Research Article
Evaluating The Duration of Clinical Pharmacist Interventions for Drug Therapy Problems in The Intensive Care Unit
- Okeroghene Aghogho Timipre 1
- Peter A. Owonaro 1*
- Joshua Funsho Eniojukan 1
- Sounyo Adekola Owonaro 1
- Awala E. Daughter 1
- Brisibe F. Seiyefa 2
1Faculty of Pharmacy, Department of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
2College of Health Sciences, Department of Family Medicine, Niger Delta University, Amassoma, Nigeria.
*Corresponding Author: Peter A. Owonaro, Faculty of Pharmacy, Department of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
Citation: Timipre O.A., Owonaro P.A., Eniojukan J.F., Owonaro S.A., Daughter A.E., et al. (2025). Evaluating The Duration of Clinical Pharmacist Interventions for Drug Therapy Problems in The Intensive Care Unit, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 3(2):1-9. DOI: 10.59657/2997-6103.brs.25.044
Copyright: © 2025 Peter A. Owonaro, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 18, 2024 | Accepted: January 06, 2025 | Published: January 13, 2025
Abstract
This study assessed the contribution of clinical pharmacists to managing Drug Therapy Problems in the Intensive Care Unit of a tertiary hospital in South-South Nigeria. The present study aims to measure the time that, on average, the clinical pharmacist has to intervene in the DTPs in the intensive care setting, calculate the mean time spent on each kind of intervention, identify potential variables influencing this duration, and also determine what types of interventions-at pre-scriber, patient or drug level-take the most time because of better resource management in the medication management improvement in the intensive care setting. A prospective observational study design was adopted, and data collection was done in the Pharmaceutical Care Network Europe classification scheme for Drug Therapy Problems Version 9.1. In the present study, it was determined that 55 (34.4%) of the 160 patients were aged 65 years and above, 99 (61.9%) were male, and 115 (71.9%) were uninsured. More than half of the patients continued to smoke (50%) and consume alcohol (59.4%). Clinical pharmacists estimated that the DTP interventions required 15-30, 30-60, and >60 minutes in 37.5%, 34.4%, and 28.1%, respectively. Factors affecting time consumption were the availability of physicians in the ICU 41%, the number of DTPs identified 30%, cooperation from the patient/family 23.1%, and the complexity of the patient case 6.3%. Drug level was where most time-consuming interventions, 62.5%, were required. Understanding these influences optimizes resource allocation and time management to enhance pharmaceutical care, thereby improving patient outcomes in the critical care setting.
Keywords: drug therapy problems; intensive care unit; clinical pharmacist interventions; medication management; patient safety
Introduction
Drug Therapy Problems constitute one of the major challenges to healthcare delivery, especially within the complex setting of an Intensive Care Unit (Tharanon et al., 2022). The problems of drug therapy refer to any undesirable event that a patient experiences, which involves or is suspected to involve drug therapy; they have great bearing on the patients' outcomes, lengths of stay in hospitals, and costs of health care (Çakır et al., 2024). Identification and resolution by a clinical pharmacist of DTPs would, therefore, be even more important in a setting of critical care with additional multiple medications on top of complicated therapeutic regimens (Pichala et al., 2013; Al Fahmawi et al., 2018; Çakır et al., 2024). The management of critically ill patients in ICUs is always very challenging, given that most of the illnesses are very serious, with multiple organ dysfunctions, altered pharmacokinetics, and also a need for numerous medications (Short et al., 2023). These factors greatly enhance the risk of drug-related problems and make medication management particularly complex (McTavish et al., 2024; Short et al., 2023). A clinical pharmacist is an integral member of the multidisciplinary team in the ICU and has an important role in the optimization of medication therapy through various interventions at prescriber, patient, and drug levels.
Besides, the complex nature of medication management in the ICUs is compounded by the critical states of patients, the need for rapid therapeutic decisions, and the great potentials for serious consequences related to medication errors (Stollings et al., 2018). In all these, the clinical pharmacist has to strike a balance while ensuring timely and effective intervention. Such interventions, depending on the complexity of the case, the number of DTPs identified, and the degree of collaboration with other professionals in the field, can be quite different in terms of time. This is an added challenge in the Nigerian healthcare context in which this study is placed, where a high proportion of the patients are uninsured and hence their financial positions further complicate medication management because financial status may affect treatment options or the availability of medication (Oseni et al., 2023). Moreover, the prevalence of certain lifestyle factors among the patients admitted to the ICU-such as smoking and consumption alcohol-requires cautious medication therapy management (Ajibola & Fajemirokun, 2018).
