Research Article
Determinants of Low Fifth-Minute Apgar Score Among Newborn: A Case Control Study in North Shewa Zone Public Hospitals, Central Ethiopia: A Case Control Study
- Teshome Ketema Sime *
- Yilma Jangule Tadesse
- Buta Adugna
Salale University, College of Health Sciences, Fitche, Ethiopia.
*Corresponding Author: Teshome Ketema Sime, Salale University, College of Health Sciences, Fitche, Ethiopia.
Citation: Sime TK, Tadesse YJ, Adugna B. (2025). Determinants of low fifth-minute APGAR score among newborn: A case control study in north shewa Zone public hospitals, Central Ethiopia: A case control study. Journal of Clinical Paediatrics and Child Health Care, BioRes Scientia Publishers. 2(1):1-13. DOI: 10.59657/2997-6111.brs.25.012
Copyright: © 2025 Teshome Ketema Sime, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 17, 2024 | Accepted: December 30, 2024 | Published: January 03, 2025
Abstract
Objectives: The study aimed to assess the determinants of low fifth-minute APGAR score among newborn delivered at hospitals in north shewa, Oromia, Ethiopia, 2023
Design and settings: A facility based unmatched case-control study was conducted among 411 newborns was conducted from March 30 to April 30, 2023, in North Shoa Zone public hospitals. Participants: 147 Newborns with 5th APGAR score less than 7 were considered as cases whereas 293 Newborns presented with 5th APGAR score greater than 7 were considered as controls. A consecutive sampling technique was employed to recruit cases, while a systematic random sampling technique was used to select controls. A pretested structured questionnaire through a face-to-face interview, a mother's medical records review, and observational checklist were used to collect data. The AOR with a 95 % confidence level were performed. Finally, variables with P < 0.05 were considered statistically significant.
Outcome measures: The medical charts of participants were used to recruit cases and controls.
Results: Anemia [AOR = 2.4, 95% CI: 1.76–3.04], low birth weight [AOR = 2.4, 95% CI: 1.54–3.08], twin pregnancy [AOR = 1.7, 95% CI: 1.23–2.17], and absence of ANC follow up [AOR = 1.6, 95% CI: 1.02–2.18] were revealed as significant predictors of low Apgar score.
Conclusions: A low fifth minute Apgar score was associated with low birth weight, antepartum hemorrhage, twin pregnancy, and not receiving ANC follow-up. It will be easier to identify high-risk pregnancies that result in low Apgar scores if pregnant women get effective health education on anemia during pregnancy, twin pregnancy, low birth weight and ANC before getting pregnant.
Keywords: 5th minute; newborn; apgar score; determinant; ethiopia
Introduction
Neonate is a period from birth to the first 28 days of life which is classified as early neonate for the first three weeks of life after delivery, whereas late neonate refers to the final three weeks [1]. APGAR score is an American pediatric growth assessment record used to rapidly and simply evaluate the newborn's health just after birth. A grade of zero to two is given to each five vital signs parameters developed by virginia. The resultant APGAR score is between zero and ten [2]. The scoring systems contain five parameters with each of them holding 0-2 points. These parameters are Activity, Pulse, Grimace, Appearance, and Respiration. It is interpreted as a Low APGAR score of 0-3 - Moderate APGAR score of 4-6 & Normal APGAR score of 7-10. A newborn with an APGAR score of fewer than 7 needs special attention [1]. Newborn who has a low score at 1 minute and a normal score at 5 minutes should not have any long-term problems while the vice versa exposes the neonate to different long-term problems [3]. Globally, 2.6 million children under the age of five and around 7,000 newborns died in the first month of birth, with the majority of these deaths occurring in the first few weeks. Neonatal mortality has a significant influence on under-five mortality [4]. The Sustainable development Goal (SDG) in South-East Asia aims to reduce newborn mortality to at least 12 per 1000 live births by 2030, only accounting for about one-third of neonatal fatalities in 2018 [5]. A poor APGAR score at 5 minutes was significantly linked with neonatal mortality [6,7]. Low APGAR score accounting for 100–250/1000 live births as compared to 5–10/1000 live births in developed countries. Currently, 1 in every 30 children in Ethiopia dies within the first month which is still significant [5]. In the United States, cohort studies have shown a high correlation between low APGAR scores and neonatal mortality, as seen by the 0.06% overall neonatal mortality rate and the 0.2% infant mortality rate [11]. Several studies have shown that a low fifth-minute APGAR score is linked to greater mortality rates, lower IQ scores, and a higher chance of arterial septal defect [12–14].
The risk of recurrence of a low APGAR score in the subsequent pregnancy was 1.1% [15,16]. So, more attention should be given to providing crucial newborn care & promptly determining the newborn APGAR score concerned with reducing neonatal mortality. A hospital-based retrospective case-control study with 277 medical records showed that 42 of the 79 newborns with a 5-minute APGAR score of less than 7 have died [17]. Despite having adequate resuscitation 13.8% of neonates died making up 28.72% of all neonates who died due to low APGAR score at 5 minutes. This shows that even after having an efficient resuscitation, newborns with poor APGAR scores are still at a higher risk of perinatal morbidity and death [18]. The odds of a low APGAR score at 5 minutes are significantly correlated with obstetric factors such as antepartum hemorrhage, pregnancy-induced hypertension, anemia, heart disease, diabetes mellitus, birth injury, caesarian delivery, prolonged second stages of labor, and severe birth asphyxia [19,20]. Despite many studies has been conducted in our setup, to the knowledge of the author no study conducted in the area and no Previous study examined the effect of common medical conditions that were during current pregnancy on the low Apgar score at five minutes. Therefore, this study aimed to assess determinants of low fifth minutes AGAR score among newborns delivered at public hospitals of North Shoa zone, central Ethiopia.
