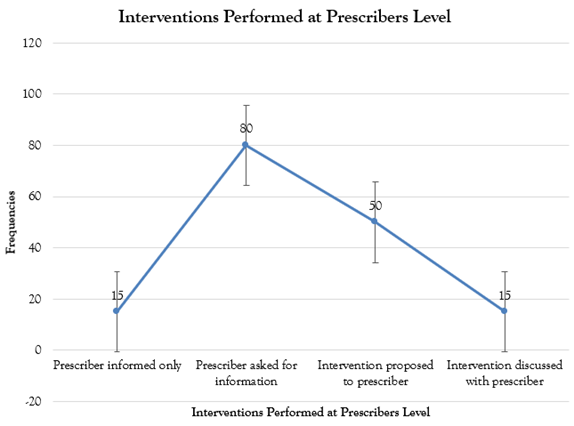
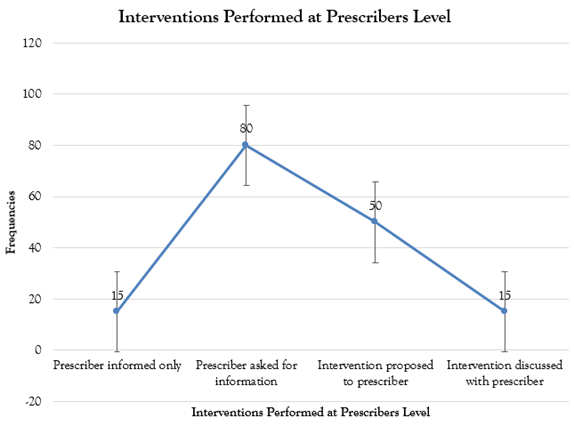
Figure 7: Interventions Performed at Prescriber's Level.
Analysis of the prescriber's level interventions done by clinical pharmacists, as depicted in Figure 7, showed that the interaction pattern varied. In 15 cases (9.4%), the information was provided solely to the prescribers. The majority of interactions involved active requests from prescribers to the pharmacists for information, which accounted for 80 cases (50.0%). Pharmacists also suggested interventions to prescribers in 50 cases (31.3%) and discussed collaboratively in 15 cases (9.4%).
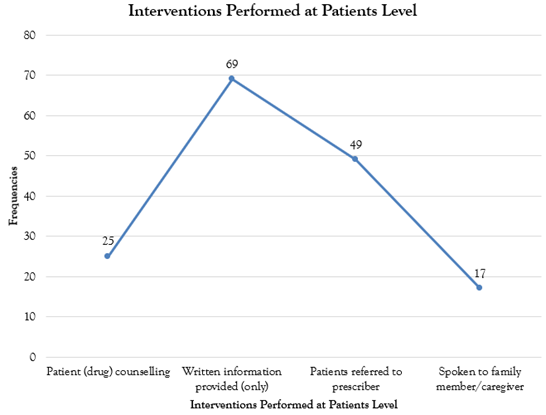
Patient-level interventions outlined in Figure 8 reveal the multilevel activity of clinical pharmacists in performing therapeutic management. The use of written documentation was thus the most frequent type, with 69 cases (43.1%). Prescriber referrals contributed to 49 cases (30.6%). Direct medication counseling services for patients were given in 25 instances (15.6%). Consultative interactions with family members and caregivers comprised 17 cases (10.6%), as shown in Figure 8 below, an indication of a holistic approach toward coordination of care for these patients.
Analysis of drug-level interventions as observed in Figure 9 reflects the various pharmaceutical adjustments provided by clinical pharmacists. The most frequent interventions concerned the withdrawal of drug administration, with 68 interventions, or 42.5%, followed by changes in medication instructions, with 42 interventions, or 26.3%. New initiations of drugs were carried out in 25 instances, or 15.6%, while dosage adjustments took place in 15, or 9.4%, cases. Other less common interventions were drug substitutions and formulation modifications, each contributing 5 cases (3.1%), further illustrating the diversity of therapeutic adjustments that are often required in clinical practice.