However, it is shown that very few pieces of research have focused on the time factor of the interventions by clinical pharmacists, particularly in developing healthcare systems. For example, one article showed that there was a need for better documentation of interventions from the pharmacy to provide more comprehensive and safer patient care, but did not relate the aspect of time regarding the intervention (Baptista et al., 2023). Literature also shows that even as clinical pharmacists may improve patient outcomes, the duration and timing of such interventions are still less explored, particularly in resource-constrained settings (Althomali et al., 2022). This calls for a need for future research to focus on the time-related aspects of these interventions in diverse healthcare settings. The current study will fill this knowledge gap by determining the time taken by clinical pharmacists to conduct DTP interventions in the ICU setting. The analysis of the meantime taken for different kinds of interventions and identification of factors that influence these durations will be useful for resource allocation and optimization of workflows in critical care pharmacy services. This will also contribute to the growing body of evidence that will help develop more effective and efficient pharmaceutical care practices within an ICU setup, thus translating into improved patient outcomes and health care delivery/ This study consequently aims to evaluate the time taken by clinical pharmacists in conducting interventions for DTPs in the ICU, which has the dual purpose of establishing the average time taken, factors that determine the duration, and which levels of interventions at the prescriber, patient, or drug level-require more time to inform resources allocation and time management to realize better medication management practices in critical care settings.
Methods
Study Setting
This study was conducted in the dedicated Intensive Care unit of a tertiary healthcare institution that is situated in the South-South geopolitical zone of Nigeria.
Research Design
In this, the study has tried to present a prospective, observational research design to describe and document the effects and implications related to drug therapy complications.
Respondents
All those patients who have been admitted to the hospital's intensive care wards throughout the study period.
Sample Size
The study included all patients undergoing intensive care therapy during one year, from mid-2023 to mid-2024.
Data Collection
In this study, the Drug Therapy Problems were classified based on the Pharmaceutical Care Network Europe, Version 9.1 (Foppe van Mil et al., 2020; Ahmed et al., 2021). This was an extended tool for the standardized documentation and classification of drug-related problems. Background data on patients relevant to the study were also collected during data collection. The PCNE framework utilized contains five main categories, each with subcategories. The categories are, therefore, hierarchical and enable the detailed classification of medication-related problems considering that critical care patients have pharmaceutical challenges as these patients usually have multiple comorbid conditions requiring the management of multifaceted medication.
Quality Assurance Measures
The reliability and validity of the tool were tested by two known pharmaceutical experts, academicians, and researchers. Besides, face validity testing by the experts was carried out to ensure that the instrument would actually measure what it was intended for.
Ethical Compliance
Written permission was obtained from the medical research ethics committee of the institution, before the research that the research methods and procedures were in line with the approved guidelines on ethics.
Results
Demographics of Sampled Patients
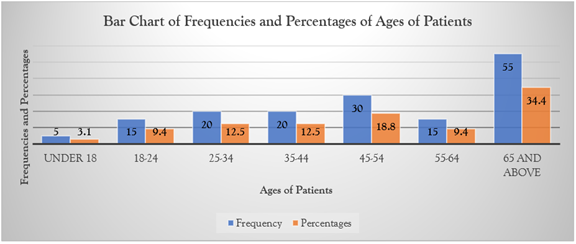
Figure 1: Bar Chart of Ages of Respondents.
Analysis of the patient age distribution showed that among the 160 participants, only 5 patients (3.1%) were minors under 18. Young adults aged 18-24 comprised 15 patients (9.4%), while 20 individuals (12.5%) fell within the 35-44 age bracket. The middle-aged group of 45-54 years included 30 patients (18.8%), and 15 patients (9.4%) were between 55-64 years old. The biggest proportion was the elderly, aged 65 years and above, with 55 patients constituting 34.4% of the entire population under study.
