Research Article
Factors Affecting the Psychological Well-being of Caregivers of Dementia Patients: A Thematic Review
- Jeevitha Gowda R *
- Parimala Guruprasad
M.Sc., MS Ramaiah University of Applied Sciences, New BEL Road, MSR Nagar, Bangalore, Karnataka, India.
*Corresponding Author: Jeevitha Gowda R, M.Sc., MS Ramaiah University of Applied Sciences, New BEL Road, MSR Nagar, Bangalore, Karnataka, India.
Citation: Jeevitha Gowda R., Guruprasad P. (2025). Factors Affecting the Psychological Well-being of Caregivers of Dementia Patients: A Thematic Review, Clinical Case Reports and Studies, BioRes Scientia Publishers. 9(3):1-9. DOI: 10.59657/2837-2565.brs.25.225
Copyright: © 2025 Jeevitha Gowda R., this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 15, 2025 | Accepted: January 29, 2025 | Published: February 05, 2025
Abstract
Background: Dementia is a progressive neurodegenerative condition that requires extensive caregiving, often leading to significant psychological distress among caregivers. Understanding the factors affecting the well-being of caregivers is essential for developing effective support strategies.
Aim: This thematic review explores the key factors that influence the psychological well-being of caregivers of dementia patients.
Methods: A systematic review was conducted using 45 peer-reviewed studies published between 2015 and 2024. The studies were sourced from PubMed, PsycINFO, and Scopus, using keywords such as dementia caregivers, psychological well-being, and caregiver burden. Data were analyzed and grouped into four thematic domains: psychosocial, emotional, physical, and environmental factors.
Results: This thematic review explores factors affecting the psychological well-being of dementia caregivers. Key influences include age, gender, marital status, educational level, and social support. The review highlights the importance of tailored interventions, such as respite care and caregiver education, to alleviate caregiver stress and improve mental health outcomes.
Conclusion: The review emphasizes the multifaceted nature of caregiver distress. Targeted interventions, including caregiver education, support networks, and respite care, are critical to alleviating caregiver burden and improving well-being. Future research should focus on longitudinal studies and culturally tailored interventions to better address the unique challenges faced by dementia caregivers.
Key Message
Caregiving for dementia patients significantly impacts caregivers’ psychological well-being across psychosocial, emotional, physical, and environmental domains. Key factors contributing to caregiver distress include role strain, social isolation, emotional distress, physical health decline, and environmental stressors such as financial strain and inadequate healthcare access. Interventions aimed at providing emotional support, enhancing social networks, offering caregiver education, and ensuring respite care are essential in alleviating caregiver burden. The review underscores the need for targeted, culturally sensitive support systems and further research to understand and address the evolving challenges faced by dementia caregivers.
Keywords: dementia; caregivers; psychological well-being; caregiver burden; thematic review
Introduction
Dementia is a progressive neurodegenerative condition characterized by the decline of cognitive abilities, including memory, reasoning, and behavior, significantly impairing daily functioning. Globally, an estimated 55 million people live with dementia, and this number is projected to rise to 78 million by 2030 due to aging populations (Dementia, n.d.). This growing prevalence places a considerable burden not only on healthcare systems but also on family caregivers, who provide the majority of care for individuals with dementia in many countries. Caregivers, often untrained and unpaid family members, take on the dual roles of emotional support and physical care, often to the detriment of their well-being (Brodaty & Donkin, 2009). The psychological well-being of caregivers is an essential yet often overlooked aspect of dementia care. Studies show that caregivers frequently experience high levels of stress, depression, and anxiety, with some reporting symptoms akin to post-traumatic stress disorder (Sörensen & Conwell, 2011). These mental health challenges are compounded by the progressive nature of dementia, which demands increased caregiving effort over time. Caregivers may also face anticipatory grief as they witness the decline of their loved ones, leading to emotional exhaustion (Garand et al., 2012).