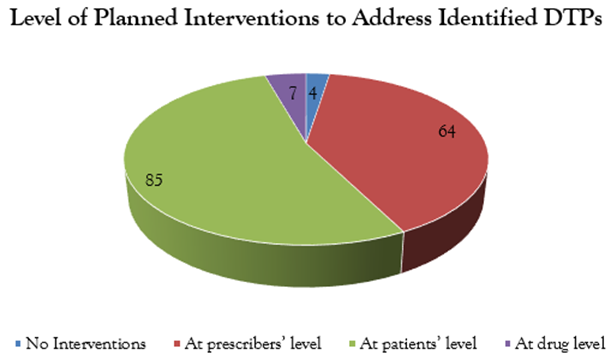
Figure 10: Level of Interventions Planned to address the Identified Drug Therapy Problems.
Figure 10 shows the intervention patterns analyzed, which indicates the hierarchical distribution of therapeutic interventions that were made to solve DTPs in the intensive care setting. The majority of interventions occurred at the patient level, with 85 cases constituting 53.1%, while prescriber-level interventions comprised 64 cases, or 40.0%. Modifications at the drug level comprised a much smaller percentage at 7 cases, or 4.4%, while a small subset of 4 cases, or 2.5%, required no intervention. These findings stressed the strategic focus on both patient-centered and prescriber-collaborative approaches; collectively, these represented 93.1% of all therapeutic interventions, thus setting these as the main channels for DTP management in the critical care environment.
Discussion
Overview of Main Findings
This is representative of the important role clinical pharmacists play in intensive care units as it relates to medication-related problems. Most interventions, 53.1%, were by direct patient contact and by prescriber contact, amounting to 40.0%. It has been suggested that pharmacists are involved with direct patient care and health provider consultation to ensure effective treatment, demonstrating an approach to patient-oriented pharmaceutical service (Alvarez et al., 2017).
Patient-Level Interventions
The predominance of patient-level interventions represents 53.1% and shows the great emphasis laid on direct patient engagement and education. These include written information, accounting for 43.1% of the patient-level interventions, and patient drug counseling, accounting for 15.6%, thus putting clear communication in the limelight as regards the mitigation of DTPs. This calls, therefore, for a high proportion of information in writing, since this strategy assures retention and adherence to information, which may be crucially important in the ICU setting, where the state of the patient's consciousness and/or cognition is variable (Bronkhorst et al., 2014; Hilgarth et al., 2023). In pharmaceutical care, this is one of those practices widely espoused since the written materials can act as a useful reference to patients and their caregivers in or outside the environment (Ho et al., 2013; Chiang et al., 2020).
Prescriber-Level Collaboration
The high proportion of prescriber-level interventions at 40.0% shows the collaborative nature of pharmaceutical care in an ICU setup. Our data indicate that 50.0% of prescribers themselves sought information from clinical pharmacists and, thus, strongly recognized the place of a pharmacist for his expertise as an integral member of the healthcare team (Alsayed et al., 2024; Wei et al., 2024). Of these, 31.3% of the interventions were proposed to prescribers, and 9.4% involved discussions in depth, showing the dynamic and consultative relationship between the pharmacist and the prescribers (Cvikl & Sinkovič, 2020; Hilgarth et al., 2023). This collaboration is highly essential in the ICU environment when complicated medication regimens, together with the critical states of the patients, require close coordination among caregivers (Gomes & Guidoni, 2023).
Challenges in Drug-Level Interventions
The percentage of intervention at the drug level is very low, at 4.4%. This result is interesting for further discussion. The low engagement at the drug level can be justified based on many reasons like complicated patient conditions, time constraints, institutional protocols, and resource limitations (MacTavish et al., 2023; Ahmed et al., 2024). Most of the patients in the ICU have multiple comorbidities in unstable conditions; hence, major modifications of drugs could be risky. The results indicated that 34.4% of the patients were 65 years and above; this age group requires conservative approaches to medication management.
