Research Article
Clinical Pharmacist’s Intervention in Identifying and Resolving Drug Therapy Problems in The Intensive Care Unit of a Tertiary Hospital in South-South Nigeria
- Okeroghene Aghogho Timipre 1
- Peter A. Owonaro 1*
- Joshua Funsho Eniojukan 1
- Sounyo Adekola Owonaro 1
- Awala E. Daughter 1
- Brisibe F. Seiyefa 2
1Faculty of Pharmacy, Dept of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
2College of Health Sciences, Dept of Family Medicine, Niger Delta University, Amassoma, Nigeria.
*Corresponding Author: Peter A. Owonaro, Faculty of Pharmacy, Dept of Clinical Pharmacy and Pharmacy, Niger Delta University, Amassoma, Nigeria.
Citation: Timipre O.A., Owonaro P.A., Eniojukan J.F., Owonaro S.A., Daughter A.E., et al. (2025). Clinical Pharmacist’s Intervention in Identifying and Resolving Drug Therapy Problems in The Intensive Care Unit of a Tertiary Hospital in South-South Nigeria, Journal of Clinical Research and Clinical Trials, BioRes Scientia Publishers. 4(1):1-10. DOI: 10.59657/2837-7184.brs.25.038
Copyright: © 2025 Peter A. Owonaro, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 10, 2024 | Accepted: January 02, 2025 | Published: January 07, 2025
Abstract
Drug Therapy Problems (DTPs), events compromising the therapeutic outcomes of drug therapy, are among the several problems hindering patient treatment, particularly in Intensive Care Units (ICUs). The study aims to evaluate the clinical pharmacist’s intervention in identifying and resolving Drug Therapy Problems (DTPs) in the Intensive Care Unit (ICU) of Federal Medical Center (FMC), Bayelsa State. The research, conducted in the ICU of Federal Medical Centre, Yenagoa, Bayelsa State, examined critically ill patients from July 1, 2023, to July 1, 2024. A prospective observational study examined the outcomes and implications of drug therapy problems. The study population included all patients admitted to the Federal Medical Centre, Yenagoa, Bayelsa State ICUs between 1st July 2023 and 1st July 2024. The study included all 160 patients admitted to the ICU of Federal Medical Center, Yenagoa, from 1st July 2023 to 1st July 2024, due to the infrequent availability of large numbers of critical care patients. Data was collected using the PCNE Foundation's DTPs Version 9.1 classification scheme, a comprehensive tool categorizing DTPs into five major sections, domains, and sub-domains, designed to capture the complexity of drug therapy management in the ICU. Combining PCNE classification with detailed patient demographics, including age, gender, ethnicity, medical history, current admission details, and treatment information, enables comprehensive dataset analysis to explore correlations between patient characteristics and DTP types and intervention effectiveness in various patient subgroups. The study obtained comprehensive ethical clearance from the health research ethics committee of the Federal Medical Center Yenagoa and adhered to ethical research principles. A total of 160 patients were screened for DTPs. Out of these 160 patients, males were 99(61.9%) and females were 61(38.1%). A majority of 55(34.4%) are between the ages of 65 and above. A mean number of approximately nine drugs were prescribed to patients during their stay in the ICU of FMC, Yenagoa with a co-morbidity of two ailments and a mean length of stay of eight days...The detailed results showed that the top specific causes of DTPs identified patients related 62 (38.8%) as the prevalent cause of DTPs, and the least 3(1.9%) were due to treatment duration. A majority of 83(51.9%) of the proposed interventions were not accepted. The majority intervention of 23(41.1%) cases reported was accepted but it was not implemented, the outcome of intervention shows that the majority of 71(44.4%) problems reported were partially solved. The study revealed a high prevalence of DTPs between July 2023 and July 2024, supported by mean values for co-morbidities, poly-pharmacy, and hospital stay, despite high intervention rates, low physician acceptance led to insignificant outcomes and drug effectiveness, highlighting the crucial role of clinical pharmacists in ensuring positive intervention outcomes and treatment effectiveness. Health institutions should foster collaboration between clinical pharmacists and other healthcare providers to increase clinical pharmacist services, thereby reducing Drug Therapy Problems and improving patient outcomes.