Methods & Materials
Stud setting and period
This study was conducted in North Shoa public hospitals, central Ethiopia from March 30 to April 30, 2023. The North Shewa zone is located in the Oromia region, Ethiopia, 112 km northwest of the capital city, Addis Ababa. The zone has a total population of about 1,639,586, of which a majority (89.75%) of the population residing in rural areas. A total of 71 public health institutions serves the population, including 64 health centers, seven hospitals, and 30 private medium clinics. All of these hospitals offer obstetrical services for mothers. The zonal health office's report indicates that overall, 9,364 births were made at the chosen hospital each year. The North Shewa zone's main city Fiche town is home to Salale university comprehensive specialized hospital, which performs about 2,487 births annually. Similarly, Sendafa hospital, M/Turi hospital, G/Meskel hospital, and Chancho hospital oversees around 2004, 1317 and 1645 deliveries annually, 2234 deliveries annually respectively.
Study design
A facility based prospective case-control was conducted.
Population
Source Population
All newborn mothers who gave birth at selected North Shewa Zone public hospitals will be the source population.
Study Population
All selected newborn mothers who gave birth at North Shewa Zone public hospitals during the study period.
Cases: All newborns with a low fifth-minute APGAR score (APGAR less than 7) at the randomly selected hospitals of the North Shewa Zone that fulfilled the inclusion criteria.
Controls: All newborns with a fifth-minute APGAR score (APGAR>=7) at the randomly selected hospitals of North Shewa Zone that fulfilled the inclusion criteria.
Inclusion and Exclusion Criteria
All babies delivered after 28 weeks of gestation & during the study period at North shewa public health facility were included in the study. Charts with incomplete documentation, Newborns referred from other health facilities, Newborns with gross congenital anomalies incompatible with life. Such as anencephaly, severe hydrocephaly, and Gastroschisis, Preterm, Multiple pregnancies except twin pregnancies were excluded from the study
Determination of Sample Size
To determine the required sample size for this study Epi-info version 7.2.2.12 stat calculation software was used for variables that have significant associations with a low fifth-minute APGAR score. Mothers who had a history of khat use, maternal APH in the current pregnancy, Maternal PIH in the current pregnancy, MSAF, and birth injury are considered to calculate the required sample size. From these maternal gravidities is chosen as an independent variable hence it gives us the maximum sample size as compared to other predictor variables.
The sample size was determined using a formula for two population proportions and calculated using Epi-info version 7.2.2.12 stat calculation software by considering that the percent of controls exposed (having Grand multiparity history) were 5.4% whereas 12.09% of cases exposed (main exposure variable) which is estimated from other studies [30], 95% CI, 80% power of the study and control to case ratio of 2:1. Accordingly, after adding 10% for non-response rate 147 cases and 294 controls (a total sample size of 441) are planned to be involved in this study.
Table 1: Sample size calculation for unmatched case-control study by open Epi software
| Factors considered for calculating sample size | Percent of controls exposed (%) | Percent of cases with exposure (%) | No of cases | No of Controls | Ref |
| MSAF | 19.1 | 6.4 | 87 | 174 | (22) |
| Pregnancy induced HTN | 8.3 | 31.2 | 107 | 213 | (20) |
| Birth injury | 22 | 41 | 76 | 151 | (17) |
| Grand multiparity | 5.4 | 12.09 | 221 | 441 | (25) |
| Mothers who had history of khat use | 10.65 | 4.6 | 68 | 135 | (24) |
Sampling Procedure
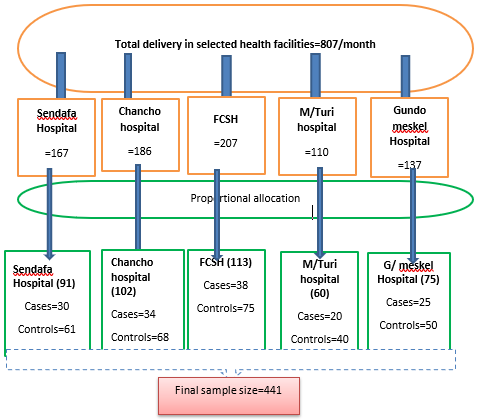
From the 7 functional public hospitals in North Shewa; using the rule of thumb (>=30%) five public hospitals were selected through a simple random sampling technique by lottery method. According to the 2015 E.C semi-annual delivery report of randomly selected health institutions, the lowest monthly proportion of institutional delivery was taken from delivery registration logo book. Accordingly, the sample size was proportionally allocated for hospitals for each hospital by fixing one-month average delivery flow. All cases and subsequent two eligible controls in the study sites were included in the study. A consecutive sampling technique was employed to recruit cases, while a systematic random sampling technique every two intervals was used to select controls. Non-respondents for controls were replaced by the subsequent controls delivered to make the case-to-control ratio even.