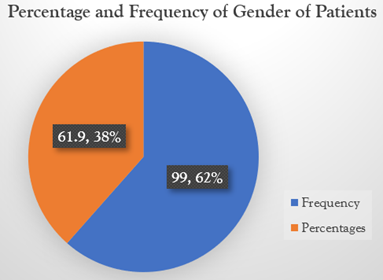
Figure 2: Gender of Patient.
Analysis of gender distribution for ICU patients indicates a significant male dominance with 99 patients being male accounting for 61.9% as opposed to 61 female patients who accounted for 38.1% and took part in the administration of the questionnaire.
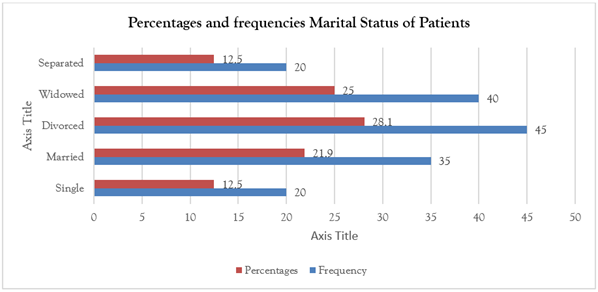
Figure 3: Marital Status.
Marital Status Distribution in the 160 ICU patients, the largest portion belonged to divorced status, which totaled 45 (28.1%), followed by the widowed status with 40 (25.0%). Married patients accounted for 35 cases, representing 21.9%, and the statuses of single and separated statuses each had 20 cases, accounting for 12.5% of patients. Aggregating these together, patients with a lost marriage status - the divorced and widowed - make up the dominant population of the research.
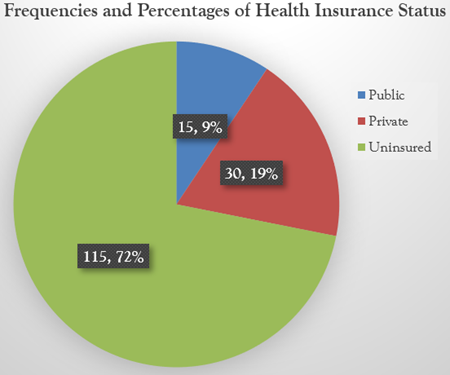
Figure 4: Health Insurance Status.
The analysis of insurance coverage showed a disturbing trend: 115 patients, or 71.9%, had no health insurance at all. Only a few patients were covered: 30, or 18.8%, had private health insurance, and just 15 patients, or 9.4%, were on public insurance. This high level of uninsured patients reflects a critical gap in healthcare access and may put them at higher health risks and financial burdens in times of medical need.
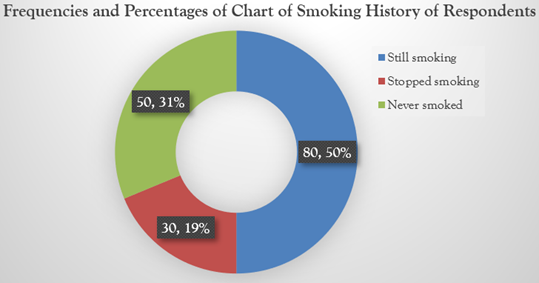
Figure 5: Smoking History.
It is clear from the smoking patterns observed among the study participants: half of the patient population, 80 patients or 50.0%, were current smokers; while 30 patients, or 18.8%, reported having quit smoking. Fifty patients, 31.3%, reported never smoking. The predominance of active smokers in the population exposes them to a myriad of clinical concerns, where the presence of tobacco may complicate certain modes of treatment and increase their susceptibility to DTPs will compromise therapeutic outcomes.
Analysis of the history of drinking showed the alarming situation of 95 current drinkers, which accounts for 59.4%, whereas 28 patients, 17.5%, had stopped drinking alcohol. The remaining 37 patients, 23.1%, had never consumed alcohol. The high prevalence of active alcohol use among ICU patients is a serious clinical challenge; continued alcohol intake may interfere with the effectiveness of treatment, increase the risk for DTPs, and thus potentially compromise patient care outcomes.
Figure 7: Time Taken for the Clinical Pharmacist to Conduct Each DTP Intervention.