Demographic and Socioeconomic Considerations
Demographic analysis brings forth several factors that will possibly influence the approach toward the DTPs. A predominance of males, 61.9%, would suggest a host of potential gender-specific medication management considerations. The very high percentage of patients, 71.9%, not having insurance raises several potential concerns about medication accessibility and adherence, and thus the kinds of interventions that can realistically be instituted.
Lifestyle and Social Support Factors
Lifestyle factors were identified as one of the important concerns in DTP management. In this case, 50.0% currently smoking and 59.4% presently drinking added more to the challenge in managing the drug therapy. These habits will ultimately have their impacts on the pharmacokinetic drug profile: metabolism, efficacy, and interaction need cautious attention while planning pharmaceutical care (Fraser, 1997; Koppisetti & Chandra, 2011; Masoomzadeh & Javadzadeh, 2021). A distribution indicating that 28.1% of the patients are divorced and 25.0% widowed shows that medication management needs to address social support systems.
Resource Limitations and Care Delivery
These findings of the results of interventions confirm the literature findings but provide new insights into specific challenges found within developing country contexts. The emphasis on patient and prescriber-level interventions reflects a pragmatic approach toward pharmaceutical care. Direct communication and education will more often be immediate tools in medication outcome improvement. It has much to do with resource-limited settings where advanced drug monitoring systems may not be available.
These findings add to the ever-increasing evidence regarding the critical role of the clinical pharmacist within the ICU, pointing at the same time to areas where more effort and investment will be needed. Specifically, the results emphasize the need for balanced intervention strategies that pay attention to immediate patient care needs and systemic challenges in healthcare delivery.
Conclusion
This study provides an overview of the intervention patterns of clinical pharmacists addressing DTPs in the ICU and underlines their predominant focus on patient level, with 53.1% and prescriber level with 40.0% interventions. The findings illustrate both the extended role of pharmacists in critical care but also point to areas of potential improvement, particularly regarding drug-level interventions at 4.4%. This very high proportion of uninsured patients-71.9% combined with high, lifestyle-related risk factors-apparently indicates that comprehensive health-care strategies should go far beyond medication management. Efforts in the future will have to be directed toward enhanced interdisciplinarity, a stronger take-up of health insurance coverage, and special training for critical care pharmacists. In this way, this setting is going to be extremely vital to optimizing pharmaceutical care and better outcomes for patients in the ICU.
Recommendations
To improve the management of DTPs in the ICU, there should be interprofessional collaboration through effective communication of the pharmacist with other health team professionals. Further, expansion in health insurance coverage and special critical care training for pharmacists is greatly beneficial for achieving optimal patient outcomes with lesser chances of DTP occurrence.
Public Health Implications
It has been shown that this will be useful in improving patient safety by reducing healthcare costs and likely decreasing adverse drug events through proactive pharmacist interventions and fewer days of hospitalization. Narrowing health insurance is vital to advance the interests in health equity, and make it necessary for all patients to gain access to essential drugs. In addition, targeted public health efforts aimed at reducing smoking and alcohol consumption can help reduce susceptibility to DTPs and improve overall community health.
Authors' Conflict of Interest
The authors declare no conflict of interest.
References
- Alsayed, H. A. H., Sharif-Askari, F. S., Sharif-Askari, N. S., Halwani, R. (2024). Clinical Pharmacist Interventions in An Intensive Care Unit Reduces ICU Mortality at A Tertiary Hospital in Dubai, United Arab Emirates. Exploratory Research in Clinical and Social Pharmacy, 14:100431.
Publisher | Google Scholor - Adisa, R., Osoba, D. O. (2019). Evaluation of Drug Therapy Problems Among Outpatient Hypertensive and Type-2-Diabetic Patients at A Tertiary Hospital, South-West Nigeria. Nigerian Journal of Pharmaceutical Research, 15(2):127-141.