 =
= ≈ 2 Where, K= frequency interval
≈ 2 Where, K= frequency interval
N= the total number of the population n = the required number in the sample
Table 2: Show how the sample allocation was calculated for each randomly selected hospitals in North Shoa Zone, Oromia, Ethiopia, 2023
| Institutional name | The average Monthly delivery report | Proportion of neonate delivered | Sample allocated | Number of cases | Number of controls |
| G/meskel Hospital | 137 | 17% | 75 | 25 | 50 |
| Salale university comprehensive specialized Hospital | 207 | 25.7% | 113 | 38 | 75 |
| M/Turi | 110 | 13.6% | 60 | 20 | 40 |
| Chancho Hospital | 186 | 23% | 102 | 34 | 68 |
| Sendafa hospital | 167 | 20.7% | 91 | 30 | 61 |
| Total | 807 | 100% | 441 | 147 | 294 |
Sampling techniques
Figure 1: shows the Schematic presentation of the Sampling technique and procedure for each randomly selected public hospitals in North shewa zone, Oromia, Ethiopia, 2023
Data Collection Procedure & Quality Assurance
A pretest was conducted on 5% of the sample size at Kuyu hospital which is other than the selected hospitals to assess the reliability of data collection instruments. Based on the pretest result, corrective measures were taken on the questionnaire. Before the actual data collection, Training was given to data collectors & supervisors on how to measure the weight of the baby, APGAR score, & on how to take informed consent. The data collectors were clarified the study's intent and receive verbal consent from the respondents. Data was collected by Eight trained Bsc midwives working in delivery wards of each selected public hospital, and two second-degree holding supervisors from the health discipline, respectively. The data was collected through a face-to-face interview using a structured & pretested questionnaire, a mother's medical records review as well as by using an observational checklist. Calibrated Seca scale & observational checklist was used to assess fetal birth weight & APGAR score respectively. Information which could not be obtained by interview, like common medical conditions during current pregnancy, obstetrics factors, intra partum events, and newborn related information, was extracted from maternal records at the postnatal ward. Questionnaire was primarily prepared in the English language and translated into Local language by professional who is familiar on this field and fluent in the two languages and back-translated to English language by another expert, who is not familiar with the original questionnaires in order to guarantee its consistency. To assure the completeness of the questionnaire, the collected data was checked daily during data collection.
Data Processing & Analysis
Firstly, the collected data was cleaned, coded, and checked for missing values & completeness before actual analysis. Then after entered using Epi data version 3.1 and then exported to statistical software and SPSS version 26.0 statistical packages for analysis. To assess the association between predictor variables with the dependent variable, first Binary logistic regression analysis was used. Variables with a significant association at P less than0.25 in the binary analysis were entered into multivariable logistic regression analysis using the stepwise forward variable elimination technique method to determine the determinants of the low fifth-minute APGAR score and those variables with P less than 0.05 were considered to be statistically significant. Multicollinearity was checked by variance inflation factors of less than 10%. Hosmer-Lemeshow tests for goodness of fit was carried out(p=0.472). Finally, the analyzed data was summarized as Frequency, percentage, mean, and standard deviation. Significance was determined using crude and adjusted odds ratios with 95% confidence intervals.
Study Variables
The variables to be included in this questionnaire are both independent and dependent variables for which an association is going to be assessed among cases as well as controls.
Dependent variable
Low fifth-minute APGAR score
Independent variables
Socio-demographic Factors: Age, Sex, Level of education, marital status, residence, Parents in come, Occupation.
Maternal medical/obstetrics factors: mode of delivery, fetal presentation, MSAF, ANC contact, the onset of labor, instrumental delivery, prolonged second stage of labor, DM, Anemia, hyperemesis gravidarum, cardiac disease and PIH.
Neonatal-related factors: sex, birth weight, gestation at birth
Operational Definition
Fetal gestational age: gestational age of the fetus at the time of delivery
High APGAR Score(Controls): A similar group of newborns with APGAR scores of 7 or above at five minute of delivery [25].
Low APGAR score (Cases): Newborns who delivered with APGAR scores below 7 at five minute of delivery [25].
Fifth minute: 5 minutes from the fully delivery of newborn.
Result
Socio-demographic characteristics study participants
A total of 294 controls and 147 cases were involved in the study. All 411 mothers who were asked for an interview was contacted for the research making the response rate 100%. The mothers' ages ranged from 18-43 with mean and standard deviation of (26.8 ± 5.7) respectively. The age group between 20 and 35 years old accounted for around two third of the age distribution of mothers who were cases and controls (62.5%). The independent sample t-test indicates that there is no statistically significant difference in the mean age between the cases and controls (P-value = 0.498). The percentage of housewives among the mothers in the cases was almost similar with the percentage in the controls with the difference is not significant (74.8% vs. 74.4%, p = 0.672). Regarding residence there were a relatively greater percentage of mothers of cases (62.5%) who lived in urban than controls (60.6%). However, the independent sample t-test indicates that there is no statistically significant difference(p=0.075). About 74.8% of the cases and 77.1% of controls were married with no statistically difference between them(p=0.321).
The educational background shows there is slight difference between cases who did not attend formal education (34%) as compared to controls who did not attend formal education (37.4%) but the difference is not statistically significant(p=0.179). There is not a significant difference among or omo ethinic group of cases (74.8%) and controls (78.2%) with p –value= 0.548. About 13.6% of the cases and 13.2% of controls were muslim religious follower with no statistically difference between them(p=0.081). Women khat chewing history among cases (8.2%) and controls (8.1%) were no statistically significant(p=0.057). there is no statistically significant difference among women who had Physical and emotional support during labor and delivery of cases (65.8%) versus controls (68%) at p value=0.086 (Table 3).