In low- and middle-income countries (LMICs) like India, the caregiving burden is exacerbated by cultural expectations and limited access to professional healthcare resources (Sharma & Popli, 2023). Family caregivers are often expected to shoulder the responsibility of care due to strong familial norms, which may leave them isolated and unsupported (Shaji et al., 1996). Additionally, financial constraints and the lack of specialized dementia care services create a compounded stress burden, making it difficult for caregivers to prioritize their mental health. The caregiving experience is multifaceted and influenced by a variety of psychosocial, emotional, physical, and environmental factors. Psychosocial stressors, such as role strain and social isolation, are among the most significant challenges reported by caregivers (Becerra Carrillo et al., 2024). Emotional factors, including feelings of guilt, sadness, and even resentment, further compromise psychological well-being. Physical health is also adversely affected due to chronic stress, sleep disturbances, and the physical demands of caregiving (Wesson et al., 2017). Environmental factors, such as financial strain and inadequate living conditions, create additional barriers to maintaining mental health. This thematic review aims to explore the complex interplay of these factors, synthesizing evidence to identify key determinants of psychological well-being in caregivers of dementia patients. By understanding these determinants, healthcare practitioners, policymakers, and researchers can develop targeted interventions to alleviate caregiver burden and improve their quality of life. Furthermore, this review emphasizes the need for culturally sensitive solutions, particularly in resource-limited settings, to address the unique challenges faced by caregivers globally.
Methodology
Literature Search
A literature search was conducted using MEDLINE, Scopus, and Google Scholar to identify articles meeting the following inclusion criteria:
- Published in English-language journals.
- Appeared in peer-reviewed publications.
- Focused on factors affecting the psychological well-being of caregivers of dementia patients.
Searching and Screening
The search was conducted in three stages to refine results and retrieve the most relevant articles at the first level, search terms related to psychological outcomes were used, including “anxiety,” “depression,” “stress,” and “psychological well-being.” In the second level terms associated with dementia caregiving were applied, such as “dementia caregivers,” “caregiver burden,” “emotional distress,” and “family caregiving.” Finally in the third level search terms specific to caregiving contexts were utilized, such as “long-term care,” “informal caregiving,” and “caregiver challenges.”
The search was independently carried out by two authors, and results were combined. Identified citations were compiled into a master list, and duplicate articles were excluded. Articles selected for detailed review included various study designs, such as original research articles, systematic reviews, narrative reviews, qualitative studies, and commentaries.
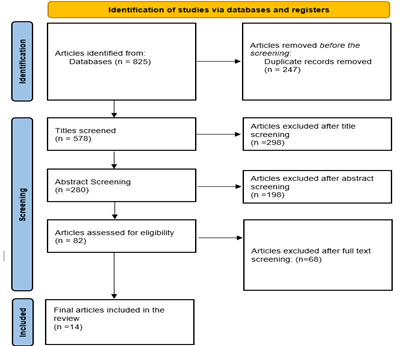
Titles of the articles were screened to exclude irrelevant studies. Abstracts of the remaining articles were then reviewed to further refine the selection. Full-text screening was conducted to ensure adherence to inclusion criteria. The methodological process of article selection is illustrated in Figure 1.
Figure 1: Flowchart of Screening and Inclusion/Exclusion of Articles
Data Extraction
Data from selected articles were systematically organized in a spreadsheet. Extracted information included:
- Year and country of publication.
- Type and design of the study.
- Nature of the caregiver sample and sample size.
- Psychological factors studied (e.g., stress, depression).
- Study findings and conclusions.
- Limitations of each study.
This process enabled a comprehensive overview of existing literature on the topic.
Data Synthesis
A thematic analysis approach was employed to group identified factors into categories based on common themes:
- Psychosocial Factors: Including role strain, social isolation, and caregiver identity.
- Emotional Factors: Guilt, grief, and emotional distress.
- Physical Factors: Chronic fatigue, sleep disturbances, and health deterioration.
- Environmental Factors: Financial stress, access to healthcare, and living conditions.
Factors with statistically significant associations reported in multiple studies were highlighted. Discrepancies in findings were analyzed, and reasons for varying effects were discussed. Additionally, recommendations suggested by authors for mitigating caregiver distress were noted.