Keywords: drug therapy problems; clinical pharmacists; patient outcomes
Introduction
There are several problems in the cause of treatment of patients, especially in the Intensive Care Unit (ICU) of the healthcare system and one such problem is Drug Therapy problems (DTPs). Drug Therapy Problems (DTPs) are defined as events that compromise the therapeutic outcomes expected from drug therapy (Cipolle et al., 2012). The complexity of drug therapy, particularly for older adults, presents a significant challenge within the healthcare system (Steinman & Hanlon, 2010). As the number of medications prescribed increases, so does the risk of drug therapy problems (DTPs), which are exacerbated by the multifaceted nature of geriatric pharmacotherapy (Ahmad et al., 2014; Ertuna et al., 2019). The World Health Organization (WHO) has highlighted that more than half of all medications are not used as intended, leading to widespread misuse and improper administration by patients (WHO, 2014). This situation is even more dire in the Intensive Care Unit (ICU), where critically ill patients are particularly vulnerable. Drug Therapy Problems (DTPs) in such settings not only worsen clinical outcomes but also contribute to increased healthcare costs and heightened risks for patients. Studies have shown that patients in the ICU with unresolved DTPs experience longer hospital stays, incur higher medical expenses, and face double the risk of mortality compared to those without such complications (Tefera et al., 2020). The consequences of DTPs are multifaceted, adversely affecting clinical outcomes and escalating healthcare costs. The consequences of unresolved DRPs are severe, ranging from prolonged suffering to life-threatening conditions. However, it is well-documented that appropriate pharmacotherapy, when effectively managed, can significantly reduce the risk of these negative outcomes (Cipolle et al., 2012). The role of pharmacists is pivotal in this context, as they possess the expertise to identify, prevent, and resolve DTPs, thereby safeguarding patient safety and enhancing the efficacy of medications.
This study is therefore necessitated by the need to address DTPs, especially within the confines of Intensive Care Units (ICUs), where critically ill patients are at an elevated risk of drug-drug interactions, drug accumulation, and adverse drug events. These risks are attributed to the complex and often unstable conditions of ICU patients, necessitating meticulous management of their medication therapy (Ertuna et al., 2019). Clinical pharmacy emerged as a discipline dedicated to the optimization of medication therapy, with a strong emphasis on health promotion, wellness, and disease prevention. Clinical pharmacists, through their specialized skills, can substantially improve the quality of care for ICU patients. This can be achieved by conducting thorough medication reviews, enhancing the management of high-risk drugs, and curtailing unnecessary medical expenses, which are often a burden on healthcare systems (Al Rahbi et al., 2014). The backdrop of this study is therefore set against this broader context of drug misuse and its ramifications. The ICU setting presents a microcosm where the consequences of drug misuse and DTPs are magnified due to the vulnerability of the patient population. The interventions of clinical pharmacists in this setting are crucial, as they have the potential to mitigate the risks associated with complex drug regimens and to ensure that the goals of drug therapy are met with precision and care. The role of clinical pharmacy extends beyond the mere dispensing of medications. It encompasses a proactive approach to patient care, where pharmacists engage in collaborative practices with other healthcare professionals to optimize therapeutic outcomes. Their interventions are informed by a deep understanding of pharmacokinetics and pharmacodynamics, as well as a keen awareness of the individual needs of each patient. In the ICU, where patients are often unable to advocate for themselves due to their critical condition, the clinical pharmacist serves as a guardian of their medication-related well-being. The study's focus is on FMC, Bayelsa State, which provides a unique opportunity to explore the specific challenges and opportunities associated with drug therapy in a developing country's healthcare setting.
Aim of the Study
The aim of the study is to evaluate the clinical pharmacist’s intervention in identifying and resolving Drug Therapy Problems (DTPs) in the Intensive Care Unit (ICU) of Federal Medical Center (FMC), Bayelsa State.
Methodology
Study Area
The research was conducted in the Intensive Care Unit (ICU) of the Federal Medical Centre, Yenagoa, Bayelsa State where the most critically ill patients were treated. The study spanned through the period 1st July 2023, to 1st July 2024.
Study Design
For this study, a prospective observational design was adopted to explore the outcomes and implications of drug therapy problems (DTPs).
Population of the Study
For this research, the study population encompassed all patients admitted to the Intensive Care Units (ICUs) of the Federal Medical Centre, Yenagoa, Bayelsa State, from 1st July 2023 to 1st July 2024.
