Research Article
Evaluating The Effectiveness of Public Smoking Bans on Respiratory Health Outcomes in Oyo State, Nigeria
- Oluwaseun Remilekun Omole *
Department of Nursing Science, Coventry University, England, United Kingdom.
*Corresponding Author: Oluwaseun Remilekun Omole, Department of Nursing Science, Coventry University, England, United Kingdom.
Citation: Oluwaseun R. Omole. (2025). Evaluating The Effectiveness of Public Smoking Bans on Respiratory Health Outcomes in Oyo State, Nigeria. Journal of Clinical Medicine and Practice, BioRes Scientia Publishers. 2(1):1-6. DOI: 10.59657/3065-5668.brs.25.018
Copyright: © 2025 Oluwaseun Remilekun OMOLE, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 11, 2025 | Accepted: February 25, 2025 | Published: March 04, 2025
Abstract
Background: Public smoking bans are implemented globally to mitigate the adverse health effects of tobacco smoke exposure. However, limited empirical evidence exists on their effectiveness in improving respiratory health outcomes in Nigeria. This study evaluates the impact of public smoking bans on respiratory health indicators in Oyo State, Nigeria.
Methods: A quasi-experimental, cross-sectional study design was employed, incorporating retrospective and prospective data collection. The study was conducted in urban and semi-urban areas of Oyo State, including Ibadan, Ogbomoso, and Oyo town. A multi-stage sampling technique was used to recruit 400 participants aged 18 years and above, categorized into individuals with respiratory conditions and the general population. Data were obtained via structured questionnaires, medical records review, pulmonary function tests (PFTs), and environmental air quality assessment. Statistical analyses, including paired t-tests, chi-square tests, and logistic regression, were performed using SPSS version 26.0.
Results: The study revealed a significant decline in respiratory symptoms post-ban, including chronic cough (28.0% pre-ban vs. 16.0% post-ban, p less than 0.001), shortness of breath (24.5% vs. 12.3%, p less than 0.001), and wheezing (21.3% vs. 10.5%, p less than 0.001). Pulmonary function parameters showed significant improvement post-ban, with increased mean forced expiratory volume in one second (FEV1) (2.35 ± 0.75 L pre-ban vs. 2.78 ± 0.65 L post-ban, p=0.049) and forced vital capacity (FVC) (3.10 ± 0.82 L vs. 3.45 ± 0.70 L, p=0.041). Environmental air quality assessment indicated a reduction in mean particulate matter concentrations (PM2.5: 85.3 ± 12.6 µg/m³ pre-ban vs. 50.8 ± 9.2 µg/m³ post-ban, p=0.016; PM10: 140.2 ± 15.8 µg/m³ vs. 90.5 ± 10.4 µg/m³, p=0.003). Pearson correlation analysis demonstrated a significant inverse relationship between air quality improvements and respiratory health indicators (r = -0.65, p less than 0.001 for PM2.5 vs. FEV1).
Conclusion: The implementation of public smoking bans in Oyo State, Nigeria, has led to significant improvements in respiratory health outcomes, as evidenced by reduced symptoms, enhanced pulmonary function, and improved air quality. These findings underscore the necessity of sustained policy enforcement and public awareness to maximize health benefits.
Keywords: public smoking ban; respiratory health; air quality; pulmonary function; tobacco control; health policy
Introduction
Tobacco use remains a significant public health concern globally; contributing to a myriad of health complications; particularly respiratory diseases. Exposure to second-hand smoke (SHS) exacerbates these health risks; leading to increased morbidity and mortality among non-smokers. In response; many regions have implemented public smoking bans to mitigate the adverse health effects associated with SHS exposure [1]. Public smoking bans have been widely adopted as a strategy to protect individuals from the harmful effects of SHS. Evidence indicates that these bans lead to significant health benefits. For instance; a meta-analysis by Tan and Glantz [1] found that smoke-free legislation was associated with a lower rate of hospitalizations for cardiac; cerebrovascular; and respiratory diseases; with more comprehensive laws yielding larger risk reductions. Similarly; a systematic review by Frazer et al. [2] concluded that smoking bans contribute to reduced harm from SHS exposure; decreased smoking prevalence; and lower tobacco consumption. In Nigeria; tobacco use is a growing concern; particularly among adolescents. A study conducted in Oyo State revealed that 3.5% of students aged 13–15 years were current smokers; highlighting the need for effective tobacco control measures [3]. Nigeria enacted the National Tobacco Control Act in 2015 to address this issue; aligning with the World Health Organization's Framework Convention on Tobacco Control. This legislation prohibits smoking in public places; bans all forms of tobacco advertising; and restricts sales to minors; among other measures [4].