Table 3: Socio-demographic characteristics of mothers of cases and controls who gave birth at public hospitals of North Shoa Zone, Oromia, Ethiopia;2023(n=441)
| Questions | Category | Low APGAR score at 5th minutes | Total | P value | |
| Cases | Control | ||||
| Age of the mother? | <20> | 9(6.1) | 20(6.8) | 29(6.5) | 0.498 |
| 20-35 | 92(62.5) | 204(69.3) | 296(67) | ||
| >35 | 36(24.4) | 70(23.8) | 106(24) | ||
| Residence | Urban | 58(39.4) | 110(37.4) | 168(38) | 0.075 |
| Rural | 89(60.6) | 184(62.5) | 273(62) | ||
| Marital status | single | 6(4) | 4(1.3) | 10(2.2) | 0.321 |
| married | 110(74.8) | 230(78.2) | 340(77.1) | ||
| divorced | 11(7.4) | 24(8.1) | 35(8) | ||
| Widowed | 20(13.6) | 36(12.2) | 56(12.7) | ||
| Ethnicity | Oromo | 85(57.8) | 171(58.1) | 256(58) | 0.548 |
| Amhara | 30()20.4 | 60(20.4) | 90(20.4) | ||
| Tigre | 14(9.5) | 28(9.5) | 42(9.5) | ||
| Guraghe | 18(12.2) | 35(11.9) | 53(12) | ||
| Religion | Orthodox | 70(47.6) | 140(47.6) | 210(47.6) | 0.081 |
| Protestant | 54(36.7) | 108(36.7) | 162(36.7) | ||
| Muslim | 20(13.6) | 39(13.2) | 59(13.3) | ||
| Catholic | 3(2) | 7(2.3) | 10(2.2) | ||
| Educational status? | No formal education | 50(34) | 110(37.4) | 160()36 | 0.179 |
| Primary education | 50(34) | 90(30.6) | 140(32) | ||
| Secondary education (9-12) | 25(17) | 50(17) | 75(17) | ||
| College and above | 22()14.9 | 44(14.9) | 66(15) | ||
| Occupation? | House wife | 110(74.8) | 220(74.8) | 330(74.8) | 0.672 |
| Government employee | 7(4.7) | 20(6.8) | 27()6.1 | ||
| Private employee | 2(1.3) | 14(4.7) | 16(3.6) | ||
| Merchant | 28(19) | 40(13.6) | 68(15.4) | ||
| Khat chewing history? | Yes | 12(8.2) | 24(8.1) | 36(8.2) | 0.057 |
| No | 135(91.8) | 270(91.8) | 405(91.8) | ||
| Physical and emotional support during labor and delivery | Yes | 97(65.9) | 200(68) | 297(67.4) | 0.086 |
| No | 50(34.1) | 94(32) | 144(32.6) | ||
Obstetrics characteristics of mothers
There was a significant difference (p = 0.093) between the proportion of mothers of cases who had no ANC contact and that of controls (65.9% vs. 68%). There was no significant difference (0.342) between the control and case groups in terms of the percentage of women who were Primigravida 10.2% vs 10.2%, Multigravida 57.8% vs 61.2%, and Grand multigravida 32% vs 28.5% respectively. In comparison to controls, cases were more likely to experience antepartum hemorrhage, and delivered from twin pregnancy and premature membrane rupture Type of the Pregnancy (7.4% versus 7.5%; P= 0.023), and (13.6% versus 11.9%; p=0.002) respectively. The percentage of women who had PIH in the current pregnancy did not change significantly between the case and control groups (14.3% versus 11.9% = 0.074).
Among controls compared to cases, the proportion of women who had Duration of PROM less than 12 hours, and cord prolapse was not significantly greater (19.1% versus 11.6%; P=0.084), and (11.5% versus 2.3%; P=0.071) respectively. The percentage of women who had PROM in the current pregnancy did not change significantly between the case and control groups (38.7% versus 32%; P= 0.192). Nevertheless, the chi-square test p-value of 0.093 indicates that there is no statistically significant difference in presence of chorioamnionitis between cases and controls (25% versus 15%). Among controls compared to cases, the proportion of women who undergone Induced onset of labor, and augmented with oxytocin was not significantly greater (19.8% versus 13%; P= 0.079), and (24% versus 15%; P=0.142) respectively.
Only 18.3%of mothers of controls and 15%of mothers of cases had Prolonged second stage of labor, yet there is no statistically significant difference between the two groups (chi-square test-p-value = 0.065). Meconium-stained liquor, Caesarean section mode of delivery, Anemia were varied between controls and cases in a statistically significant way (20.4%, versus 13%; P=0.004), (19.8% versus 19.8%; P=0.036), and (14.2%versus 10.2%; P=0.024) for the Chi-square test, respectively (Table 4).
Table 4: Obstetric characteristics of mothers of cases and controls who gave birth public hospitals of North Shoa Zone, Oromia, Ethiopia;2023(n=441)
| Variables | Category | Low 5th minute APGAR score | Total | P value | |
| Cases | Controls | ||||
| Gravidity of the mother? | Primigravida | 15(10.2) | 30(10.2) | 45(10.2) | 0.342 |
| Multigravida | 85(57.8) | 180(61.2) | 265(60) | ||
| Grand multigravida | 47(32) | 84(28.5) | 131(29.8) | ||
| Parity of the mother? | Primiparous | 11(7.4) | 30(10.2) | 41(9.3) | 0.765 |
| Multiparous | 89(60.5) | 190(64.6) | 279(63.2) | ||
| Grand multiparous | 47(32) | 74(25.2) | 121(27.4) | ||
| ANC visit | Yes | 97(65.9) | 200(68) | 297(67.3) | 0.001 |
| No | 50()34.1 | 96(32) | 146(32.7) | ||
| Number of ANC visit? | 1 time | 25(17) | 55(18.7) | 80(18.1) | 0.067 |
| 2-3 times | 22(14.9) | 80(27.3) | 102(23) | ||
| >=4 times | 40(27.2) | 65(22) | 105(23.8) | ||
| Type of the Pregnancy | Singleton | 127(86.4) | 259(88) | 386(81.5) | 0.002 |
| Twins | 20(13.6) | 35(11.9) | 55(12.5) | ||
| APH | Yes | 11(7.4) | 22(7.5) | 33(7.5) | 0.023 |
| No | 136(92.5) | 272(92.5) | 408(92.5) | ||
| PIH in the current pregnancy | Yes | 21(14.3) | 35(11.9) | 56(12.7) | 0.074 |
| No | 126(85.7) | 259(88) | 385(87.3) | ||
| PROM | Yes | 57(38.7) | 94(32) | 151(34.2) | 0.192 |
| No | 90(61.2) | 200(68) | 290(65.8) | ||
| Duration of PROM | <12> | 119(80.9) | 260(88.4) | 379(86) | 0.084 |
| >12 hours | 28(19.1) | 34(11.6) | 62(14) | ||