Sample Size
The sample size for the study is One Hundred and Sixty (160) patients. This sample size was based on a time-based sampling approach, as patients who required critical care in the hospital were not often available in large numbers. Instead of calculating a sample size, all patients who were on admission at the Intensive Care Unit (ICU) of the Federal Medical Center, Yenagoa, for the period between 1st July 2023 to 1st July 2024 were included in the study.
Data Collection
Data collection was achieved with the use of Pharmaceutical Care Network Europe (PCNE), the foundation’s classification scheme for Drug Therapy Problems (DTPs) Version (9.1) (Foppe et al., 2020). This classification scheme is a comprehensive tool designed to categorize and document the various types of DTPs encountered in clinical practices. The classification scheme was structured into five major sections, each with its domains and sub-domains. This structure facilitated a detailed categorization of DTPs as the domains and sub-domains were designed to capture the complexity of drug therapy management in the intensive care unit setting, where patients often had multiple comorbidities and were on complex medication regimens. In addition to the PCNE classification scheme, a section for patients’ demographics was developed to collect relevant patient demographic characteristics. The patient data collected included age, gender, and ethnicity, as well as relevant medical history, including comorbidities, allergies, and history of previous hospitalizations. Additionally, information on the current admission, such as the reason for admission, presenting symptoms, and initial treatment, was captured. Combining the patient demographic data with the PCNE classification scheme created a comprehensive dataset, allowing researchers to explore potential correlations between patient characteristics and the types of DTPs encountered, as well as the effectiveness of interventions in different patient subgroups (Foppe et al., 2020).
Reliability and Validity
The reliability of the instrument was tested by its administration on patients outside the study sample before it was administered to sample patients for the study. The validity was determined by a rigorous assessment process conducted by senior clinical pharmacists, who were also academicians and researchers. They evaluated the tool for face validity, ensuring that it appeared to measure what it was supposed to measure.
Ethical Approval
A comprehensive ethical clearance was obtained from the health research ethics committee of the Federal Medical Center Yenagoa before embarking on the study with a commitment to uphold the principles of ethical research throughout the study. The measures taken to obtain permissions, and consent, maintain confidentiality and privacy, minimize risks, communicate benefits, and secure ethical clearance demonstrated the study's commitment to ethical excellence. These efforts not only protected the participants but also enhanced the credibility and validity of the research findings.
Results
Data obtained from the administration of questionnaires on patients in the Intensive Care Unit (ICU) of Federal Medical Centre (FMC), Yenagoa were descriptively analyzed using frequencies, percentages, mean, standard deviation, and charts, and the hypotheses were inferentially tested using PPMCC. 160 patients constitute the total of the patients admitted into the Intensive Care Unit (ICU) for the period 1st July 2023 to 1st July 2024 and was consequently used for the analysis.
Demographics of Sampled Patients
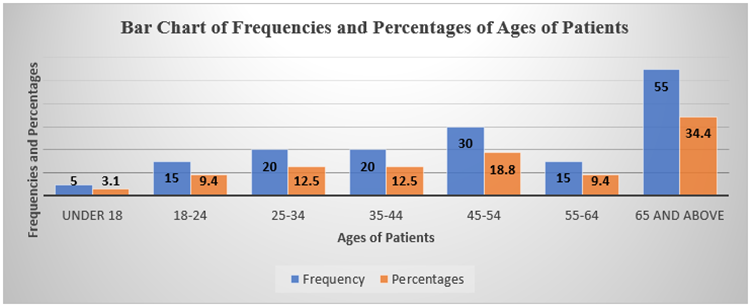
Figure 1: Bar Chart of Ages of Respondents.
The study revealed that 5(3.1%) out of 160 patients admitted and administered the questionnaire were under 18 years. 15(9.4%) are within the ages of 18-24, 20(12.5%) are within the ages of 35-44, 30(18.8%) are within the ages of 45-54, 15(9.4%) are within the ages of 55-64 and a majority of 55(34.4%) are within the ages of 65 and above.
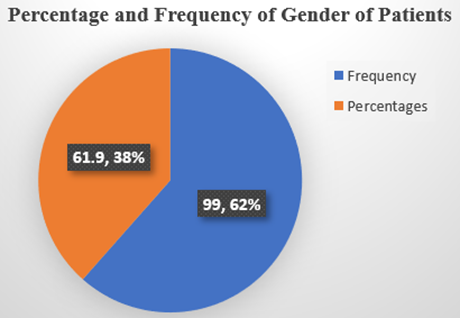
Figure 2: Gender of Patient.
