Research Article
Comprehensive Nursing's Effects on Diabetic Children's Quality of Life, Nod-Like Receptor Protein 3 levels, and Inflammatory Cytokines
- Muhammad Waqar Mazhar *
Department of Bioinformatics and Biotechnology, Government College University,38000, Faisalabad, Pakistan.
*Corresponding Author: Muhammad Waqar Mazhar, Department of Bioinformatics and Biotechnology, Government College University,38000, Faisalabad, Pakistan.
Citation: Mazhar. M.W. (2025). Comprehensive nursing's effects on diabetic children's quality of life, Nod-Like Receptor Protein 3 levels, and inflammatory cytokines. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 7(2):1-8. DOI: 10.59657/2837-4681.brs.25.133
Copyright: © 2025 Muhammad Waqar Mazhar, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 21, 2025 | Accepted: February 06, 2025 | Published: February 13, 2025
Abstract
Our goal was to find out how comprehensive nursing care affected the children with diabetes's quality of life and inflammatory cytokine levels. Fifty-eight children with diabetes who were hospitalized to our hospital participated in a control study. The patients were randomly divided into two groups, one to serve as an observation group and the other as a control group. Each group had 29 cases. The control group consisted of children who were given the standard nursing care. The children in the controlgroup received psychosocial, medical, nutritional, physicalactivity, disease-specific, daily living, and humanistic nursing care. Following nursing care, there was a significant difference (P < 0.05) in the blood glucose indicators, self-rating anxiety and depression scale scores, and drug-administration compliance, quality of life, and nursing satisfaction scores between the observation group and the control group. Furthermore, we noticed that following nursing, the observation group's levels of interleukin-8 (IL-8) and nod-like receptor protein 3 (NLRP3) were significantly lower (P < 0.05). It is advisable to prescribe and implement comprehensive nursing care for children with diabetes, as it can successfully increase blood glucose levels, alleviate negative psychological effects, and enhance nursing satisfaction.
Keywords: inflammatory cytokines; comprehensive nursing; pediatric diabetes; quality of life
Introduction
One of the most prevalent clinical metabolic disorders, diabetes mellitus has a high incidence and is more prevalent in middle-aged and older adults [1]. Nonetheless, research indicates that diabetes is more common in younger people and that the number of pediatric cases of the disease is rising annually [2, 3]. According to reports, the annual incidence of diabetes in children is rising by 3% and the growth rate of the disease is estimated to be 200 cases/d in China [4, 5]. Children with diabetes who experience prolonged hyperglycemia may have a reduction in their body's resistance, which could have an impact on their physical and mental development [6]. If pediatric diabetes is not treated in a timely manner, it may worsen the child's condition over time, result in acidosis, dehydration, and other issues, and perhaps endanger the child's life [7]. Drug control is still utilized in clinical treatment for these diseases [8]. Insulin and hypoglycemia medications must be used rationally during the course of treatment [9]. But because diabetes is a chronic condition, nursing advice and explanation are required during the nursing time when the kid is receiving medication therapy. This will help to increase the child's compliance with treatment and guarantee the child's treatment plan develops smoothly [10]. The traditional nursing model can no longer suit the needs of clinical nursing because of its singular content. The nursing model must be continuously improved in order to guarantee the demands of the nursing staff [11]. Comprehensive nursing is a holistic approach to nursing care, offering focused and all-encompassing nursing services to children with illnesses from a variety of perspectives, such as psychology, health education, sickness, nutrition and exercise, day-to-day living, and humanistic care [12]. One of the primary causes of diabetes is low-level chronic inflammation [13, 14]. Evidence from several research in both humans and animals suggest that inflammatory cytokines such TNF-α, IL-8, and IL-6 are more prevalent in diabetes patients. [15]. As a result, there is a strong correlation between inflammation and the onset of diabetes and insulin resistance. The inflammasome that has been studied the most to date is Nod-like receptor protein 3 (NLRP3) [16]. The purpose of this study was to look into how comprehensive nursing care affected the quality of life, NLRP3 and inflammatory cytokine levels, in children with diabetes.