Publisher | Google Scholor - Alfayez, O. M., Al Yami, M. S., Fazel, M. T. (2017). The Impact of Pharmacists Providing Direct Patient Care as Members of Interprofessional Teams on Diabetes Management. Saudi Pharmaceutical Journal, 25(7):1019-1021.
Publisher | Google Scholor - Ahmed, K. O., Muddather, H. F., Yousef, B. A. (2021). Pharmaceutical Care Network Europe (PCNE) Drug-Related Problems Classification Version 9.1: First Implementation in Sudan. Journal of Pharmaceutical Research International, 33(59A):699-706.
Publisher | Google Scholor - Ahmed, N. A., Fouad, E. A., El-Asheer, O. M., Ghanem, A. S. M. (2024). Pharmaceutical Interventions for Drug-Related Problems in The Neonatal Intensive Care Unit: Incidence, Types, And Acceptability. Frontiers in Pharmacology, 15:1391657.
Publisher | Google Scholor - Bronkhorst, E., Schellack, N., Gous, A. G. S., Pretorius, J. P. (2014). The Need for Pharmaceutical Care in An Intensive Care Unit at A Teaching Hospital in South Africa. Southern African Journal of Critical Care, 30(2):41-44.
Publisher | Google Scholor - Carter, B. L. (2016). Evolution of Clinical Pharmacy in The USA and Future Directions for Patient Care. Drugs & Aging, 33(3):169-177.
Publisher | Google Scholor - Chiang, L. H., Huang, Y. L., Tsai, T. C. (2021). Clinical Pharmacy Interventions in Intensive Care Unit Patients. Journal of Clinical Pharmacy and Therapeutics, 46(1):128-133.
Publisher | Google Scholor - Cvikl, M., Sinkovic, A. (2020). Interventions of a Clinical Pharmacist in A Medical Intensive Care Unit–A Retrospective Analysis. Bosnian Journal of Basic Medical Sciences, 20(4):495.
Publisher | Google Scholor - Fraser, A. G. (1997). Pharmacokinetic Interactions Between Alcohol and Other Drugs. Clinical Pharmacokinetics, 33:79-90.
Publisher | Google Scholor - Foppe Van Mil, J. W., Horvat, N., Westerlund, T., Richling, I. (2020). Classification For Drug-Related Problems (V9.1). Pharmaceutical Care Network Europe Association. 1-3.
Publisher | Google Scholor - Gomes, M. F., Guidoni, C. M. (2023). An Analysis of Pharmaceutical Care for Critical Patients of An Adult Intensive Care Unit. Brazilian Journal of Pharmaceutical Sciences, 59:e21345.
Publisher | Google Scholor - ACCP, Gubbins, P. O., Micek, S. T., Badowski, M., Cheng, J., et al. (2014). Innovation in Clinical Pharmacy Practice and Opportunities for Academic-Practice Partnership. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 34(5):e45-e54.
Publisher | Google Scholor - Hilgarth, H., Wichmann, D., Baehr, M., Kluge, S., Langebrake, C. (2023). Clinical Pharmacy Services in Critical Care: Results of An Observational Study Comparing Ward-Based with Remote Pharmacy Services. International Journal of Clinical Pharmacy, 45(4):847-856.
Publisher | Google Scholor - Ho, C. K., Mabasa, V. H., Leung, V. W., Malyuk, D. L., Perrott, J. L. (2013). Assessment of Clinical Pharmacy Interventions in The Intensive Care Unit. The Canadian Journal of Hospital Pharmacy, 66(4):212.
Publisher | Google Scholor - Hoel, R. W., Connolly, R. M. G., Takahashi, P. Y. (2021, January). Polypharmacy management in older patients. In Mayo Clinic Proceedings. 96(1):242-256.