The result from Figure 2 shows that 99(61.9%) of patients administered with the questionnaire in the ICU are male while 61(38.1%) are female.
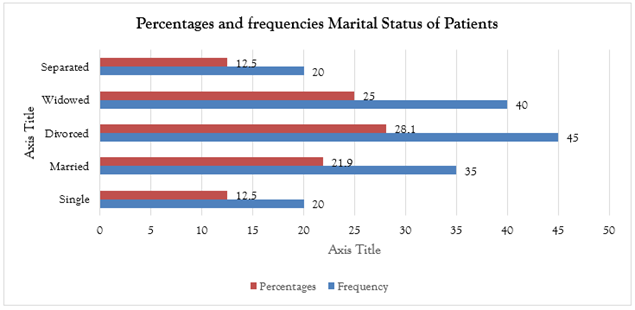
Figure 3: Marital Status.
The result from Figure 3 shows that 20(12.5%) out of 160 patients admitted and administered questionnaire are single, 35(21.9%) are married, 45(28.1%) are divorced, 40(25.0%) are widowed and 20(12.5%) are separated. This implies that the majority of the respondents are divorced and widowed.
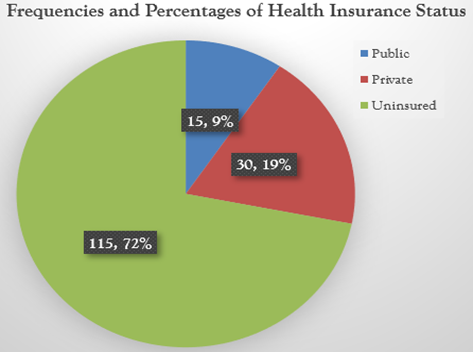
Figure 4: Health Insurance Status.
The results from Figure 4 show that 15(9.4%) out of 160 patients admitted and administered the questionnaire have public Health Insurance Status, 30(18.8%) have private Health Insurance Status, and the majority of 115(71.9%) are uninsured. This implication of the findings is that most people are not covered by health insurance schemes. This makes people to be more vulnerable to health challenges.
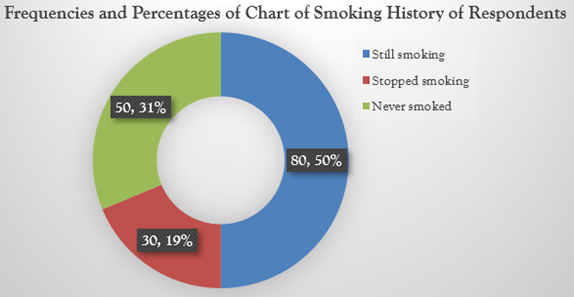
Figure 5: Smoking History.
The result from Figure 5 shows that the majority of 80(50.0%) out of 160 patients admitted and administered the questionnaire still smoke, 30(18.8%) have stopped smoking and 50(31.3%) have no smoking history. The high number of patients who smoke is an indication of a possible complication of the treatment process and vulnerability to Drug Therapy Problems (DTPs).
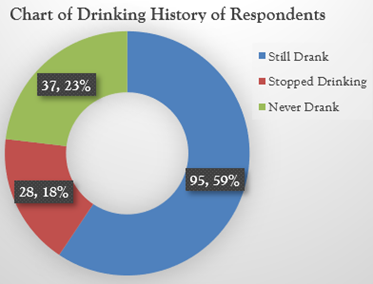
Figure 6: Drinking History.
The result of the findings of the study from Figure 6 shows that the majority of 95(59.4%) out of 160 patients still drink, 28(17.5%) have stopped drinking and 37(23.1%) have never drank. This implies that the majority of patients still drink. This also is an indication of a possible complication of the treatment process and vulnerability to Drug Therapy Problems (DTPs).
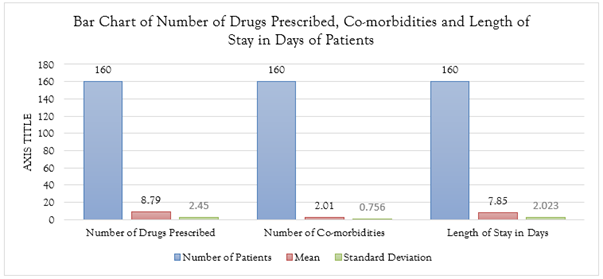
Figure 7: Mean Number of Drugs Prescribed, Co-morbidities, and Length of Stay in Days.