Materials and methods
General data
For the purpose of this randomized controlled trial, we recruited 58 pediatric patients with diabetes who were hospitalized to our hospital from 2018 to 2021. Using a random number system, two groups of patients were formed: one to act as a control and another to watch. The control group included 16 males and 13 females, with an average age of 14.56 ± 1.57 kg/m² and a variety of diabetes durations (varying from 1-4 years, with an average of 2.32 ± 0.23 years). Individuals taking part in the study were between the ages of three and twelve. Fifteen men and fourteen women made up the thirty-person observation group. Diabetes duration varied from one to four years, with an average of 2.26 ± 0.21 years, and the average age was 14.62 ± 1.68 kg/m². Children as young as three years old and as elderly as twelve years old took part. Using similar general statistics, we found no significant difference between the two groups (P > 0.05). In order to be included in the study, all of the following were needed: full and accurate clinical data, informed consent from sick children's families, approval from the ethics committee at Children Hospital Multan, and a diagnosis of diabetes, absence of mental illness, and positive results for both glucose and ketones in the urine. Participant had any of the following conditions, they were not included in the study other severe organ diseases, mental illness, a history of related diseases, cognitive and communication impairments of varying degrees, illiterate parents with impairments in cognition, communication, awareness, and mobility, blood and immune system disorders, long-term drug users, incomplete clinical data, or were dropped from the study.
Methods
General data
For the purpose of this randomized controlled trial, we recruited 58 pediatric patients with diabetes who were hospitalized to our hospital from 2018 to 2021. Using a random number system, two groups of patients were formed: one to act as a control and another to watch. The control group included 16 males and 13 females, with an average age of 14.56 ± 1.57 kg/m² and a variety of diabetes durations (varying from 1-4 years, with an average of 2.32 ± 0.23 years). Individuals taking part in the study were between the ages of three and twelve. Fifteen men and fourteen women made up the thirty-person observation group. Diabetes duration varied from one to four years, with an average of 2.26 ± 0.21 years, and the average age was 14.62 ± 1.68 kg/m². Children as young as three years old and as elderly as twelve years old took part. Using similar general statistics, we found no significant difference between the two groups (P > 0.05). In order to be included in the study, all of the following were needed: full and accurate clinical data, informed consent from sick children's families, approval from the ethics committee at Children Hospital Multan, and a diagnosis of diabetes, absence of mental illness, and positive results for both glucose and ketones in the urine. Participant had any of the following conditions, they were not included in the study other severe organ diseases, mental illness, a history of related diseases, cognitive and communication impairments of varying degrees, illiterate parents with impairments in cognition, communication, awareness, and mobility, blood and immune system disorders, long-term drug users, incomplete clinical data, or were dropped from the study.
Results
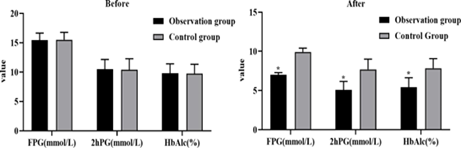
Comparison of blood glucose indicators between the two groups
The two groups exhibited no significant differences in blood glucose indicators (FPG, 2hPG, and HbA1c) prior to nursing (P > 0.05). Post-nursing, a statistically significant difference was seen (P less than 0.05, Figure 1), with the observation group exhibiting lower levels of the specified markers in comparison to the control group. The technique implemented by the observation group has proven beneficial in managing diabetes in youngsters.
Figure 1: Both groups' pre- and post-nursing blood glucose indicators Note: *P less than 0.05, compared with the control group.
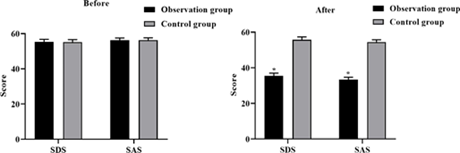
Comparison of the psychological state between the two groups
Before nursing intervention, there was no notable change in psychological state between the two groups as assessed by SDS and SAS scores (P > 0.05). Post-nursing, a statistically significant difference was seen between the observation group and the control group, with the observation group exhibiting lower SAS and SDS scores (P less than 0.05, Figure 2). The observation group's technique appears to enhance the well-being of diabetic kids.
Figure 2: Mental health statuses of the two groups before and during nursing care Note: *P less than 0.05, compared with the control group.
Comparison of nursing satisfaction of family members between the two groups. When comparing the two groups, the observation group reported far higher levels of nursing satisfaction.t (P less than 0.01, Table 1).