The implementation of public smoking bans has been associated with improvements in respiratory health outcomes. A study in Norway reported a significant decrease in respiratory symptoms among hospitality workers following the introduction of a total indoor smoking ban [5]. Similarly; research in Geneva; Switzerland; observed reductions in hospital admissions for respiratory diseases after the enforcement of a public smoking ban [6]. These findings suggest that smoking bans can lead to immediate health benefits by reducing SHS exposure. Despite the establishment of tobacco control policies; challenges persist in Nigeria. A study assessing awareness and attitudes toward the smoking prohibition law in Osun State found that only 38% of respondents were aware of the law; and none had seen the actual document. Moreover; 56 percentage felt that cigarette smoking is a problem requiring legal intervention; but only 20 percentage believed that the law would stop tobacco use [4]. These findings underscore the need for increased public sensitization and effective enforcement of smoking bans. Oyo State presents a unique context for evaluating the effectiveness of public smoking bans on respiratory health outcomes. Given the prevalence of smoking among adolescents and the existing challenges in policy enforcement; it is crucial to assess whether the smoking ban has led to measurable health improvements. This study aimed to evaluate the effectiveness of such bans on respiratory health outcomes in Oyo State; Nigeria.
Materials And Methods
Study Design
This study adopted a quasi-experimental; cross-sectional design to evaluate the impact of public smoking bans on respiratory health outcomes in Oyo State; Nigeria. The research involved a combination of retrospective and prospective data collection to assess changes in respiratory health indicators before and after the enforcement of public smoking bans.
Study Area
The study was conducted in Oyo State; Nigeria; with a focus on urban and semi-urban areas where public smoking bans have been implemented. Key locations used in this study included Ibadan; Ogbomoso; and Oyo town with high population densities and active enforcement of smoking regulations.
Study Population
The target population included individuals aged 18 years and above; residing in Oyo State for at least five years. The study population comprised two major groups: (i) individuals with a history of respiratory conditions such as asthma; chronic obstructive pulmonary disease (COPD); or bronchitis; and (ii) the general population; including non-smokers and former smokers.
Sample Size Determination
The sample size was determined using Cochran’s formula for cross-sectional studies
where: n = required sample size; Z = standard normal deviation at a 95% confidence level (1.96); p = estimated prevalence of respiratory conditions in the study area (assumed at 20%); d = margin of error (set at 5%).
Adjustments for a 10% non-response rate were included; resulting in a final sample size of approximately 400 participants.
Sampling Technique
A multi-stage sampling technique was employed
Stage 1: Selection of local government areas (LGAs) with active public smoking bans using stratified random sampling.
Stage 2: Random selection of wards from the chosen LGAs.
Stage 3: Systematic sampling of households within the selected wards.
Stage 4: Simple random sampling of eligible participants within households.
Data Collection Methods
Questionnaire Administration
A structured questionnaire was developed and administered to collect demographic data; smoking exposure history; self-reported respiratory symptoms; and awareness of the smoking ban. The questionnaire was pre-tested on 5% of the sample population for validity and reliability.
Medical Records Review
Retrospective hospital records from selected health facilities were reviewed to assess trends in respiratory-related hospital visits and diagnoses before and after the ban.
Pulmonary Function Tests (PFTs)
Spirometry tests were conducted on participants with suspected respiratory impairments to measure forced expiratory volume in one second (FEV1) and forced vital capacity (FVC); using American Thoracic Society (ATS) guidelines as outlined by Orji et al. [7].
Air Quality Assessment
Environmental air quality data were obtained from regulatory agencies and monitored using portable air quality sensors to measure particulate matter (PM2.5; PM10) in public spaces.
Data Analysis
Data were analyzed using SPSS (Statistical Package for the Social Sciences) version 26.0. Descriptive statistics such as means; standard deviations; and frequencies were used to summarize data. Inferential statistics; including paired t-tests and chi-square tests; were used to compare pre-and post-ban respiratory health indicators. Logistic regression models were employed to identify associations between public smoking bans and respiratory health outcomes; adjusting for potential confounders such as age; occupation; and previous smoking exposure.