The result from Figure 7 revealed that a mean number of approximately nine drugs were prescribed to patients during their stay in the ICU of FMC, Yenagoa with a co-morbidity of two ailments and a mean length of stay of eight days. These are indications that cases of DTPs-related problems were highly prevalent in the ICU of FMC during the study period.
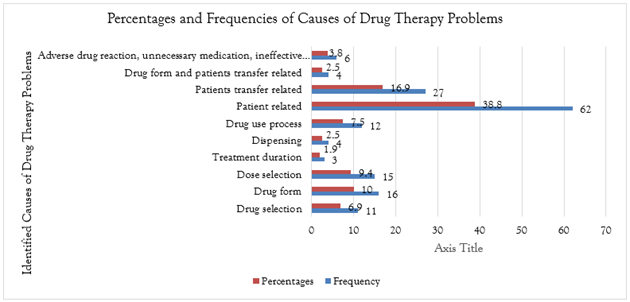
Figure 8: Prevalence and causes of DTPs.
The result from Figure 8 identified patients related 62 (38.8%) as the prevalent cause of DTPs, followed by patient transfer 27(16.9%), 16(10.0%) reported drug form, 15(9.4%) reported dose selection, 12(7.5%) was as a result of drug use process and 11(6.9%) reported drug selection. Furthermore, 6(3.8%) were caused by other factors such as adverse drug reaction, unnecessary medication, ineffective medication, and mixed medication, 4(2.5%) were as a result of drug dispensing and drug form while 3(1.9%) were due to treatment duration.
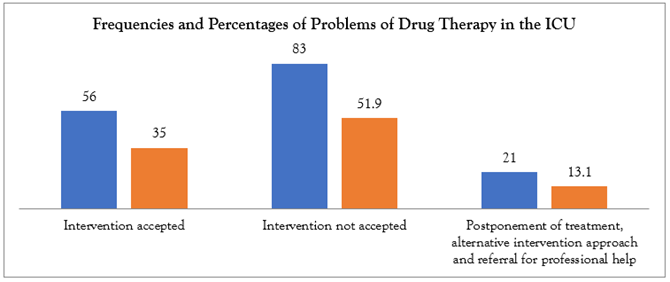
Figure 9: Proportion of DTPs Propose Interventions by the Clinical Pharmacist that was accepted and Implemented by the ICU Physician.
The result from Figure 9 shows that 56(35.0%) of Drug Therapy Problems (DTPs) in the ICU had pharmacist intervention proposals accepted, the majority of 83(51.9%) of the proposed interventions were not accepted and 21(13.1%) was attributed to others factors such as postponement of treatment, alternative intervention approach and referral for professional help.
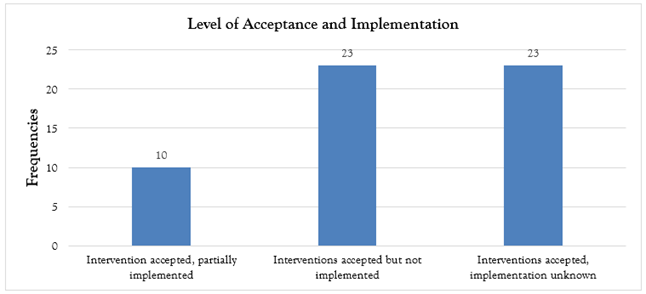
Figure 10: Level of Intervention Acceptance and Implementation.
The result from Figure 10 revealed that 10(35.0%) out of 56 proposed interventions by the clinical pharmacist reported that interventions were accepted and partially implemented. The majority of 23(41.1%) of the cases reported that though the intervention was accepted it was not implemented and 23(41.1%) also reported that interventions were accepted but the implementation was unknown. This implies that even though less than the majority of 56(35.0%) out of 160 clinical pharmacist intervention proposals were accepted, still majority of the proposals that were accepted were either not implemented or partially implemented or the implementation was not known. This is an indication of the lack of synergy between the Clinical Pharmacist and the ICU Physician.
Figure 11: Outcome of the Intervention.
The result from Figure 11 on the outcome of intervention shows that in 31(19.4%) of the cases reported, the problem status was unknown, 51(31.9%) reported that the problem was solved, majority of 71(44.4%) reported that the problem was partially solved and 7(4.4%) reported that problems were not solved.