Table 1: Nurses' ability to make their loved ones happy in the two categories
| Groups | Service attitude | Operational l skills | Communicate on skills | Blood glucose control |
| Observation group(n = 29) | 84.88 ± 8.07 | 89.85 ± 5.86 | 86.56 ± 7.07 | 94.81 ± 5.36 |
| Control group(n = 29) | 79.62 ± 8.14 | 84.33 ±6.17 | 81.88 ± 7.12 | 88.14 ± 5.54 |
| X2 | 4.762 | |||
| P | < 0.01 | |||
Comparison of medication compliance between the two groups
There was a not able disparity in medication compliance between the control group(75.66%) and the observation group (96.55%) (P less than 0.01, Table 2).
Table 2: Adherence to drug regimens between the two sets
| Groups N | Complete compliance | Partial compliance | Non-compliance | Compliance rate (%) |
| Observation group(n=29) | 22 | 6 | 1 | 28 (96.55) |
| Control group (n =29) | 14 | 8 | 7 | 22 (75.86) |
| X2 | 4.762 | |||
| P | < 0.01 | |||
Comparison of quality-of-life scores between the two groups
Comparison of nursing satisfaction of family members between the two groups. When comparing the two groups, the observation group reported far higher levels of nursing satisfaction.t (P less than 0.01, Table 1).
Figure 3: Life satisfaction ratings for the two categories Note: *P less than 0.05, compared with the control group.
Comparison of IL-8 and NLRP3 levels between the two groups
Figure 4 demonstrates that both the observation group and the control group's IL-8 and NLRP3 levels differed significantly during breastfeeding compared to before nursing, when both groups' levels were similar (P > 0.05). According to these findings, children with diabetes who had full nursing care had less inflammation.
Figure 4: Levels of IL-8 and NLRP3 in the two groups both before and after nursing Note: *P less than 0.05, compared with the control group.
Discussion
Chronic diabetes is a long-term illness. People's food habits, lifestyle modifications, and family history will all affect their chance of contracting the disease [17]. With the traits of a protracted illness and a sluggish rate of progression, the general trend is rising. Ketoacidosis is the primary sign of the disease in its early stages. The health and development of the ill youngsters would be severely impacted if the disease's progression is not stopped in a timely and efficient manner [18, 19]. Research and survey data have shown that children with diabetes have a chronically poor physical and psychological state that can lead to hypoglycemia coma. When long-term insulin treatment is combined with varying degrees of decreased sensitivity and insufficient insulin secretion, sick children have substantial postprandial blood glucose fluctuations, raising the risk of cardiovascular events. Nursing treatments should be implemented with caution because children with diabetes have low self-control and cognitive abilities [20].
Corresponding nursing interventions are required in clinical practice for children with diabetes in order to support the diseased child's recovery. The children's bodily function and self-consciousness are weak, and their age is comparatively young. Nursing and therapeutic therapy are therefore more challenging [21]. The routine nursing approach is neither systematic or planned for in practice, and it is not immediately apparent how this improves children's symptoms and signs [22]. The hospital's comprehensive nursing program for children with diabetes aimed to stabilize their blood glucose levels, improve the comfort of ill children, and ensure the quality of nursing services. The results showed that the observation group improved more on the blood glucose indicators (FPG, 2hPG, and HbAlc) than the control group, even if their SDS and SAS scores were lower. Furthermore, the observation group showed significantly higher rates of medication compliance among sick children compared to the control group. Furthermore, family members in the observation group reported higher levels of nurse satisfaction and quality of life compared to the control group. The study's findings showed that everyday life nursing helped lower blood glucose levels in diabetic youngsters. The following are the causes: Given the unique needs of young children, the management and treatment of diabetes involve a lengthy process for which the thoughtful, rational, and scientific nursing approaches chosen are crucial. The nursing needs of sick children cannot be met by conventional nursing because of its narrow focus and one model [23]. Comprehensive nursing is a type of contemporary nursing approach that emphasizes people-orientation and works to improve the physical and mental well-being of sick children by offering them high-quality, round-the-clock nursing care[24]. Among these is psychological comprehensive nursing, which provides support and advice to enhance family members' and sick children's trust in therapy as well as the psychological well-being of both groups [25]. To lower the likelihood of unfavorable outcomes, the comprehensive nursing of daily life directs the daily medication, insulin monitoring, and oral infection prevention for sick children [26]. Comprehensive nursing care for an ill child involves treating the child's symptoms as soon as possible and guiding their daily nutrition to improve their prognosis for recovery [27]. The purpose of health education is to dispel myths and increase awareness among family members of sick children. In sick children, blood lipids and blood sugar levels can be stabilized with diet and activity instruction. Children with illnesses no longer fear the medical setting thanks to humanistic care, which also strengthens the bond between nurses and patients, gives sick children the self-assurance they need to conquer their conditions, and treats them with hope and optimism [28].
