Case Report
Case Report of Primary PCI with Covered Stent in Coronary Ectesia in Acute Myocardial Infarction
1Interventional Cardiologist, Golden Heart Hospital, Jabalpur, Madhya Pradesh, India.
2Non Invasive Cardiologist, Golden Heart Hospital, Jabalpur, Madhya Pradesh, India.
3Consultant Pulmonologist, Golden Heart Hospital, Jabalpur, Madhya Pradesh, India.
4Consultant Gynecologist, Golden Women Care Hospital, Jabalpur, Madhya Pradesh, India.
*Corresponding Author: Pushpraj Patel, Interventional Cardiologist, Golden Heart Hospital, Jabalpur, Madhya Pradesh, India.
Citation: Patel P, Mishra A, Patel A, Patel KS. (2024). Case Report of Primary PCI with Covered Stent in Coronary Ectesia in Acute Myocardial Infarction, Journal of Clinical Cardiology and Cardiology Research, BioRes Scientia Publishers. 3(3):1-5, DOI: 10.59657/2837-4673.brs.24.036
Copyright: © 2024 Pushpraj Patel, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 13, 2024 | Accepted: September 12, 2024 | Published: September 20, 2024
Abstract
Introduction: By definition, coronary artery ectasia (CAE) also called as aneurysmal coronary artery disease is a dilatation exceedingly more than one-third of the coronary artery length with the diameter of the dilated segment measuring more than 1.5 times the diameter of a normal adjacent segment.
Case Presentation: Our case is a 58-year-old male with prior medical problems under regular treatment and on anti-platelets medication too, who presented to the ER with an acute anferior wall ST elevation myocardial infarction (STEMI). The Coronary angiogram revealed large ectatic segment in the left anterior descending coronary artery (LAD) with 100% stenosis in the middle segment. Upon POBA of the LAD a big clot burden was noted on the ectatic segment. We planned to keep him on HEPARIN infusion after thrombolysis with streptokinase for 24 hours. Then again Cath showed complete resolution of the clot and the lesion was stented with drug eluting covered stent showing excellent final result further he was managed with NOAC and aspirin orally.
Discussion: We found that our case is interesting and unique in exploring the association of CAE that presents with acute MI and how to treat it safely in the primary PCI setup in Cath lab. CAE is not a usual finding during CAG. Usually, CAE patients are asymptomatic but CAD symptoms can be seen. There is still no standard treatment specific for CAE itself, but when presenting with acute MI management is directed by the CAD guidelines while keeping in consideration practical approach. We reviewed the literature of CAE presentation, etiology, differential diagnosis and treatment and discussed the most appropriate antithrombotic therapy for our patient of acute MI with CAE. As per the current evidence, use of prophylactic antiplatelet and anticoagulant in these patients is preferred, RCT and studies are needed to determine the best form and duration of antithrombotic therapy.
Conclusion: Presently there is no standard operating protocol for CAE with CAD. Bio statistically more significant large scale multi centric trials are required to be done so that standard guidelines can be devised by professional societies.
Keywords: coronary artery ectasia; coronary aneurysm; coronary artery disease; myocardial infarction
Introduction
Coronary artery ectasia (CAE), also known as aneurysmal coronary artery disease. Coronary artery ectasia (CAE) is a dilation of the coronary artery lumen. Ectasia is diffuse dilation of a coronary artery and coronary aneurysm is focal coronary dilation [1]. The definition of coronary artery ectasia is “a dilatation exceedingly more than one-third of the coronary artery length with the diameter of the dilated segment measuring more than 1.5 times the diameter of a normal adjacent segment” [2]. It is uncommon but well recognized finding in CAG.
Types and classification of CAE is divided into four groups [2]. Type 1 is diffuse ectasia involving 2 or 3 coronaries. Type 2 is diffuse ectasia in one coronary and localized in another vessel. Type 3 is diffuse ectasia in one coronary only. Type 4 is localized or segmental involvement.
CAE is infrequent finding in CAG, but is a well-recognized entity with 1.2-4.9% prevalence and male preponderance of 3:1 male: female ratio [1,3]. CAE in children and young usually associated with Kawasaki disease and fungal or septic emboli, Marfan syndrome, arteritis from polyarteritis nodosa, Takayasu disease, or systemic lupus erythematosus.
CAD risk factors associated are atherosclerosis with CAE [1,2,4]. On observation 90.8% of patients with CAE were found to have CAD [1]. While most patients are asymptomatic, some may present with symptoms of CAD incidence varies between 0.3% and 4.9% [4,5]. As per CASS registry, coronary artery ectasia is seen in 4.9% of coronary angiograms. CAE can be small if vessel size under 5 mm, medium if vessels size 5 to 8 mm, and giant if vessel size over 8 mm [4]. Based on location most common lesion location is seen in the right coronary artery (68%), proximal left anterior descending (60%), and left circumflex (50%) [4]. Based on shape CAE can be saccular when the transverse diameter is more than the longitudinal diameter and fusiform when the longitudinal diameter is more than the transverse diameter.
The prognosis for CAE is directly related to the severity of CAD. CAE can in association with CAD cause more MACE than Isolated CAE, but CAE still carries the risk of myocardial ischemia and infarction. Type 1 and Type 2 CAE demonstrate a higher risk than Type 3 and type 4 CAE. There is no data backed relationship between the diameter of an artery and the outcome [1]. Here we present a case of a male with CAE who presented with symptoms of ST elevation myocardial infarction (STEMI).