Pharmaceutical Care Network Europe Summary of Key Findings
The result of the analysis of data obtained from the administration of 160 PCNE questionnaires on patients in the Intensive Care Unit (ICU) of Federal Medical Centre (FMC), Yenagoa using frequencies, percentages, and charts revealed that the majority of patients within the study period are not covered by health insurance schemes. This makes people to be more vulnerable to health challenges. The study further revealed that a mean number of approximately nine drugs were prescribed to patients during their stay with a co-morbidity of two ailments and a mean length of stay of eight days. These are indications that cases of DTPs-related problems were highly prevalent in the ICU of FMC during the study period. The study also confirmed that the majority of patients within the study period still smoke and drink. The high number of patients who still smoke and drink is an indication of a possible complication of the treatment process and vulnerability to Drug Therapy Problems (DTPs). The study identified patient-related as the most prevalent cause of DTPs, followed by patient transfer, drug form, dose selection, drug use process, and drug selection. Also, other factors such as adverse drug reactions, unnecessary medication, ineffective medication, and mixed medication were identified as causes followed by drug dispensing, drug form, and treatment duration. The result revealed that the majority of the proposed interventions of the Clinical Pharmacist were not accepted by the physician. It further confirms that even in cases where it was accepted, the majority of the cases reported, that though intervention was accepted it was not implemented. It also reported that in some cases interventions were accepted but the implementation was unknown. This implies that even though less than the majority of clinical pharmacist intervention proposals were accepted, still majority of the proposals that were accepted were either not implemented or partially implemented or the implementation was not known. This is an indication of the lack of synergy between the Clinical Pharmacist and the ICU Physician. The result on the outcome of intervention shows that 31(19.4%) of the cases reported problem status was unknown, 51(31.9%) reported that the problem was totally solved, majority of 71(44.4%) reported that the problem was partially solved and 7(4.4%) reported that problems were not solved. This is an indication that the majority of DTPs in the study facility were not addressed.
Discussion
The current study shares similarities and contradictions with several literature findings from previous studies in terms of findings and implications. One such noticeable difference relates to the acceptance and actual implementation rate of proposed interventions by the clinical pharmacist. Sociodemographic factors of the patients, such as a history of smoking, intake of alcohol, and co-morbidities, are poorly and insignificantly related to the effectiveness of therapy with drugs and interventions. These factors are not strong predictors of treatment outcomes within the ICU environment. Findings from this study emphasize improved interprofessional collaboration, integration of clinical pharmacists into ICU teams, targeted training and education of healthcare professionals, and a holistic approach to the care provided for patients. Larger, longitudinal studies are needed in future research to explore the complex relationships that exist among DTPs, interventions, and patient outcomes in the ICU setting. There was also a negative correlation in the prevalence of DTP with intervention outcomes, r = -0.369, p = 0.013, wherein the higher the DTP prevalence, the less favorable the outcomes of interventions (Okwonu et al., 2020). They attributed this to various factors like poor acceptance rates of proposed interventions, complexity of inpatient cases, and limitations in the role of a clinical pharmacist.
Whereas the general trend of this study is comparable to literature findings, there are a few observed differences when compared to other similar investigations. The findings of this study are contrary to the study from the Turkish university hospital ICU. According to Albayrak et al. (2022), most of the suggestions that the clinical pharmacist in that study made were largely embraced and implemented by the physicians throughout the operating room in the ICU of the setting of the current study. Whereas, in the current study, physicians in the ICU refused 51.9% of proposed interventions. This contrasts with the higher rates of acceptance and subsequent implementation seen in such studies as Niriayo et al., 2024; Babirye et al., 2023; Paisansirikul et al., 2021. This can indicate that the rate of acceptance of pharmacists is lower, possibly due to barriers between inter-professional communication and collaboration with physicians, responsible for the limited effects of pharmacist interventions on patient outcomes.
Another divergence involves the exact nature of factors involved in treatment effectiveness and the outcome of interventions. Although previous literature has always pinpointed the patient-related factors of age, comorbid conditions, and medication history as being significant in DTPs, the same from Niriayo et al. (2024), Baye et al. (2023), and Paisansirikul et al. (2021) were confirmed in this present study, adding that smoking and alcohol history negatively affected efficiency in treatment and intervention outcome in an ICU environment. This represents a unique finding; therefore, it places into perspective the consideration of patient-specific lifestyle factors in the development of comprehensive medication management approaches.