Results
The initial search conducted using the methodology outlined in the review produced over 825 results. These were filtered to exclude studies that did not focus on the factors responsible for mental health challenges among dementia caregivers. After applying inclusion and exclusion criteria, the most relevant studies were selected. The results selected from the selected articles are given in table 1.
| Author | Study Type and Design | Caregiver Sample and Size | Psychological Factors Studied | Findings and Conclusions | Limitations |
| (Pinyopornpanish et al., 2021) | Cross-sectional | 102 caregivers (average age 55, Female 77.5%) | Perceived stress, depressive symptoms | Caregiver burden linked to neuropsychiatric symptoms of patients via stress and depression (r = 0.21, p = 0.001) | No longitudinal follow-up, self-report bias |
| (Park et al., 2021) | Cross-sectional | 371,287 caregivers (Female 50%, Male 50%) | Depressive symptoms | Family caregivers’ depressive symptoms linked to living with dementia patients (OR 1.47, CI 1.32–1.62) | Lack of specific data on caregiving experience |
| (Liu et al., 2020) | Cross-sectional | 279 caregivers (Female 62.7%) | Stress load, behavioral symptoms | Behavioral symptoms of patients and disease progression impacted caregiver well-being and finances (r = 0.319, p < 0> | Limited to a specialist outpatient setting |
| (Su & Chang, 2020) | Cross-sectional | 270 caregivers (Female 50%, Male 50%) | Affiliate stigma, anxiety | Caregiver stigma linked to higher anxiety and caregiver burden (p < 0> | No long-term follow-up |
| (Baharudin et al., 2019) | Cross-sectional | 202 caregivers (Female 71.3%) | Coping strategies, BPSD | Caregiver burden linked to BPSD and moderated by coping strategies and personality (r = 0.199, p < 0> | Cross-sectional design limits causality conclusions |
| (Shikimoto et al., 2018) | Cross-sectional | 1,437 caregivers (Not specified) | Psychological distress | 14.9% of caregivers showed signs of depression/anxiety due to care duties and dementia-related symptoms (p < 0> | Self-reporting of mental health conditions |
| (Park et al., 2018) | Cross-sectional | 320 caregivers (Female 63.8%, Male 36.3%) | Unmet needs, caregiving satisfaction | Formal support mediated caregiver burden and satisfaction (χ2 (p) = 256.60, p < 0> | No intervention testing |
| (Shim et al., 2015) | Longitudinal | 110 caregivers (Female 75.5%) | Neuropsychiatric symptoms, memory impairment | Memory impairment and neuropsychiatric symptoms predicted caregiver burden (r = 0.37, p < 0> | Short follow-up period (1 year) |
| (Kim et al., 2016) | Descriptive-phenomenological | 12 caregivers (Female 100%) | Anxiety, financial impact | Caregivers showed anxiety about the course of dementia and its financial impact | Small sample size, subjective reporting |
| (Yu et al., 2016) | Cross-sectional | 401 caregivers (Female 62.6%) | Filial piety, caregiving burden | Filial piety partially mediated the caregiving burden, related to BPSD (r = −0.28, p < 0> | Cultural specificity of the sample |
| (Goren et al., 2016) | Cross-sectional | 1,302 caregivers (Female 53%, Male 47%) | Health-related quality of life | Caregivers showed poorer health-related quality of life and greater comorbid risks (p < 0> | No focus on dementia severity or subtype |
| (Yu et al., 2015) | Cross-sectional | 168 caregivers (Female 68.5%) | Cognitive function, caregiving hours | Higher patient cognitive decline and caregiving hours correlated with increased caregiver burden (r = −0.28, p < 0> | Lack of exploration into caregiving satisfaction |
| (Zhang et al., 2013) | Case-control | 58 caregivers (Female 72%) | Psychological distress, family functioning | Caregivers experienced impaired family functioning and low social support (p < 0> | Small sample size, limited to urban settings |
| (Etters et al., 2008) | Comprehensive literature review | Not applicable (review of studies) | Caregiver burden (CB), dementia, caregiver health, early nursing home placement | Factors like gender, relationship to patient, culture, and personal characteristics influence caregiver burden. | Focus on articles from 1996-2006; limitations not explicitly stated. |
Detailed Thematic Breakdown
The results of the studies examined reveal several key themes related to the mental health of dementia caregivers. These include the impact of age, gender, marital status, educational level, and the availability of support networks, among others. Each of these factors plays a significant role in determining caregiver distress and mental health outcomes.