| Is there chorioamniotis | Yes | 37(25) | 44(15) | 81(18.7) | 0.093 |
| No | 110(75) | 250(75) | 360(81.6) | ||
| The onset of labor | Spontaneous | 118(80.2) | 256(87) | 374(84.8) | 0.079 |
| Induced | 29(19.8) | 38(13) | 67(15.2) | ||
| labor Augmented | Yes | 35(24) | 44(15) | 79(18) | 0.142 |
| No | 112(76) | 250(75) | 362(82) | ||
| Prolonged second stage of labor | Yes | 27(18.3) | 44(15) | 71(16) | 0.065 |
| No | 120(81.7) | 250(75) | 370(84) | ||
| Meconium-stained liquor | Yes | 30(20.4) | 38(13) | 68(15.4) | 0.004 |
| No | 117(79.6) | 256(87) | 373(84.6) | ||
| Mode of delivery | SVD | 98(66.6) | 200(68) | 298(67.4) | 0.036 |
| Operative vaginal Delivery | 20(13.6) | 36(12.2) | 56(12.6) | ||
| Caesarean section | 29(19.8) | 58(19.8) | 87(19.7) | ||
| Anemia | Yes | 21(14.2) | 30(10.2) | 51(11.6) | 0.024 |
| No | 126(85.8) | 264(89.8) | 390(88.4) | ||
| Cord prolapses | Yes | 17(11.5) | 7(2.3) | 24(5.5) | 0.071 |
| No | 130(88.5) | 287(98.7) | 417(94.5) | ||
Common medical illness related factors
The percentage of women who had diabetes mellitus did not change significantly between the case and control groups (85.7% vs. 88%, p = 0.057). The percentage of women who had 11.5 versus 2.3 % but the difference was not statistically significantly between the case and control groups (p = 0.749). About (38.7%) of cases and (32%) controls had history of hyperemesis gravidarum but the difference was not statistically significant(p=0.076). The percentage of women who had HIV/AIDS did not change significantly between the case and control groups (32% vs. 30.6%, p = 0.241). The percentage of women who had 11.5 versus 2.3 % but the difference was not statistically significantly between the case and control groups (p = 0.749). About (18.3%) of cases and (15%) controls had history of hepatitis B virus but the difference was not statistically significant (p= 0.083) (Table 5).
Table 5: Common medical illiness related factors of cases and controls who gave birth public hospitals of North Shoa Zone, Oromia, Ethiopia;2023(n=441)
| Variables | Response | 5th minute APGAR score | Total | p-value | |
| Cases | Controls | ||||
| Diabetes mellitus | Yes | 126(85.7) | 259(88) | 385(87.3) | 0.057 |
| No | 21(14.3) | 35(11.9) | 56(12.7) | ||
| Cardiac disease | Yes | 17(11.5) | 7(2.3) | 24(5.5) | 0.749 |
| No | 130(88.5) | 287(98.) | 417(94.5) | ||
| Hyperemesis gravidarum | Yes | 57(38.7) | 94(32) | 151(34.2) | 0.076 |
| No | 90(61.2) | 200(68) | 290(65.8) | ||
| HIV status | Reactive | 47(32) | 90(30.6) | 137(31) | 0.241 |
| Non-reactive | 100(68) | 204(69.4) | 304(69) | ||
| Hepatatis B virus status | Reactive | 27(18.3) | 44(15) | 71(16) | 0.083 |
| Non-reactive | 120(81.7) | 250(75) | 370(84) | ||
Fetal/neonatal characteristics
When it came to newborn sex, the percentage of female was 58.5% among cases and 54.4% among controls, respectively. This difference between cases and controls is not statistically significant (p-value = 0.547). Sixty seven percent of the cases were term, as compared to eighty-one percent of the controls (p = 0.071). Although the difference was not statistically significant(p=0.176), About 68% of cases among infants had a vertex presentation, compared to 69.4% of controls. Compared to controls, cases had greater proportions of low birth weight (16.3% vs. 16.4%, p = 0.019). The observed birth weight difference between cases and controls is statistically significant (Table 6).
Table 6: Characteristics of newborns who delivered at public hospitals of North Shoa Zone, Oromia, Ethiopia; 2023 (n=441)
| Questions | Category | Low 5th minute APGAR score | Total | P value | |
| Cases | Controls | ||||
| Fetal Sex | Female | 86(58.5) | 160(54.4) | 246(55.7) | 0.547 |
| Male | 61(41.4) | 134(45.6) | 195(44.3) | ||
| Gestational age at birth? | Term | 99(67.4) | 240(81.6) | 339(76.8) | 0.071 |
| Post-term | 48(32.6) | 54(18.3) | 102(24.2) | ||
| Fetal presentation at birth? | Breech | 47(32) | 90(30.6) | 137(31) | 0.176 |
| Cephalic | 100(68) | 204(69.4) | 304(69) | ||
| Fetal weight at birth? | Low birth weight | 24(16.3) | 48(16.4) | 72(16.4) | 0.019 |
| Macrocosmic | 23(15.6) | 26(8.8) | 49(11.1) | ||
| Normal | 90(61.2) | 220(74.8) | 310(70.5) | ||
Determinant factors of 5th minute low Apgar score
The findings of the binary logistic regression analysis showed that the low Apgar score was significantly correlated with the following factors: antepartum hemorrhage (APH), meconium-stained amniotic fluid (MSAF), mode of delivery, anemia, fetal sex, gestational age at birth, Pregnancy type, and fetal weight at birth. All significant variables from binary logistic regression were accounted for in multivariable logistic regression. The findings indicated that women delivered from twin pregnancy had about 1.7 times the odds of having a poor five-minute Apgar score as compared to newborns delivered from single pregnancy [AOR = 1.7, 95% CI: 1.23–2.17]. Compared to a normal 5th minute Apgar score, women who had no prenatal care contact were 1.6 times more likely to have a fifth minute low Apgar score [AOR = 1.6, 95% CI: 1.02–2.18]. Furthermore, compared to normal 5th minute Apgar, there was a 2.4fold increase in the likelihood of a poor Apgar score for babies born to anemic women [AOR = 2.4, 95% CI: 1.76–3.04]. Compared to their peers, neonates who delivered with a low Apgar score in the fifth minute had a 2.4 times higher risk of having low birth weight [AOR = 2.4, 95% CI: 1.54 3.08] (Table 7).