This is further in contrast to the study by Liang et al. conducted in nursing homes with integrated medical and old-age care in China in 2024, which found that the prevalence of DTPs was lower than that in a traditional care setting. The current study found a high burden of DTPs in the ICU. This may be attributed to particularities within the patient population and the provided care in this setting. While many identified studies indeed reported positive impacts of clinical pharmacist interventions on patient outcomes, such as those by Lekpittaya et al. (2024) and Aderemi-Williams et al. (2021), the current study could not establish a significant positive impact of the proposed interventions on the health outcomes of the ICU patients. The limited acceptance and implementation of recommendations offered by a clinical pharmacist in the setting of the study may be a contributory factor to the observed difference. The current study examined in more detail the types of specific interventions made by the clinical pharmacist and the duration spent completing them. That the interventions targeting drug levels generally were more time-consuming for the pharmacist to complete, unlike those at the prescriber or patient level, brings important nuances into the complexity and resourcing implications of addressing DTPs in the setting of the ICU. This in turn could be used to underpin the allocation of pharmacist resources in terms of implementing specific, focused training programs that could further improve the efficiency and effectiveness of pharmacist-led interventions. Contrasts with earlier studies realized in this current study highlight difficulties and dynamics within the setting of the ICU, which may require adapted strategies in handling prevailing problems of drug therapy. Lower acceptance rates for pharmacist interventions and identification of specific patient-related factors as predictors of effectiveness call for an increase in inter-professional collaboration and more patient-centered strategies to optimize medication management in the critical care setting. Overall, the comparison to the available literature showed similarities in the prevalence and pattern of DTPs and contributing factors but revealed some context-specific differences regarding the implementation and impact of clinical pharmacist interventions that may relate to unique characteristics of the study setting and healthcare system.
Conclusion
This study identified a high prevalence of DTPs in the study area within the period between 1st July 2023 to 1st July 2024 which is confirmed by the presence of mean values of 2 for co-morbidity, 11 for poly-pharmacy, and 7 days for hospital stay. Though, the rate of proposed intervention provided was high acceptance from the physician was low resulting in low positive and insignificant intervention outcomes and drug effectiveness contrary to studies with high acceptance rates. This is an indication that the role of clinical pharmacists in the identification and resolution of DTPs is fundamental in ensuring positive intervention outcomes and treatment effectiveness.
Recommendations
Based on the findings, it is recommended that health institutions should encourage clinical pharmacist service by increasing synergy with other health professionals to reduce the problems associated with Drug Therapy Problems (DTPs) so as to enhance patients’ drug therapy outcomes.
Public Health Implication
This study of clinical pharmacist interventions in the ICU of FMC, a tertiary hospital in South-South Nigeria holds an implication for health professionals, policymakers, researchers, and public health. For health professionals, this means developing better interprofessional collaboration, targeted training and education, optimization of the role of the clinical pharmacist, and adopting a more patient-centered approach to care. The relatively low rates of acceptance and implementation of pharmacist interventions point to the need for improved communication and shared decision-making among the ICU staff. Policymakers should support the empowerment of the clinical pharmacist in critical care, gains in health care and health insurance, and interprofessional education and collaboration. Public health implications include the probable improved interprofessional collaboration to enhance patient outcomes, the need for patient-centered care related to either smoking or alcohol history, the development of the clinical pharmacist's function in ICUs, and the call to improve healthcare access related to insurance problems. Addressing these implications would hopefully translate into better management of drug therapies in ICUs, improved outcomes for patients, and improved public health in resource-constrained settings.
Authors' Conflict of Interest
There was no conflict of interest among the authors. The researchers appreciated the statistician, participants, and researchers for the time.
References
- Aderemi-Williams, R. I., Nduaguba, S. O., Akoji, E. M., Ogbo, P. U., Abah, I. O. (2021). Drug Therapy Problems Identified Among Patients Receiving Antiretroviral Treatment in A HIV Clinic: A Prospective Study in North Central, Nigeria. Pan African Medical Journal, 40(1).
Publisher | Google Scholor - Ahmad, A., Mast, M. R., Nijpels, G., Elders, P. J., Dekker, J. M., et al. (2014). Identification of Drug-Related Problems of Elderly Patients Discharged from Hospital. Patient Preference and Adherence, 155-165.