Age of Caregivers
Age significantly influences the mental health of dementia caregivers, with studies suggesting that older caregivers tend to report more resilience compared to their younger counterparts. Older caregivers often have greater life experience, which may enhance their ability to cope with stressors. However, younger caregivers, especially those balancing caregiving with family and career responsibilities, often experience higher levels of stress. The study by, for instance, found that younger caregivers were more prone to psychological distress due to the additional burdens of work and family life (Pinyopornpanish et al., 2021). Younger caregivers also tend to have fewer coping mechanisms and may struggle more with the emotional and physical demands of caregiving.
Gender Differences in Caregiver Mental Health
Gender plays a critical role in determining the mental health of dementia caregivers. In many studies, women caregivers report higher levels of distress, including anxiety and depression, compared to men. This can be attributed to the dual responsibilities that women often carry, both as caregivers and as individuals expected to manage household duties. For instance, (Kim et al., 2016) observed that middle-aged female caregivers experienced anxiety related to the uncertainty of their loved one's condition and the overwhelming responsibilities they faced. While men also experience stress, their emotional responses may be different, often characterized by feelings of helplessness or isolation. The impact of caregiving on men's mental health is often less recognized, but some studies suggest that men are not immune to significant distress, especially when they feel isolated or unsupported in their caregiving role.
Marital Status and Caregiver Mental Health
Marital status is another critical factor affecting caregiver distress. Married caregivers, for example, often experience increased anxiety and stress due to the dual responsibility of managing caregiving alongside family and household duties. This was highlighted in the study by (Park et al., 2018), which found that married caregivers experienced higher levels of depressive symptoms, likely due to the added stress of managing multiple roles (Park et al., 2021). Conversely, unmarried caregivers may experience different stressors, such as a lack of emotional support or social isolation. Studies suggest that unmarried caregivers are more likely to report depressive symptoms, as they lack the social support that a partner could provide. Both marital status and the availability of a supportive partner appear to influence mental health outcomes significantly.
Educational Level and Caregiver Mental Health
The educational level of caregivers is closely tied to their mental health. Caregivers with higher education levels tend to report better mental health outcomes, likely due to their greater understanding of dementia and caregiving techniques. As noted by (Liu et al., 2020), caregivers with higher levels of education tend to have better access to healthcare resources and are more adept at managing stress through education and self-care practices. Higher education may also correlate with better problem-solving skills, which could help caregivers manage the emotional and physical challenges of caregiving. Conversely, caregivers with lower levels of education may struggle more with navigating the healthcare system and understanding dementia, leading to higher levels of stress and anxiety. Education may also play a role in fostering social support networks, which are essential for reducing caregiver burden.
Social Isolation and Support Networks
The presence or absence of social support is one of the most significant factors affecting caregiver mental health. Caregivers who lack a strong social support network often experience higher levels of depression, anxiety, and stress. Studies such as (Shikimoto et al., 2018)highlight the importance of formal and informal support systems for caregivers. Those with strong support systems—whether family, friends, or community resources—tend to report lower levels of caregiving burden and better mental health outcomes. Caregivers who are socially isolated, on the other hand, often feel overwhelmed by their responsibilities and are at a greater risk for burnout and mental health deterioration. The study by (Park et al., 2018) emphasized that formal support services, such as respite care and professional counselling, can play a key role in reducing caregiver stress. Overall, the mental health of dementia caregivers is influenced by multiple interconnected factors, including age, gender, marital status, educational level, and social support. Caregivers' ability to manage their mental health is affected by their coping skills, the availability of resources, and their social and family dynamics. The studies reviewed indicate that interventions aimed at supporting caregivers should consider these factors to be most effective. Tailored support, such as respite care, educational programs, and the fostering of strong social networks, can help alleviate caregiver burden and improve mental health outcomes for those caring for individuals with dementia.