Trimeric complexes containing caspase-1 precursor, NLRP3, and apoptosis-associated speck-like protein are known as the NLRP3 inflammasome. Certain immune cells, such as macrophages and dendritic cells, can activate caspase-1 when the intracellular NLRP3 protein and IL-1β precursor are upregulated. According to the source, this process promotes the development of IL-1β and IL-18 precursor and causes inflammation, which can manifest as damage to specific tissues or a broad inflammatory response [29]. Experiments in rats with type 2 diabetes have shown that diabetic cardiomyopathy can be ameliorated by lowering NLRP3 gene expression. [30]. Deactivating the NLRP3 inflammasome is one way epigallocatechin-3-gallate reduces inflammation and diabetes-induced glucose tolerance. [31]. The NLRP3 inflammasome is blocked by gastrodinamina in mice, which reduces cognitive deterioration and depressive-like behaviors. These findings suggest a potential role for the NLRP3 inflammasome in the onset of diabetes. The results showed that the levels of IL-8 and NLRP3 were significantly lower in the observation group compared to the control group. This lends credence to the idea that comprehensive nursing care helps lower the body's inflammatory response in unwell children, which improves their prognosis and delays the course of their disease.
Conclusion
It is recommended and appropriate to use comprehensive nursing to raise blood glucose levels, alleviate negative psychological effects, and increase nursing satisfaction in children with diabetes. The study's sample size is limited, so it is impossible to completely rule out bias in the results when comparing the clinical data from the two groups. In order to validate our findings, we therefore intend to carry out a prospective study involving more patients and follow-up.
References
- Oldridge, N.B., et al. (2001). Prevalence and outcomes of comorbid metabolic and cardiovascular conditions in middle-and older-age adults. Journal of clinical epidemiology, 54(9):928-934.
Publisher | Google Scholor - Patterson, C., et al. (2014). Diabetes in the young–a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes research and clinical practice, 103(2):161-175.
Publisher | Google Scholor - Raza, A., et al. (2022). Prevalence of hepatitis B virus infection among persons with hepatitis D virus and diabetes mellitus in Pakistan, 2019-2021. Archives of Hepatitis Research, 8(1):001-004.
Publisher | Google Scholor - Mazhar, M.W., et al., International Journal of Probiotics and Dietetics.
Publisher | Google Scholor - Kaul, K., et al. (2013). Introduction to diabetes mellitus. Diabetes: an old disease, a new insight, 1-11.
Publisher | Google Scholor - Giannini, C., et al. (2007). Role of physical exercise in children and adolescents with diabetes mellitus. Journal of Pediatric Endocrinology and Metabolism, 20(2):173-184.
Publisher | Google Scholor - Fulop, M.J. Diabetes and the family: Treatment manual for a family psychotherapy of recurrent diabetic ketoacidosis and recurrent hypoglycemia in children and adolescents. 1991: Pacific University Oregon Graduate School of Professional Psychology.
Publisher | Google Scholor - Tahrani, A.A., A.H. Barnett, and C.J. Bailey. (2016). Pharmacology and therapeutic implications of current drugs for type 2 diabetes mellitus. Nature Reviews Endocrinology, 12(10):566-592.
Publisher | Google Scholor - Chan, J.L. and M.J. Abrahamson. (2003). Pharmacological management of type 2 diabetes mellitus: rationale for rational use of insulin. in Mayo clinic proceedings. Elsevier.
Publisher | Google Scholor - Ollendick, T.H. and J.A. Cerny. (2013). Clinical behavior therapy with children. Springer Science & Business Media.
Publisher | Google Scholor - Meleis, A.I. (2011). Theoretical nursing: Development and progress. Lippincott Williams & Wilkins.
Publisher | Google Scholor - Marsiglio, W., Dads, kids, and fitness: A father's guide to family health. 2016: Rutgers University Press.