Ethical Considerations
Written informed consent was obtained from all participants; and confidentiality of responses was strictly maintained.
Limitations
Potential limitations of the study included reliance on self-reported data; possible recall bias; and variations in enforcement levels of the smoking ban across different locations. Efforts were made to mitigate these by incorporating objective measures such as air quality assessments and spirometry tests.
Results
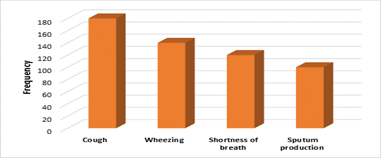
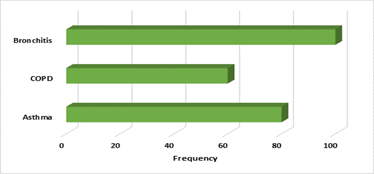
The study included 400 participants with a balanced distribution across different age groups. Most participants were between 31–45 years (31.5%); followed by those aged 46–60 years (24.5%) and 18–30 years (24.0%). The majority were male (52.5%); while females accounted for 47.5%. In terms of occupation; nearly half (49.5%) were employed; 36.2% were self-employed; and 14.3% were unemployed. Smoking history indicated that 62.5% had never smoked; while 18.8% were former smokers and an equal percentage were current smokers (Table 1). Regarding smoking exposure; 50% of participants were classified as non-smokers; 30% as former smokers; and 20% as current smokers. Notably; more than half (55.0%) reported exposure to second-hand smoke. Among smokers; 12.5% had smoked for less than five years; 22.5% for 5–10 years; and 15.0% for more than ten years (Table 2). Respiratory symptoms were prevalent among participants; with 45.0% reporting cough; 35.0% wheezing; 30.0% shortness of breath; and 25.0% sputum production (Figure 1). Diagnosed respiratory conditions included bronchitis (25.0%); asthma (20.0%); and COPD (15.0%) (Figure 2).
Pulmonary function tests (PFT) showed significant improvement following the smoking ban. The mean Forced Expiratory Volume in 1 second (FEV1) increased from 2.35 ± 0.75 L to 2.78 ± 0.65 L (p = 0.049); Forced Vital Capacity (FVC) improved from 3.10 ± 0.82 L to 3.45 ± 0.70 L (p = 0.041); and the FEV1/FVC ratio increased from 0.76 ± 0.08 to 0.81 ± 0.07 (p = 0.033) (Table 3). Air quality assessment revealed a significant reduction in air pollutants after the smoking ban. PM2.5 levels decreased from 85.3 ± 12.6 µg/m³ to 50.8 ± 9.2 µg/m³ (p = 0.016); while PM10 levels dropped from 140.2 ± 15.8 µg/m³ to 90.5 ± 10.4 µg/m³ (p = 0.003) (Table 4). A significant reduction in respiratory symptoms was observed post-ban. The prevalence of chronic cough decreased from 28.0% to 16.0% (p less than 0.001); shortness of breath from 24.5% to 12.3% (p less than 0.001); and wheezing from 21.3% to 10.5% (p less than 0.001). Additionally; frequent hospital visits dropped from 34.3% to 18.8% (p less than 0.001) (Table 5). Correlation analysis demonstrated a strong negative relationship between air quality and pulmonary function. Pre-ban PM2.5 levels were negatively correlated with FEV1 (r = -0.65; p less than .001); and PM10 was negatively correlated with FVC (r = - 0.58; p = 0.002). Post-ban correlations remained significant but were weaker; with PM2.5 negatively correlated with FEV1 (r = -0.45; p = 0.007) and PM10 with FVC (r = -0.42; p = 0.010) (Table 6).