Discussion
The findings of this review underscore the multifaceted nature of caregiver mental health, particularly within the context of dementia caregiving. The mental and emotional well-being of caregivers is influenced by various factors, including age, gender, marital status, educational level, social support, and physical health. These variables interact in complex ways, shaping caregivers’ stress levels, coping mechanisms, and overall mental health outcomes.
Age and Caregiver Mental Health
One of the most significant factors influencing caregiver mental health is age. As highlighted by (Pinyopornpanish et al., 2021), older caregivers often show more resilience due to their accumulated life experience, while younger caregivers tend to experience higher levels of distress. Younger caregivers often struggle with caregiving responsibilities while simultaneously balancing other roles, such as employment and raising children. These additional burdens may amplify their emotional distress, as they lack both the coping skills developed over time and the resources to manage the complex caregiving demands (Etters et al., 2008). This suggests that interventions should be tailored to age-specific needs, addressing the distinct challenges faced by younger and older caregivers.
Gender Differences in Caregiving Stress
Gender is another critical factor in caregiver mental health. Several studies, including (Kim et al., 2016) demonstrate that women caregivers report higher levels of distress, including depression and anxiety, likely due to the dual expectations placed on them in both the caregiving and domestic spheres. This pattern is compounded by societal norms that often place the caregiving burden primarily on women. However, men also experience stress, though often in different forms, such as feelings of isolation or helplessness. (Park et al., 2021) observed that male caregivers, while less likely to express their distress openly, often experience significant mental health challenges, including depression and anxiety, though they may not seek support due to cultural expectations around masculinity. The gendered nature of caregiving stress suggests that interventions need to be sensitive to both the overt and covert ways in which caregiving impacts mental health for men and women.
Marital Status and Social Support
Marital status plays a significant role in caregiver mental health outcomes. Married caregivers, as noted by (Park et al., 2021), often report higher levels of anxiety, likely due to the combined pressures of caregiving and other family responsibilities, including financial concerns and maintaining the household. These caregivers face the dual challenge of managing caregiving duties alongside their marital and parental roles. On the other hand, unmarried caregivers tend to experience social isolation, which can further exacerbate feelings of depression and anxiety. The absence of a supportive partner can result in a lack of emotional and practical support, which is crucial for stress management in caregiving. (Liu et al., 2020) point out that married caregivers tend to have more social support, which buffers the impact of caregiving on their mental health. This highlights the importance of encouraging marital and social support networks for caregivers, especially those without partners.
Educational Level and Coping Skills
Education emerges as a protective factor for caregiver mental health. As demonstrated by (Liu et al., 2020), caregivers with higher education levels tend to experience lower levels of stress, likely because they possess a better understanding of dementia and caregiving techniques. Educated caregivers are more likely to have access to resources, healthcare knowledge, and social support, all of which contribute to better coping mechanisms. This finding suggests that interventions aimed at improving caregiver knowledge—such as education on dementia, caregiving strategies, and mental health—could significantly reduce caregiver burden and improve mental health outcomes. Education also enhances caregivers' ability to navigate the healthcare system, ensuring they receive the necessary support for both the patient and themselves.
Social Isolation and Support Systems
Social isolation is one of the most significant risk factors for caregiver mental health deterioration. (Shikimoto et al., 2018) emphasized the role of social networks in alleviating caregiver burden. Caregivers who have access to strong support systems, whether through family, friends, or community resources, tend to experience less anxiety and depression compared to those who are isolated. Support networks offer emotional validation, practical assistance, and respite from caregiving duties, all of which contribute to reduced stress. However, caregivers who lack these networks are at an increased risk of burnout, leading to a decline in mental health. (Etters et al., 2008)further pointed out that formal support, such as respite care and counselling, can play a critical role in preventing caregiver burnout. This underscores the need for policy initiatives aimed at providing accessible, effective support systems for caregivers.