Publisher | Google Scholor - Albayrak, A., Başgut, B., Bikmaz, G. A., Karahalil, B. (2022). Clinical Pharmacist Assessment of Drug-Related Problems Among Intensive Care Unit Patients in A Turkish University Hospital. BMC Health Services Research, 22(1):79.
Publisher | Google Scholor - Al Rahbi, H. A. M., Al-Sabri, R. M., Chitme, H. R. (2014). Interventions by Pharmacists in Out-Patient Pharmaceutical Care. Saudi Pharmaceutical Journal, 22(2):101-106.
Publisher | Google Scholor - Babirye, M., Yadesa, T. M., Tamukong, R., Obwoya, P. S. (2023). Prevalence and Factors Associated with Drug Therapy Problems Among Hypertensive Patients at Hypertension Clinic of Mbarara Regional Referral Hospital, Uganda: A Cross-Sectional Study. Therapeutic Advances in Cardiovascular Disease, 17:17539447231160319.
Publisher | Google Scholor - Baye, T., Girmaw, F., Ashagrie, G., Kassaw, A. T. (2023). Drug Therapy Problems and Associated Factors Among Hypertensive Patients in North Wollo Public Hospitals, Northeast Ethiopia: Institutional-Based Cross-Sectional Study. Integrated Blood Pressure Control, 47-57.
Publisher | Google Scholor - Cipolle, R. J., Strand, L. M., Morley, P. C. (2012). Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management. New York: McGraw-Hill Medical. 435-644.
Publisher | Google Scholor - Ertuna, F., Aydin, A., Yilmaz, S. (2019). Drug Therapy Problems in Intensive Care Units: A Systematic Review. Journal of Clinical Pharmacy and Therapeutics, 44(3):326-336.
Publisher | Google Scholor - Foppe van Mil, J. W., Horvat, N., Westerlund, T., Richling, I. (2020). Classification for Drug-Related Problems (V9.1). Pharmaceutical Care Network Europe Association.
Publisher | Google Scholor - Herledan, C., Cerfon, M. A., Baudouin, A., Larbre, V., Lattard, C., et al. (2023). Impact of Pharmaceutical Care Interventions on Multidisciplinary Care of Older Patients with Cancer: A Systematic Review. Journal of Geriatric Oncology, 14(4):101450.
Publisher | Google Scholor - Lekpittaya, N., Kocharoen, S., Angkanavisul, J., Siriudompas, T., Montakantikul, P., et al. (2024). Drug-Related Problems Identified by Clinical Pharmacists in An Academic Medical Center in Thailand. Journal of Pharmaceutical Policy and Practice, 17(1):2288603.
Publisher | Google Scholor - Niriayo, Y. L., Gebregziabher, T., Demoz, G. T., Tesfay, N., Gidey, K. (2024). Drug Therapy Problems and Contributing Factors Among Patients with Epilepsy. PLoS one, 19(3):e0299968.
Publisher | Google Scholor - Niriayo, Y. L., Kifle, R., Asgedom, S. W., Gidey, K. (2024). Drug Therapy Problems Among Hospitalized Patients with Cardiovascular Disease. BMC Cardiovascular Disorders, 24(1):50.
Publisher | Google Scholor - Okwonu, F. Z., Asaju, B. L., Arunaye, F. I. (2020). Breakdown Analysis of Pearson Correlation Coefficient and Robust Correlation Methods. In IOP Conference Series: Materials Science and Engineering. IOP Publishing. 917(1):012065.
Publisher | Google Scholor - Paisansirikul, A., Ketprayoon, A., Ittiwattanakul, W., & Petchlorlian, A. (2021). Prevalence and Associated Factors of Drug-Related Problems Among Older People: A Cross-Sectional Study at King Chulalongkorn Memorial Hospital in Bangkok. Drugs-Real World Outcomes, 8:73-84.
Publisher | Google Scholor - Steinman, M. A., Hanlon, J. T. (2010). Polypharmacy In Older Adults: A Complex Clinical Challenge. Journal of the American Geriatrics Society, 58(7):1247-1254.
Publisher | Google Scholor - Tefera, G. M., Zeleke, A. Z., Jima, Y. M., Kebede, T. M. (2020). Drug Therapy Problems and The Role of Clinical Pharmacist in Surgery Ward: Prospective Observational and Interventional Study. Drug, Healthcare and Patient Safety, 71-83.
Publisher | Google Scholor - World Health Organization. (2014). Global Status Report on Noncommunicable Diseases 2014.
Publisher | Google Scholor