Table 1: Socio-Demographic Characteristics of Participants
| Variable | Frequency (n = 400) | Percentage (%) |
| Age Group (years) | ||
| 18-30 | 96 | 24.0 |
| 31-45 | 126 | 31.5 |
| 46-60 | 98 | 24.5 |
| >60 | 80 | 20.0 |
| Gender | ||
| Male | 210 | 52.5 |
| Female | 190 | 47.5 |
| Occupation | ||
| Unemployed | 57 | 14.3 |
| Employed | 198 | 49.5 |
| Self-employed | 145 | 36.2 |
| Smoking Status | ||
| Never Smoked | 250 | 62.5 |
| Former Smoker | 75 | 18.8 |
| Current Smoker | 75 | 18.8 |
Table 2: Smoking Exposure History
| Variable | Frequency (n = 400) | Percentage (%) |
| Smoking Status | ||
| Non-smoker | 200 | 50.0 |
| Former smoker | 120 | 30.0 |
| Current smoker | 80 | 20.0 |
| Exposure to Second-hand Smoke | ||
| Yes | 220 | 55.0 |
| No | 180 | 45.0 |
| Duration of Smoking Exposure (Years) | ||
| < 5> | 50 | 12.5 |
| 5 – 10 years | 90 | 22.5 |
| > 10 years | 60 | 15.0 |
Figure 1: Respiratory Symptoms Reported by Participants
Figure 2: Diagnosed Conditions
Table 3: Pulmonary Function Test (PFT)
| Parameter | Pre-Ban (Mean ± SD) | Post-Ban (Mean ± SD) | p-value |
| FEV1 (L) | 2.35 ± 0.75 | 2.78 ± 0.65 | 0.049 |
| FVC (L) | 3.10 ± 0.82 | 3.45 ± 0.70 | 0.041 |
| FEV1/FVC Ratio | 0.76 ± 0.08 | 0.81 ± 0.07 | 0.033 |
Data are significantly different at pless than 0.05
Table 4: Air Quality Assessment
| Parameter | Pre-Ban (Mean ± SD) | Post-Ban (Mean ± SD) | p-value |
| PM 2.5 (µg/m³) | 85.3 ± 12.6 | 50.8 ± 9.2 | 0.016 |
| PM 10 (µg/m³) | 140.2 ± 15.8 | 90.5 ± 10.4 | 0.003 |
Data are significantly different at p less than p less than 0.05; Legend: PM = Particulate Matter
Table 5: Association Between Smoking Ban and Respiratory Symptoms
| Respiratory Symptom | Pre-Ban Frequency (%) | Post-Ban Frequency (%) | Chi-Square (X2) | p-value |
| Chronic Cough | 112 (28.0%) | 64 (16.0%) | 15.7 | less than 0.001 |
| Shortness of Breath | 98 (24.5%) | 49 (12.3%) | 19.3 | less than 0.001 |
| Wheezing | 85 (21.3%) | 42 (10.5%) | 17.1 | less than 0.001 |
| Frequent Hospital Visits | 137 (34.3%) | 75 (18.8%) | 21.4 | less than 0.001 |
Data are significantly different at p less than 0.05
Table 6: Correlation Analysis (Pearson’s r) Between Air Quality and Respiratory Health Indicators
| Air Quality | Respiratory Health Indicators | Correlation Coefficient (r) | p-value |
| PM 2.5 (Pre-ban) | FEV1 (Pre-ban) | -0.65 | less than 0.001 |
| PM 10 (Pre-ban) | FVC (Pre-ban) | -0.58 | 0.002 |
| PM 2.5 (post-ban) | FEV1 (post-ban) | -0.45 | 0.007 |
| PM 10 (post-ban) | FVC (post-ban) | -0.42 | 0.010 |
Data are significantly different at p less than 0.05; Legend: PM = Particulate Matter
Discussion
The implementation of public smoking bans has been a pivotal strategy in mitigating the adverse health effects associated with tobacco smoke exposure. This study evaluates the effectiveness of such bans on respiratory health outcomes in Oyo State; Nigeria; by analyzing socio-demographic characteristics; smoking exposure history; respiratory symptoms and diagnoses; pulmonary function tests (PFTs); air quality assessments; and the association between the smoking ban and respiratory symptoms. The study's participant distribution across age groups and occupations provides a comprehensive overview of the population affected by smoking and its associated risks. Notably; 18.8% of participants identified as current smokers; while 55% reported exposure to second-hand smoke. These figures underscore the pervasive nature of smoking and passive smoke exposure within the community.
Comparable studies have highlighted similar concerns. For instance; a systematic review by Faber et al. [8] emphasized the role of public smoking bans in reducing second-hand smoke exposure; thereby decreasing smoking prevalence and initiation rates. The review concluded that such bans are instrumental in promoting public health by diminishing both active and passive smoking rates. The prevalence of respiratory symptoms among participants—45% reporting cough; 35% wheezing; and 30% shortness of breath—aligns with established data linking smoking to respiratory ailments. Diagnosed conditions such as asthma (20%); chronic obstructive pulmonary disease (COPD) (15%); and bronchitis (25%) further corroborate the detrimental impact of smoking and second-hand smoke exposure. These findings are consistent with global research. A study by Been [9]. demonstrated that the implementation of smoke-free legislation was associated with significant reductions in preterm births and hospital admissions for asthma; underscoring the positive health outcomes of such policies.