Table 7: Binary and multivariable logistic regression analysis on determinant factors of low Apgar score among newborns who delivered at public hospitals of North Shoa Zone, Oromia, Ethiopia;2023 (n=441)
| Variables | Category | 5th minute low Apgar score | Odds Ratio | ||
| Cases | Controls | COR | AOR | ||
| Gestational age at birth | Term | 99(67.4) | 240(81.6) | 1 | 1 |
| Post-term | 48(32.6) | 54(18.3) | 2.1(1.10–3.1) | 1.8(0.87-1.39) | |
| Fetal birth weight | Low birth weight | 24(16.3) | 48(16.4) | 1.2(1.04-2.43) | 2.4(1.54-3.08) * |
| Macrosomic | 23(15.6) | 26(8.8) | 2.1(0.97-3.23) | 1.9(0.67-3.13) | |
| Normal | 90(61.2) | 220(74.8) | 1 | 1 | |
| ANC Visit | Yes | 97(65.9) | 200(68) | 0.93(0.27-1.94) | 1.6(1.02-2.18) * |
| No | 50()34.1 | 96(32) | 1 | 1 | |
| APH | Yes | 11(7.4) | 22(7.5) | 1.0(0.74-1.48) | 1.2(0.63-1.77) |
| No | 136(92.5) | 272(92.5) | 1 | 1 | |
| Pregnancy type | Single | 127(86.4) | 259(88) | 1 | 1 |
| Twin | 20(13.6) | 35(11.9) | 1.1(1.07-2.14) | 1.7(1.23-2.17) * | |
| MSAF | Yes | 30(20.4) | 38(13) | 1.7(0.17-3.23) | 0.9(0.64-1.16) |
| No | 117(79.6) | 256(87) | 1 | 1 | |
| Mode of delivery | SVD | 98(66.6) | 200(68) | 1 | 1 |
| Operative vaginal Delivery | 20(13.6) | 36(12.2) | 1.2(0.58-1.96) | 1.1(0.83-1.37) | |
| Caesarean section | 29(19.8) | 58(19.8) | 1.02(0.64-1.28) | 1.3(0.78-1.82) | |
| Anemia | Yes | 21(14.2) | 30(10.2) | 1.4(1.14-2.29) | 2.4(1.76-3.04) * |
| No | 126(85.8) | 264(89.8) | 1 | 1 | |
Discussion
Apgar score can be influenced by various factors that occur before and during pregnancy including the physical and emotional support during labor and delivery. Therefore, this study identified the determinant factors for a low Apgar score which is important for proper, immediate, and sustainable intervention to improve maternal for better pregnancy outcomes. The determinants that were independently associated with the low APGAR at five minutes were no ANC follow up, anemia, and birth weight. Fifth minute low Apgar score was more likely on newborns who delivered from anemic mothers compared to normal 5th minute Apgar score. This study is consistent with studies done in Sweden, Brazil, the USA, and Gondar [13,21,26]. This similarity is due to the fact that, anemia during pregnancy puts infants at increased risk of immediate birth asphyxia and long-term permanent cognitive damage and mortality [27]. Anemia in pregnancy is more prevalent in the developing world, where under nutrition and infections are more frequent which complicates pregnancy outcome. However, a study done in Amhara region Ethiopia and Japan indicated that anemia during pregnancy is not a determinant factor for birth asphyxia/low Apgar score [13,21,28]. This difference could be due to high prevalence of a history of antepartum hemorrhage in this study and difference in study setting. This finding suggests that health care providers should take into account the potential risk of anemia during pregnancy while assessing clinical condition of the mother.
The risk of the low Apgar score was higher in newborns whose mothers had no antenatal care contact compared to normal 5th minute Apgar. This finding is similar to studies done in Sweden [14,21]. This could be the fact that supplementation, treatments, birth preparedness and readiness and counseling for a danger sign of pregnancy is given during antenatal care follow up. Medical care for women with obstetric complications begins with the recognition of danger signs. Delays in recognizing danger signs, in seeking, reaching, and obtaining appropriate maternity care are key elements in maternal and perinatal health. The other possibility could be because mothers who had no ANC visits will not gain a screening opportunity for certain risk factors like, anemia during pregnancy and low birth weight which were the risk factors for the low Apgar score in this study. Low at Apgar Fifth minute score was more likely on newborns delivered from twin pregnancy when compared to newborns delivered from single pregnancy [14]. This could be related to being delivered from twin pregnancy prone the neonates to the risk of low birth weight, preterm delivery, exposed to anesthesia if the delivery is undergone by cesarean section. Besides women with twin pregnancy is at the risk of Anemia during pregnancy as increased iron demand.
This finding also indicates that the antenatal care follow up efficiently will help to mitigate the problem of low Apgar score Low birth weight was a major determinant factor that was significantly associated with a low Apgar score in the present study. Those newborns who delivered with a 5th minute low Apgar score were higher odds of having low birth weight compared to their counterparts. This finding is also consistent with the studies conducted in Ethiopia, Iran, and Ghana [21,29,30]. This could be explained by the fact that small babies might suffer from difficult birthing, impaired thermoregulation, hypoglycemia, polycythemia and might develop difficulty in cardiopulmonary transition and perinatal asphyxia, which could further affect Apgar score.