Time analysis of clinical pharmacist DTP interventions showed that the highest number, 60 pharmacists (37.5%), completed their interventions within a time frame of 15-30 minutes, followed by 55 pharmacists (34.4%) who took 30-60 minutes. The remaining 45 pharmacists (28.1%) needed more than 60 minutes to complete their interventions. These findings support the potential delay in the delivery of interventions, given that most cases fall into the range of 15-60 minutes, thus indicating further optimization of interventions in an ICU setting.
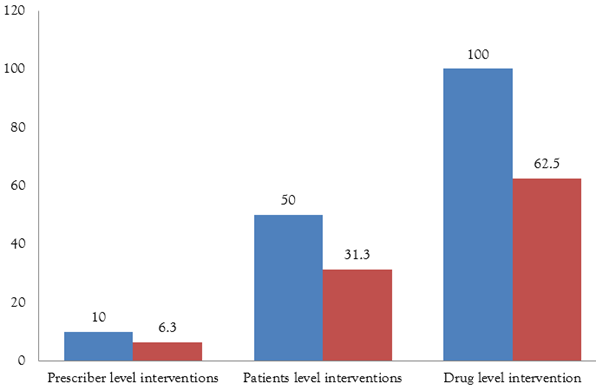
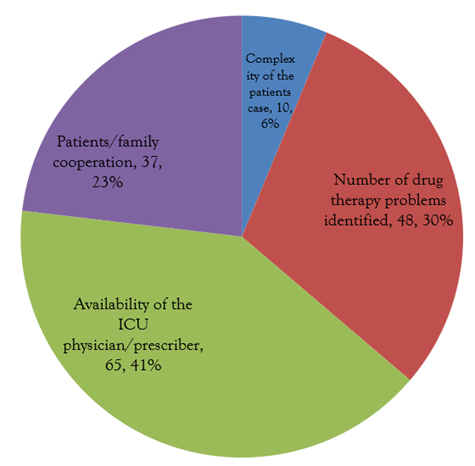
Figure 8: Factors That Influenced the Duration of the DTP Interventions.
Factors affecting the duration of the DTP interventions pointed to several challenges: the first factor was the availability of physicians or prescribers to the ICU, noted by 65 respondents (40.6%), followed by several drug therapy problems from 48 respondents (30.0%). The factor of patient and family non-cooperation affected 37 cases, or 23.1%, whereas case complexity was the least mentioned factor, cited by only 10 respondents, or 6.3%. These findings bring out that prescriber availability represents the most significant barrier to timely DTP interventions.
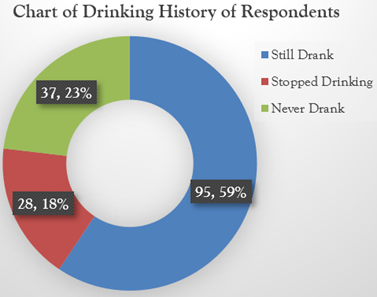
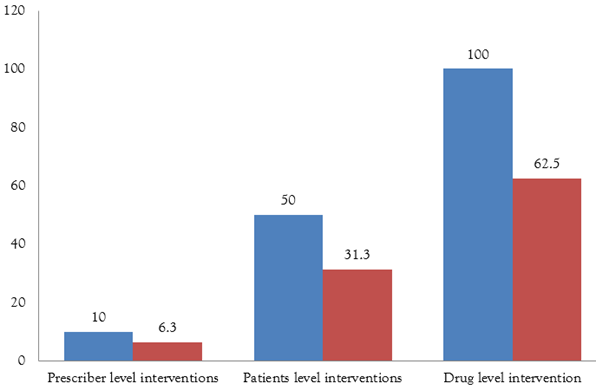
Figure 9: Interventions that Took More Time.
Analysis of time-consuming DTP interventions showed that drug-level interventions were the most time-consuming, with 100 cases constituting 62.5%, while patient level accounted for 50 cases, 31.3%, and prescriber level had the least with only 10 cases accounting for 6.3%. These clearly show that the most time is invested in drug-level interventions by the clinical pharmacist in the ICU.