Limitations
While the studies reviewed provide valuable insights into the factors affecting caregiver mental health, several limitations must be acknowledged. First, many of the studies were cross-sectional in nature, making it difficult to establish causal relationships between caregiving and mental health outcomes. Longitudinal studies would provide more robust evidence of the long-term effects of caregiving on mental health and how these effects evolve over time. Second, the studies varied in their measurement of caregiver mental health, with some focusing on specific psychological outcomes (e.g., anxiety or depression) while others examined broader constructs such as stress or burden. This variability in outcomes makes direct comparisons across studies challenging. Additionally, the cultural context of caregiving was not consistently addressed in all studies. The caregiving experience is deeply influenced by cultural norms, and the findings from Western contexts may not fully apply to other regions, such as Asia or Africa, where caregiving dynamics and societal expectations may differ. Future research should explore the cultural dimensions of caregiving and how they influence mental health outcomes, especially in non-Western countries. Finally, the majority of studies focused on primary caregivers, often neglecting the experiences of secondary caregivers or those providing care in institutional settings. While primary caregivers tend to bear the most significant mental health burden, secondary caregivers or institutional staff may also experience distress and burnout. Expanding the focus to include these groups could provide a more comprehensive understanding of caregiver mental health.
Conclusion
In conclusion, the mental health of dementia caregivers is influenced by a wide array of factors, including age, gender, marital status, education, and social support. Caregivers who are younger, female, or socially isolated are particularly vulnerable to mental health challenges, including anxiety and depression. In contrast, caregivers who are older, better educated, and supported by strong social networks tend to fare better. These findings underscore the importance of designing interventions that are tailored to the unique needs of caregivers based on their demographic characteristics and available support systems. Efforts to reduce caregiver burden should focus on providing educational resources, improving access to social support, and developing policies that offer practical and emotional assistance to caregivers. Future research should aim to address the limitations of existing studies, particularly by incorporating longitudinal designs, exploring cultural differences, and considering a broader range of caregivers.
Conflict of Interest
“No potential conflict of interest relevant to this article was reported”.
References
- Baharudin, A. D., Din, N. C., Subramaniam, P., Razali, R. (2019). The associations between behavioral-psychological symptoms of dementia (BPSD) and coping strategy, burden of care and personality style among low-income caregivers of patients with dementia. BMC Public Health, 19(4):447.
Publisher | Google Scholor - Becerra Carrillo, N., Guasconi, M., Barello, S. (2024). The Impact of Caregiver Affiliate Stigma on the Psychosocial Well-Being of Caregivers of Individuals with Neurodegenerative Disorders: A Scoping Review. Healthcare, 12(19):Article 19.
Publisher | Google Scholor - Brodaty, H., Donkin, M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2):217.
Publisher | Google Scholor - Dementia. (n.d.). ( 2024).
Publisher | Google Scholor - Etters, L., Goodall, D., Harrison, B. E. (2008). Caregiver burden among dementia patient caregivers: A review of the literature. Journal of the American Academy of Nurse Practitioners, 20(8):423-428.
Publisher | Google Scholor - Garand, L., Lingler, J. H., Deardorf, K. E., DeKosky, S. T., Schulz, R., et al. (2012). Anticipatory Grief in New Family Caregivers of Persons with Mild Cognitive Impairment and Dementia. Alzheimer Disease and Associated Disorders, 26(2):159.
Publisher | Google Scholor - Goren, A., Montgomery, W., Kahle-Wrobleski, K., Nakamura, T., Ueda, K. (2016). Impact of caring for persons with Alzheimer’s disease or dementia on caregivers’ health outcomes: Findings from a community based survey in Japan. BMC Geriatrics, 16(1):122.
Publisher | Google Scholor - Kim, J. S., Kim, E. H., An, M. (2016). Experience of Dementia-related Anxiety in Middle-aged Female Caregivers for Family Members with Dementia: A Phenomenological Study. Asian Nursing Research, 10(2):128-135.