Publisher | Google Scholor - Dabravolski, S.A., et al. (2021). The role of mitochondrial mutations and chronic inflammation in diabetes. International journal of molecular sciences, 22(13):6733.
Publisher | Google Scholor - Poznyak, A., et al. (2020). The diabetes mellitus–atherosclerosis connection: The role of lipid and glucose metabolism and chronic inflammation. International journal of molecular sciences, 21(5):1835.
Publisher | Google Scholor - Jain, S.K., et al. (2009). Curcumin supplementation lowers TNF-α, IL-6, IL-8, and MCP-1 secretion in high glucose-treated cultured monocytes and blood levels of TNF-α, IL-6, MCP-1, glucose, and glycosylated hemoglobin in diabetic rats. Antioxidants & redox signaling, 11(2):241-249.
Publisher | Google Scholor - Di Virgilio, F. (2013). The therapeutic potential of modifying inflammasomes and NOD-like receptors. Pharmacological reviews, 65(3):872-905.
Publisher | Google Scholor - Asif, M. (2014). The prevention and control the type-2 diabetes by changing lifestyle and dietary pattern. Journal of education and health promotion, 3(1):1.
Publisher | Google Scholor - Jerram, S.T., M.N. Dang, and R.D. Leslie. (2017). The role of epigenetics in type 1 diabetes. Current diabetes reports, 17:1-11.
Publisher | Google Scholor - De Azevedo, J.C.V., et al. (2023). Biology and natural history of type 1 diabetes mellitus. Current Pediatric Reviews, 19(3):253-275.
Publisher | Google Scholor - Ohmann, S., et al. Cognitive functions and glycemic control in children and adolescents with type 1 diabetes. Psychological medicine, 40(1):95-103.
Publisher | Google Scholor - Mechanic, D. (1983). Adolescent health and illness behavior: Review of the literature and a new hypothesis for the study of stress. Journal of Human Stress, 9(2): 4-13.
Publisher | Google Scholor - Gormley-Fleming, E. and D. Martin. (2018). Children And young people's nursing skills at a glance. John Wiley & Sons.
Publisher | Google Scholor - Lawson, M.L., et al. (2005). A randomized trial of regular standardized telephone contact by a diabetes nurse educator in adolescents with poor diabetes control. Pediatric Diabetes, 6(1):32-40.
Publisher | Google Scholor - Leget, C. (2021). Humanist Approaches to Spiritual Care in Patient Counseling in the Netherlands, in Suffering in Theology and Medical Ethics. 2021, Brill Schöningh. 214-225.
Publisher | Google Scholor - Eccleston, C., et al. (2015). psychological interventions for parents of children and adolescents with chronic illness. Cochrane database of systematic reviews, (4).
Publisher | Google Scholor - Hockenberry, M.J. and D. Wilson. (2013). Wong's nursing care of infants and children multimedia enhanced version. 2013: Elsevier Health Sciences.
Publisher | Google Scholor - Child, W.H.O.D.o. and A. Health. (2000). Management of the child with a serious infection or severe malnutrition: guidelines for care at the first-referral level in developing countries. 2000: World Health Organization.
Publisher | Google Scholor - Zhang, C., et al. (2021). Epigallocatechin-3-gallate prevents inflammation and diabetes-Induced glucose tolerance through inhibition of NLRP3 inflammasome activation. International Immunopharmacology, 93:107412.
Publisher | Google Scholor - Abdullaha, M., et al. (2021). Tetramethoxystilbene inhibits NLRP3 inflammasome assembly via blocking the oligomerization of apoptosis-associated speck-like protein containing caspase recruitment domain: in vitro and in vivo evaluation. ACS Pharmacology & Translational Science, 4(4):1437-1448.
Publisher | Google Scholor - Ding, K., et al. (2022). The role of NLRP3 inflammasome in diabetic cardiomyopathy and its therapeutic implications. Oxidative Medicine and Cellular Longevity, 2022. 2022(1):3790721.
Publisher | Google Scholor - Zhang, C., et al. (2021). Epigallocatechin-3-gallate prevents inflammation and diabetes-Induced glucose tolerance through inhibition of NLRP3 inflammasome activation. International Immunopharmacology, 93:107412.
Publisher | Google Scholor