Conclusion
A low Apgar score was shown to be associated with a number of characteristics, including not receiving ANC follow up, having anemia during pregnancy, having low birth weight, and twin pregnancy. Therefore, it is recommended that obstetric care providers firmly adhere to advise and counseling on the importance of ANC follow up. In addition, they should provide widespread health education on factors such as low birth weight, and twin pregnancy as they increase the likelihood of low fifth minute Apgar score. Effective health education during pre-pregnancy about anemia during pregnancy and Antepartuem period will aid in identifying high-risk pregnancies that could causes low fifth minutes Apgar score.
Recommendation
During labor and delivery, it was advised to increase access to compassion ship in addition to the normal treatment of employing electronic fetal monitoring. Effective health education, particularly that which promotes a healthy lifestyle before to conception and antenatal care, will aid in the identification of high-risk pregnancy that results in a low fifth minutes APGAR score. Pregnant mothers who run the risk of giving birth to children with low Apgar scores should be screened, counseled, and given access to vital health information on the factors that contribute to low Apgar scores. Create Public awareness and provide health education for women come to health facility.
Limitation of study
The study lacked access to data on a number of previously documented determinant factors of low Apgar score, including analgesia during labor and delivery, uterine rupture, abnormal heart rate in fetal tissue, diabetes mellitus, antipsychotic medication, thrombocytopenia, and thyroid disorders. The results may not apply to preterm, severe congenital malformations, or numerous pregnancies because the study was limited to term and post-term pregnancies. There might be intra-observer variability as a result of the research design.
Abbreviations & Acronyms
| ANC | Antenatal Care |
| APGAR | American pediatrics growth assessment record |
| APH | Antepartum hemorrhage |
| AOR | Adjusted odd ratio |
| ARR | Adjusted relative risk |
| ASD | Atrial septal defect |
| BMI | Body mass index |
| BSc | Bachelor of science |
| CI | Confidence interval |
| C/S | Caesarian Section |
| DM | Diabetes mellitus |
| EDHS | Ethiopian demographic health survey |
| ETB | Ethiopian Birr |
| HEG | Hyperemesis gravidarum |
| HIE | Hypoxic ischemic necrosis |
| HIV | Human immune virus |
| LBW | Low birth weight |
| NMR | Neonatal mortality rate |
| MD | Medical doctor |
| MSAF | Meconium-stained amniotic fluid |
| MSc | Masters of Science |
| PIH | Pregnancy induced hypertension |
| PROM | Premature rupture of membrane |
| SDG | Sustainable development goal |
| SPSS | Statistical package for social science |
| U5MR | Under five mortality rates |
| US | United states |
| WHO | World health organization |
Declarations
Acknowledgements
The authors are grateful to the Salale University, College of Health Science for the approval of the ethical clearance. They are also thankful to the North Shoa Zonal Health Office and the public hospitals in North Shoa Zone for their agreement to do this study in the hospitals. Finally, we would like to thank the study participants and data collectors for their cooperation throughout the study period.
Authors Contributions
The description provided outlines the specific contributions of each author in a research study. Here's a summary of their roles:TKS Conceived the study, participated in its design and coordination, initiated the research, carried out the statistical analysis, interpreted the results, wrote the final manuscript, and critically reviewed it. TKS also bears primary responsibility for the final content, acts as a guarantor to access the data, and makes the final decision to publish.
BA and YJ: Participated in the study’s design, guided the statistical analysis, and critically reviewed the manuscript. TKS, BA and YJ: Were involved in principal supervision, participated in the study’s design and coordination, edited the manuscript, and critically reviewed the manuscript. All authors have read and approved the final manuscript.
Funding
The authors did not receive a specific grant for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests
None declared.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
Prior to the data collection period, ethical clearance and approval were obtained from the Salale University ethical board, with reference number IRB/902/14. A letter of support was provided to the administrative office of each selected hospital, and permission was granted to conduct the study. Written informed consent was obtained from each study participant after explaining the study's purpose, procedures, benefits, duration, and any potential risks in the local language. Participants were assured of their right to withdraw from the study at any time. This study was conducted in accordance with the principles of the Declaration of Helsinki. All information collected from participants was treated confidentially, with identifiers removed to protect their privacy. Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data are available upon reasonable request. The datasets used and/or analyzed during the current study can be obtained from the corresponding author upon reasonable request.
References
- FMOH. (2021). Neonatal Intensive Care Unit (NICU) Training Participants’ Manual. Fmoh, 194.
Publisher | Google Scholor - Hodgins C. Apgar score. (1997). J Obstet Gynecol Neonatal Nurs, 26(1):15-16.
Publisher | Google Scholor - Leuthner SR, Das UG. (2004). Low Apgar scores and the definition of birth asphyxia. Pediatr Clin North Am, 51(3):737-745.
Publisher | Google Scholor - World Health Organization. (2017). Recommendations on newborn health: approved by the WHO Guidelines Review Committee, 1-28.
Publisher | Google Scholor - world health organization. (2018). Who Country Cooperation Strategic Agenda (2016-2020): Ethiopia, 1-2.
Publisher | Google Scholor - Rosa-Mangeret F, Benski AC, Golaz A, Zala PZ, Kyokan M, Wagner N, et al. (2022). 2.5 million Annual Deaths—Are Neonates in Low-and Middle-Income Countries Too Small to Be Seen? A Bottom-Up Overview on Neonatal Morbi-Mortality. Trop Med Infect Dis, 7(5):1-21.
Publisher | Google Scholor - Sharrow D, Hug L, You D, Alkema L, Black R, Cousens S, et al. (2022). Global, regional, and national trends in under-5 mortality between 1990 and 2019 with scenario-based projections until 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet Glob Heal, 10(2): e195-206.