Publisher | Google Scholor - Liu, C.-C., Lee, C.-F., Chang, T., Liao, J.-J. (2020). Exploring the Relationship between the Caregiver’s Stress Load and Dementia Patient Behavior: A Case Study of Dementia Specialist Outpatient Data from the Southern Medical Center of Taiwan. International Journal of Environmental Research and Public Health, 17(14):4989.
Publisher | Google Scholor - Park, M., Choi, S., Lee, S. J., Kim, S. H., Kim, J., et al. (2018). The roles of unmet needs and formal support in the caregiving satisfaction and caregiving burden of family caregivers for persons with dementia. International Psychogeriatrics, 30(4):557-567.
Publisher | Google Scholor - Park, M., Nari, F., Kang, S. H., Jang, S.-I., Park, E.-C. (2021). Association between Living with Patients with Dementia and Family Caregivers’ Depressive Symptoms-Living with Dementia Patients and Family Caregivers’ Depressive Symptoms. International Journal of Environmental Research and Public Health, 18(8):4372.
Publisher | Google Scholor - Pinyopornpanish, M., Pinyopornpanish, K., Soontornpun, A., Tanprawate, S., Nadsasarn, A., et al. (2021). Perceived stress and depressive symptoms not neuropsychiatric symptoms predict caregiver burden in Alzheimer’s disease: A cross-sectional study. BMC Geriatrics, 21(1):180.
Publisher | Google Scholor - Shaji, S., Promodu, K., Abraham, T., Roy, K. J., Verghese, A. (1996). An epidemiological study of dementia in a rural community in Kerala, India. The British Journal of Psychiatry: The Journal of Mental Science, 168(6):745-749.
Publisher | Google Scholor - Sharma, M. G., Popli, H. (2023). Challenges for Lower-Middle-Income Countries in Achieving Universal Healthcare: An Indian Perspective. Cureus, 15(1):e33751.
Publisher | Google Scholor - Shikimoto, R., Sado, M., Ninomiya, A., Yoshimura, K., Ikeda, B., et al. (2018). Predictive factors associated with psychological distress of caregivers of people with dementia in Japan: A cross-sectional study. International Psychogeriatrics, 30(8):1089-1098.
Publisher | Google Scholor - Shim, S. H., Kang, H. S., Kim, J. H., Kim, D. K. (2015). Factors Associated with Caregiver Burden in Dementia: 1-Year Follow-Up Study. Psychiatry Investigation, 13(1):43.
Publisher | Google Scholor - Sörensen, S., Conwell, Y. (2011). Issues in Dementia Caregiving: Effects on Mental and Physical Health, Intervention Strategies, and Research Needs. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry, 19(6):491.
Publisher | Google Scholor - Su, J.-A., Chang, C.-C. (2020). Association Between Family Caregiver Burden and Affiliate Stigma in the Families of People with Dementia. International Journal of Environmental Research and Public Health, 17(8):2772.
Publisher | Google Scholor - Wesson, V., Chiu, M., Feldman, R., Nelles, L. J., Sadavoy, J. (2017). Dementia and Caregiving. In H. Chiu, K. Shulman (Eds.), Mental Health and Illness of the Elderly. 515-547.
Publisher | Google Scholor - Yu, H., Wang, X., He, R., Liang, R., Zhou, L. (2015). Measuring the Caregiver Burden of Caring for Community-Residing People with Alzheimer’s Disease. PLOS ONE, 10(7):e0132168.
Publisher | Google Scholor - Yu, H., Wu, L., Chen, S., Wu, Q., Yang, Y., et al. (2016). Caregiving burden and gain among adult-child caregivers caring for parents with dementia in China: The partial mediating role of reciprocal filial piety. International Psychogeriatrics, 28(11):1845-1855.
Publisher | Google Scholor - Zhang, H., Xiong, R., Sara, H., Zhang, J., Zhang, X. (2013). Psychological distress, family functioning, and social support in family caregivers for patients with dementia in the mainland of China. Chinese Medical Journal, 126(18):3417.
Publisher | Google Scholor