Publisher | Google Scholor - Jimmy, B., Jose, J. (2011). Patient Medication Adherence: Measures in Daily Practice. Oman Medical Journal, 26(3):155-159.
Publisher | Google Scholor - Kim, J., Combs, K., Downs, J., Tillman, F. (2018). Medication Adherence: The Elephant in the Room. Us Pharm, 43(1):30-34.
Publisher | Google Scholor - Koppisetti, V. S., Chandra, N. (2011). Influence of Alcohol and Smoking on Drug Action: A Step for Better Utilization of Drugs. J. Chem, 3(1):242-248.
Publisher | Google Scholor - Krähenbühl-Melcher, A., Schlienger, R., Lampert, M., Haschke, M., Drewe, J., et al. (2007). Drug-Related Problems in Hospitals: A Review of the Recent Literature. Drug Safety, 30:379-407.
Publisher | Google Scholor - Lin, H. W., Yang, L. C., Mafruhah, O. R., Nguyen, H. T., Cao, T. T., et al. (2020). Evolution of Clinical Pharmacy Practice and Pharmacy Education in Taiwan, Vietnam, and Indonesia: A Narrative Review. Journal of the American College of Clinical Pharmacy, 3(5):947-958.
Publisher | Google Scholor - MacTavish, P., Quasim, T., Purdie, C., Ball, M., Barker, L., et al. (2020). Medication-Related Problems in Intensive Care Unit Survivors: Learning from A Multicenter Program. Annals of the American Thoracic Society, 17(10):1326-1329.
Publisher | Google Scholor - Salar Masoomzadeh, Yousef Javadzadeh. (2021). Does Alcohol Able to Change Pharmacokinetics of Drugs in Alcoholic People? Journal of Drug and Alcohol Research. 10(12).
Publisher | Google Scholor - Niriayo, Y. L., Kumela, K., Kassa, T. D., Angamo, M. T. (2018). Drug Therapy Problems and Contributing Factors in The Management of Heart Failure Patients in Jimma University Specialized Hospital, Southwest Ethiopia. PloS One, 13(10):e0206120.
Publisher | Google Scholor - Ofori-Asenso, R., Agyeman, A. A. (2016). Irrational Use of Medicines-A Summary of Key Concepts. Pharmacy, 4(4):35.
Publisher | Google Scholor - Shafiekhani, M., Mirjalili, M., Vazin, A. (2018). Psychotropic Drug Therapy in Patients in The Intensive Care Unit-Usage, Adverse Effects, and Drug Interactions: A Review. Therapeutics and Clinical Risk Management, 14:1799-1812.
Publisher | Google Scholor - Sola, K. F., Mucalo, I., Brajkovic, A., Jukic, I., Verbanac, D., et al. (2020). Drug Therapy Problems Identified Among Older Adults Placed in A Nursing Home: The Croatian Experience. Journal of International Medical Research, 48(6):0300060520928791.
Publisher | Google Scholor - Tharanon, V., Putthipokin, K., Sakthong, P. (2022). Drug-Related Problems Identified During Pharmaceutical Care Interventions in An Intensive Care Unit at A Tertiary University Hospital. Sage Open Medicine, 10:20503121221090881.
Publisher | Google Scholor - Urbanczyk, K., Guntschnig, S., Antoniadis, V., Falamic, S., Kovacevic, T., et al. (2023). Recommendations For Wider Adoption of Clinical Pharmacy in Central and Eastern Europe in Order to Optimise Pharmacotherapy and Improve Patient Outcomes. Frontiers in Pharmacology, 14:1244151.
Publisher | Google Scholor - Wei, C., Hu, M., Chen, G., Yan, Z., Yin, W., et al. (2024). Cost-Effectiveness Analysis of Pharmaceutical Care in Adult Critically Ill Patients: Based on A Prospective Cohort Study. Frontiers in Pharmacology, 15:1446834.
Publisher | Google Scholor