Discussion
Role of Pharmacists in the Clinical Setting-ICU
This was further shown in a study conducted in the ICU of a tertiary hospital in South-South Nigeria, where clinical pharmacists were established to be very important in the management of Drug Therapy Problems. The environment of the ICU is particularly complicated, as patients usually have multiple health complications that need critical attention regarding medication management (Dionisi et al., 2022). It has been emphasized that medication and pharmaceutical care involve guardians of safety, which is being specifically tailor-made to address the needs of individual patients (Patil et al., 2023). The study presents in detail the complexity involved with pharmaceutical care, which in itself involves timing and intervention classification. Most importantly, drug-level interventions are the hallmark of 62.5% of all the cases, showcasing thereby that the pharmacists are very much on board with medication-specific challenges like dose adjustment, interactions management, and adverse effect monitoring. Such broad pharmaceutical follow-ups are necessary for avoiding complications and ensuring treatment success in the best possible way (Sebastian et al., 2020). Indeed, this is supported by the study of Li et al. (2020), where 81.7% of the interventions of pharmacists were at a drug level, with specific activities predominant in dosage and drug selection. This then means most of their concentration is on the drug level, hence supporting the claim of them being time-consuming. Another study reported that 97.2% of the interventions were at the drug level, clearly underlining drug-related issues as the target for resolution, which generally requires a significant amount of pharmacists' time (Çakır et al., 2024).
Pharmacist Interventions and Time Management
A key finding of this study is the considerable amount of time dedicated to conducting these interventions. The majority of clinical pharmacists reported that it took them between 15-30 minutes (37.5%) to conduct DTP interventions, while others indicated durations of 30-60 minutes (34.4%) and more than 60 minutes (28.1%). These figures denote the complexity and need for interventions in a critical care setting whereby pharmacists have to keenly observe and institute changes in treatment plans if optimum results are to be achieved for the patients. Time management and resource allocation therefore become key in facilitating timely intervention by the pharmacist without compromising on quality. This also reflects that the interventions being conducted by pharmacists are time-consuming, suggesting identification and solution of medication-related problems extend to long-term patient care planning and monitoring.
Factors Influencing Intervention Duration
The study outlines various factors that affect DTPs' time to intervention. The availability of physicians or prescribers in the ICU was listed by 40.6% of respondents as the factor critical to affecting the time of intervention. This, therefore, points toward timely collaboration and accessibility of medical professionals to facilitate quick decision-making and implementation of necessary changes in drug therapy (Tharanon et al., 2022). The presence and responsiveness of prescribers in the ICU setting, when patient conditions can change rather quickly, are important features that enable pharmacists to make timely and effective interventions.
For 30% of the participants, the number of drug therapy problems identified was the most influential factor in the duration of intervention. Pharmacists need to spend more time critically analyzing each problem and making a detailed plan for the resolution when the patients have multiple DTPs (Çakır et al., 2024). Patient and family cooperation was also stated to be an important determinant for the duration of intervention by 23.1% of the participants (Alharbi et al., 2023). Medico-nursing education about the management of medicines and involving the patient and family in decision-making increased their cooperation, thus reducing the time of intervention (Hanggamara et al., 2022; Sim et al., 2024). Although less reported, case complexity accounted for 6.3%, which also adds up to the longer times of interventions, since critically ill patients mostly present with many comorbidities, thus comprehensive medication management.
Demographic Influences on DTPs
The demographic analysis provided data on the population in the ICU, and one predominant feature is the high rate of uninsured patients, comprising 71.9% of the study population. This is a lack of insurance which will significantly affect access to much-needed medications and follow-up care, putting them at a higher risk for DTPs. Second, the financial burden could limit the patient from pursuing the prescribed regimen appropriately leading to suboptimal outcomes and complications.
Lifestyle factors also played a role in the patient population, as 50% of patients were still smoking and 59.4% were still drinking. These factors could complicate the management of drug therapy because of the possible effects of smoking and alcohol intake on drug metabolism and action, thus affecting the adjustment of medication. Pharmacists should take note of these variables when devising intervention strategies so that they are comprehensive and effective. Such modalities, by offering patient education and support with lifestyle issues, have been shown to significantly help with health improvement and in some cases avoid DTP incidents.