The study observed significant improvements in PFT parameters post-ban: FEV1 increased from 2.35±0.75 L to 2.78±0.65 L; FVC from 3.10±0.82 L to 3.45±0.70L; and the FEV1/FVC ratio from 0.76±0.08 to 0.81±0.07. These enhancements suggest a positive impact of the smoking ban on respiratory function. Air quality assessments revealed significant reductions in particulate matter concentrations: PM2.5 levels decreased from 85.3±12.6 µg/m³ to 50.8±9.2 µg/m³; and PM10 from 140.2 ± 15.8 µg/m³ to 90.5 ± 10.4 µg/m³. Improved air quality is directly linked to better respiratory health outcomes. These results are in line with previous studies. A systematic review by Frazer et al. [2] concluded that smoking bans lead to improved health outcomes; including reductions in hospital admissions for smoking-related diseases and improvements in biomarkers of exposure to tobacco smoke. The study found significant reductions in respiratory symptoms post-ban: chronic cough decreased from 28.0% to 16.0%; shortness of breath from 24.5% to 12.3%; and wheezing from 21.3% to 10.5%. Additionally; frequent hospital visits declined from 34.3% to 18.8%.
These findings are supported by international research. A meta-analysis by Faber et al. [8] highlighted that public smoking bans are effective in reducing exposure to second-hand smoke and associated health risks; leading to decreased respiratory symptoms and hospital admissions. The study identified significant negative correlations between particulate matter levels and pulmonary function parameters; both pre-and post-ban. This indicates that lower air pollution levels are associated with better respiratory function. This observation aligns with findings from a systematic review and meta-analysis by Tan and Glantz [1]; which reported that public smoking bans are associated with significant reductions in heart disease morbidity and mortality; suggesting broader cardiovascular and respiratory health benefits.
Conclusion
The implementation of public smoking bans in Oyo State; Nigeria; has led to significant improvements in respiratory health outcomes; as evidenced by reductions in respiratory symptoms; enhancements in pulmonary function; and improved air quality. These findings are consistent with global research; reinforcing the effectiveness of smoking bans as a public health intervention.
References
- Tan CE, & Glantz SA. (2022). Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation, 126(18):2177-2183.
Publisher | Google Scholor - Frazer K, Callinan JE, McHugh J, van Baarsel S, Clarke A, et al. (2016). Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database of Systematic Reviews, (2).
Publisher | Google Scholor - Global Youth Tobacco Survey Nigeria. (2018). World Health Organization.
Publisher | Google Scholor - Desalu,OO, Adekoya AO, & Dosumu AO. (2019). Outdoor smoking in Nigeria: prevalence, correlates and predictors. BMC Public Health, 19(1):1-8.
Publisher | Google Scholor - Skogstad M, Tynes T, Haldorsen T, & Kjuus H. (2006). Decline in respiratory symptoms in service workers five months after a public smoking ban. Tobacco Control, 15(3):242-246.
Publisher | Google Scholor - Herman PM, & Cheung K. (2014). Acute respiratory and cardiovascular admissions after a public smoking ban in Geneva, Switzerland. Plos One, 9(3):e904-917.
Publisher | Google Scholor - Orji OJ, Ijioma CE, Ekeleme NC, Uduma VU, Abali IO, et al. (2023). “Evaluation of Respiratory Symptoms and Lung Function in Car Spray Painters in Ibadan, Nigeria”. Journal of Advances in Medicine and Medical Research, 35(19):237-250.
Publisher | Google Scholor - Faber T, Kumar A, Mackenbach JP, Millett C, Basu S, et al. (2020). Effect of tobacco control policies on perinatal and child health: a systematic review and meta-analysis. The Lancet Public Health, 2(9):e420-e437.
Publisher | Google Scholor - Been JV, Nurmatov UB, Cox B, Nawrot TS, van Schayck CP, et al. (2024). Effect of smoke-free legislation on perinatal and child health: a systematic review and meta-analysis. The Lancet, 383(9928):1549-1560.
Publisher | Google Scholor