Publisher | Google Scholor - Ethiopian Public Health Institute (EPHI), ICF. (2021). Ethiopia Mini Demographic and Health Survey 2019: Final Report, 1-207p.
Publisher | Google Scholor - Ethiopian Public Health Institute Addis Ababa. (2019). Ethiopia Mini Demographic and Health Survey. Federal Democratic Republic of Ethiopia Ethiopia.
Publisher | Google Scholor - Lawn JE, Lee ACC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. (2009). Two million intrapartum-related stillbirths and neonatal deaths: Where, why, and what can be done? Int J Gynecol Obstet, 107:5-19.
Publisher | Google Scholor - Gillette E, Boardman JP, Calvert C, John J, Stock SJ. (2022). Associations between low Apgar scores and mortality by race in the United States: A cohort study of 6,809,653 infants. PLoS Med, 19(7):1-15.
Publisher | Google Scholor - Modabbernia A, Sandin S, Gross R, Leonard H, Gissler M, Parner ET, et al. (2019). Apgar score and risk of autism. Eur J Epidemiol, 34(2):105-114.
Publisher | Google Scholor - Gudayu TW. (2017). Proportion and factors associated with low fifth minute Apgar score among singleton newborn babies in Gondar University referral hospital; North West Ethiopia. Afr Health Sci, 17(1):1-6.
Publisher | Google Scholor - Odd DE, Rasmussen F, Gunnell D, Lewis G, Whitelaw A. (2008). A cohort study of low Apgar scores and cognitive outcomes. Arch Dis Child Fetal Neonatal Ed, 93(2):115-120.
Publisher | Google Scholor - Li F, Wu T, Lei X, Zhang H, Mao M, Zhang J. (2013). The Apgar Score and Infant Mortality. PLoS One, 8(7):1-8.
Publisher | Google Scholor - Ensing S, Schaaf JM, Abu-Hanna A, Mol BWJ, Ravelli ACJ. (2014). Recurrence risk of low Apgar score among term singletons: A population-based cohort study. Acta Obstet Gynecol Scand, 93(9):897-904.
Publisher | Google Scholor - Tavares VB, Souza J De, Vinicius M, Affonso DG, Souza E, Rocha D, et al. (2022). Factors associated with 5 ‑ min APGAR score, death and survival in neonatal intensive care: a case ‑ control study. BMC Pediatr, 1-11.
Publisher | Google Scholor - Province S. (2021). Journal of Pregnancy and Traditional beliefs and Practices in Newborn Care among Mothers in, 4(1):1-6.
Publisher | Google Scholor - Haddad B, Mercer BM, Livingston JC, Talati A, Sibai BM. (2000). Outcome after successful resuscitation of babies born with Apgar scores of 0 at both 1 and 5 minutes. Am J Obstet Gynecol, 182(5):1210-1214.
Publisher | Google Scholor - Gebremedhin MM. (2018). Determinants of low APGAR score in newborns delivered at Lemlem Karl general hospital, Northern Ethiopia, 2018: a case control study, 2:1-17.
Publisher | Google Scholor - Yeshaneh A, Kassa A, Kassa ZY, Adane D, Fikadu Y, Wassie ST, et al. (2021). The determinants of 5th minute low Apgar score among newborns who delivered at public hospitals in Hawassa City, South Ethiopia. BMC Pediatr, 21(1):1-10.
Publisher | Google Scholor - Ajibo BD, Wolka E, Aseffa A, Nugusu MA, Adem AO, Mamo M, et al. (2022). Determinants of low fifth minute Apgar score among newborns delivered by cesarean section at Wolaita Sodo University Comprehensive Specialized Hospital, Southern Ethiopia: an unmatched case control study. BMC Pregnancy Childbirth, 22(1):1-14.
Publisher | Google Scholor - Mgaya AH, Massawe SN, Kidanto HL, Mgaya HN. (2013). Grand multiparity: Is it still a risk in pregnancy? BMC Pregnancy Childbirth, 13.
Publisher | Google Scholor - Getachew B, Etefa T, Asefa A, Terefe B, Dereje D. (2020). Determinants of Low Fifth Minute Apgar Score among Newborn Delivered in Jimma University Medical Center, Southwest Ethiopia. Int J Pediatr, 2020.
Publisher | Google Scholor - Obsa MS, Shanka GM, Menchamo MW, Fite RO, Awol MA. (2020). Factors Associated with Apgar Score among Newborns Delivered by Cesarean Sections at Gandhi Memorial Hospital, Addis Ababa. J Pregnancy, 2020.
Publisher | Google Scholor - Cnattingius S, Johansson S, Razaz N. (2020). Apgar Score and Risk of Neonatal Death among Preterm Infants. N Engl J Med, 383(1):49-57.
Publisher | Google Scholor - Desalew A, Sintayehu Y, Teferi N, Amare F, Geda B, Worku T, et al. (2020). Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: A facility-based prospective follow-up study. BMC Pediatr, 20(1):1-11.
Publisher | Google Scholor - Murata T, Yasuda S, Imaizumi K, Isogami H, Fukuda T, Kyozuka H, et al. (2022). Association of labour duration in spontaneous deliveries with low neonatal Apgar scores and foetal acidosis: the Japan Environment and Children’ s Study, 1-9.
Publisher | Google Scholor - Kiyani AN, Khushdil A, Ehsan A. (2014). Perinatal factors leading to birth asphyxia among term newborns in a tertiary care hospital. Iran J Pediatr, 24(5):637-642.
Publisher | Google Scholor - E.T. D, A.T. O, B.K. O. (2014). Stillbirths and very low Apgar scores among vaginal births in a tertiary hospital in Ghana: A retrospective cross-sectional analysis. BMC Pregnancy Childbirth, 14(1):1-8.
Publisher | Google Scholor