Implications for Healthcare Systems
The findings of this study have wider ramifications for health systems, particularly in resource-poor settings. From this, greater support and investment in pharmaceutical care services that are clinically pharmacist-led are suggested. DTP interventions can be significantly improved with increased availability and responsiveness from ICU physicians and further strengthening interprofessional collaboration. Such medication management processes should also ensure that healthcare systems engage the patient and family in priority to increase cooperation and decrease times of intervention.
The findings from the research identify significant challenges in the healthcare system that call for strategic intervention. High levels of uninsured patients and lifestyle-related health risks have emerged as key areas needing reform. The healthcare institutions should hence provide comprehensive solutions that shall enhance the accessibility and affordability of healthcare while instituting effective programs aimed at behavioral risk factors. This will go a long way in enhancing systemic improvements in the delivery of critical care for improved patient outcomes within intensive care settings.
Conclusion
This study effectively estimated the time that clinical pharmacists need to address DTPs in the ICU, finding that drug-level interventions, which require a great amount of time, are the most prevalent. The results have pointed out the important modifying role of factors such as the availability of physicians in the ICU and the complexity of the cases regarding time spent on interventions. These influences being understood would provide opportunities for healthcare facilities to ensure better resource utilization and develop improved strategies for time management, thus enhancing the effectiveness of pharmaceutical care and improving patient outcomes related to critical care.
Recommendations
In light of the findings, healthcare facilities should provide easy access to ICU physicians to collaborate with the clinical pharmacist promptly and reduce the duration of intervention. Patient and family education regarding the necessity of medication management will improve collaboration and facilitate the intervention process in a smoother and less time-consuming manner. Systemic barriers include no insurance coverage and lifestyle risk factors that are highly prevalent; medication management cannot be effectively practiced. These health system strategies will completely optimize the role of the clinical pharmacist, further improving patients' outcomes and resource utilization in the intensive care setting.
Public Health Implication
DTPs that are not corrected during the stay in an ICU contribute to extended stays in the hospital, adding to healthcare costs and, therefore increasing mortality rates. Healthcare systems' efforts to support and maximize the role of a clinical pharmacist in solving problems associated with medication use will, ultimately, contribute to an improved quality of care overall, promoting patient safety in a critical environment. Insights gained during this study should be useful to inform resource allocation and policy decisions related to supporting the clinical pharmacist's role in the management of medications.
This also can be enhanced in the capacity of healthcare systems through investment in the training and development of clinical pharmacists and the fostering of collaborative healthcare environments. If integration into a healthcare team were to be a priority of health systems, then their expertise may well improve patient outcomes help reduce healthcare costs generally, and enhance the quality of care in critical care settings.
Author's Conflict of Interest
The authors declare no conflict of interest.
References
- Ahmed, K. O., Muddather, H. F., Yousef, B. A. (2021). Pharmaceutical Care Network Europe (PCNE) Drug-Related Problems Classification Version 9.1: First Implementation in Sudan. Journal of Pharmaceutical Research International, 33(59A):699-706.
Publisher | Google Scholor - Al Fahmawi, H., Albsoul-Younes, A., Saleh, M., Abu-Abeeleh, M., Kasabri, V. (2024). Drug Therapy Problems Identified by Clinical Pharmacists at A General Surgery Ward of An Academic Referral Hospital in Jordan. Therapeutics and Clinical Risk Management, 619-631.
Publisher | Google Scholor - Alharbi, K. K., Arbaein, T. J., Alzhrani, A. A., Alzahrani, A. M., Monshi, S. S., et al. (2023). Factors Affecting the Length of Stay in the Intensive Care Unit among Adults in Saudi Arabia: A Cross-Sectional Study. Journal of Clinical Medicine, 12(21):6787.
Publisher | Google Scholor - Althomali, A., Altowairqi, A., Alghamdi, A., Alotaibi, M., Althubaiti, A., et al. (2022). Impact of Clinical Pharmacist Intervention on Clinical Outcomes in The Critical Care Unit, Taif City, Saudi Arabia: A Retrospective Study. Pharmacy, 10(5):108.
Publisher | Google Scholor - Ajibola, S. S., Timothy, F. O. (2018). The Influence of National Health Insurance on Medication Adherence Among Outpatient Type 2 Diabetics in Southwest Nigeria. Journal of Patient Experience, 5(2):114-119.
Publisher | Google Scholor - Baptista, R., Williams, M., Price, J. (2023). Improving The Impact of Pharmacy Interventions in Hospitals. BMJ Open Quality, 12(4):e002276.
Publisher | Google Scholor - Cakir, A., Memis, H., Gun, Z.U., Biçakcioglu, M. (2024). Evaluation of Drug-Related Problems of Intensive Care Unit Patients by Clinical Pharmacists: A Retrospective Study. Turkish Journal of Pharmaceutical Sciences, 21(4):274.
Publisher | Google Scholor - Dionisi, S., Giannetta, N., Liquori, G., De Leo, A., D’Inzeo, V., et al. (2022). Medication Errors in Intensive Care Units: An Umbrella Review of Control Measures. In Healthcare. 10(7):1221.
Publisher | Google Scholor - Foppe van Mil, J. W., Horvat, N., Westerlund, T., Richling, I. (2020). Classification for Drug-Related Problems (V9.1). Pharmaceutical Care Network Europe Association.
Publisher | Google Scholor - Hanggamara, J. S. D., Felinia, L., Witak, P. S., Eka, N. G. A., Zega, W. S. H. (2022). Promoting Civility in Nursing Education and Practice: A Systematic Literature Review. Malahayati International Journal of Nursing and Health Science, 5(2):124-135.
Publisher | Google Scholor - Li, X. X., Zheng, S. Q., Gu, J. H., Huang, T., Liu, F., et al. (2020). Drug-Related Problems Identified During Pharmacy Intervention and Consultation: Implementation of An Intensive Care Unit Pharmaceutical Care Model. Frontiers in Pharmacology, 11:571906.
Publisher | Google Scholor - MacTavish, P., Quasim, T., Purdie, C., Ball, M., Barker, L., et al. (2020). Medication-Related Problems in Intensive Care Unit Survivors: Learning from A Multicenter Program. Annals of the American Thoracic Society, 17(10):1326-1329.
Publisher | Google Scholor - Oseni, T. I. A., Blankson, P. K., Dele-Ojo, B. F., Duodu, F., Echieh, C. P., et al. (2023). Medication Adherence and Blood Pressure Control: A Preliminary Assessment of The Role of Health Insurance in Nigeria and Ghana. SAGE Open Medicine, 11:20503121231152324.
Publisher | Google Scholor - Patil, S. J., Ambulkar, R., Kulkarni, A. P. (2023). Patient Safety in Intensive Care Unit: What Can We Do Better? Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine, 27(3):163.
Publisher | Google Scholor - Pichala, P. T., Kumar, B. M., Zachariah, S., Thomas, D., Saunchez, L., et al. (2013). An Interventional Study on Intensive Care Unit Drug Therapy Assessment in A Rural District Hospital in India. Journal of Basic and Clinical Pharmacy, 4(3):64.
Publisher | Google Scholor - Sebastian, S., Justin, S., Athira, P. S., Daniel, L., Sathyamurthy, G., et al. (2020). Role of Clinical Pharmacist in Medication Management of Inotropes and Vasopressors in Intensive Care Unit. Indian Journal of Pharmacy Practice, 13(2):139.
Publisher | Google Scholor - Sim, J.E., Yang, Y.S., Jeong, Y.J., Park, S.H., Park, B.S. (2024). The Effectiveness of Domestic Elderly Nursing Simulation Education over the Past Decade. The Korean Society for Health and Nursing Convergence.
Publisher | Google Scholor - Short, A., McPeake, J., Andonovic, M., McFee, S., Quasim, T., et al. (2023). Medication-Related Problems in Critical Care Survivors: A Systematic Review. European Journal of Hospital Pharmacy, 30(5):250-256.
Publisher | Google Scholor - Stollings, J. L., Bloom, S. L., Wang, L., Ely, E. W., Jackson, J. C., et al. (2018). Critical Care Pharmacists and Medication Management in An ICU Recovery Center. Annals of Pharmacotherapy, 52(8):713-723.
Publisher | Google Scholor - Tharanon, V., Putthipokin, K., Sakthong, P. (2022). Drug-Related Problems Identified During Pharmaceutical Care Interventions in An Intensive Care Unit at A Tertiary University Hospital. SAGE Open Medicine, 10:20503121221090881.
Publisher | Google Scholor