Case Presentation
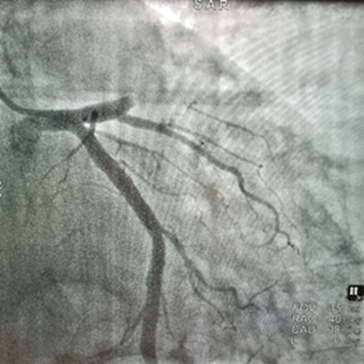
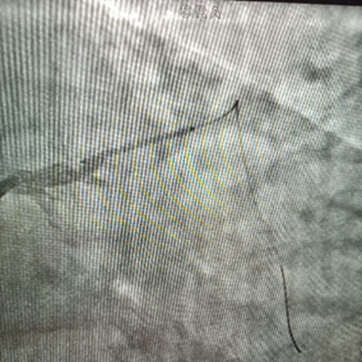
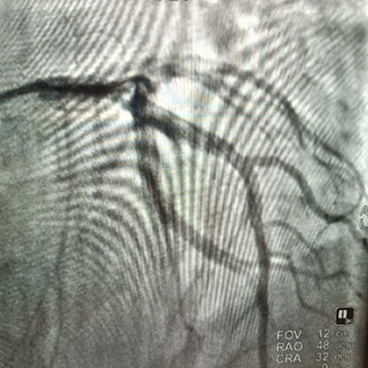
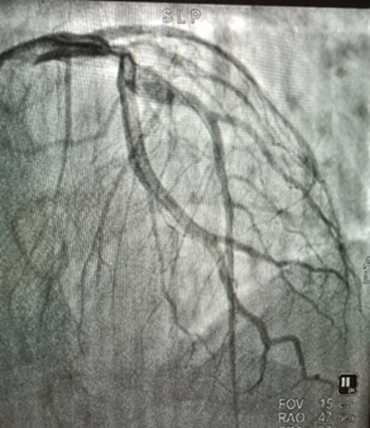
Our patient is a medically under treatment for type 2 diabetes and hypertension and current smoker 58-year-old male who presented to the ER with severe chest pain. His initial ECG showed ST segment elevation in lead V1 to V6 and lead 1, AVL, he was diagnosed to have an acute anterior wall STEMI. He was taken to Cath lab for primary PCI and initial coronary angiogram showed normal left main and left circumflex (LCX), right coronary artery (RCA) arteries, total occlusion in proximal left anterior descending artery (LAD), POBA was done and after establishing coronary flow revealed long longitudinal type 3 ectatic segments with 100% thrombotic occlusion with stenosis in the proximal and middle segment of the LAD He underwent thrombolysis with streptokinase and followed by heparin infusion for next 24 hours and in second re Cath after crossing the lesion, coronary angiography showed ectatic segment and the lesion was stented by a drug eluting covered stent 5 × 22 with excellent final result.
Figure 1: Primary CAG showing proximal LAD 100 % Occlusion.
Figure 2: Big clot burden on ectatic segment as shown.
Figure 3: Complete resolution of the clot after thrombolysis with streptokinase and heparin infusion.
Figure 4: Covered stent placement in LAD covering stenosis and CAE.
Figure 5: Patent LAD after stenting. Complete revascularization with no clot.
Discussion
CAE is seen in coronary vessels, classified based on configuration, which categorizes the lesion by measurements into transverse saccular diameter more than longitudinal, transverse or fusiform diameter less than longitudinal length [4].
Another classification is based on the degree of ectasia and number of vessels involved as described by Markis et al. [7]. 1. Diffuse ectasia in two or three vessels, 2. Diffuse ecatsia involving one vessel and localized disease in another. 3. One vessel with diffuse ectasia. 3. One vessel with localized disease.
The CAE most commonly involve was RCA in the proximal and middle segments then LAD then LCX and raely left main [1,3]. Likewise, our patient had an ectatic segment in LAD and total occlusion of the proximal part of LAD while the other coronary arteries were completely lesion free.
By research specific mechanism leading to CAE is still not very well established, risk factors and pathophysiology behind CAD and CAE are overlapping e.g., vascular remodeling and atherosclerosis [4]. Other risk factors are with male preponderance, hypertension, dyslipidemia and smoking [1,4]. Type 2 DM is often independent factor. May be related to CAE are vasculitis (Kawasaki disease, polyarteritis nodosa), connective tissue diseases (rheumatoid arthritis, systemic lupus erythematous, scleroderma), Marfan syndrome, and iatrogenic causes (stenting, angioplasty, coronary atherectomy) [4-7]. There are many cofounders involved in the process, so patients with CAE can present with other symptoms of the coexistent disease.
Studies showed angina as the most common presenting symptom of patients with CAE with CAD while other studies denied any specific symptom related to the disease [4,5]. The clinical picture of a patient with CAE may include symptoms of acute coronary syndromes (ACS) due to the turbulent blood flow in diseased vessels and thrombus formation [4,5,7]. Angina, myocardial infarction (MI), positive exercise stress test, or ST-elevation in ECG [2,5,7]. Similarly, our patient presented with chest pain and inferior STEMI due to the complete stenosis of the RCA following the ectatic segment. Furthermore; even with the development of imaging techniques such as coronary magnetic resonance angiogram (MRA) and coronary computed tomography angiogram (CTA), coronary angiography remains the gold standard for diagnosing CAE [4,7].
On discharge treatment should include all co existent disease and it should be comprehensive. Medical, angioplasty, and surgical modalities form mainstay of treatment. Aim is towards risk reduction in addition to management of CAD for obstructive lesions [1,5]. Aspirin is useful in asymptomatic CAE patients with risk factors to prevent MI possible other medications such as anticoagulants and combined antiplatelet with adenosine diphosphate inhibitors have to be evaluated on head-to-head trials [4]. Percutaneous coronary intervention (PCI) is indicated for patients with significant CAD or MACE in association with CAE [4,9]. PCI using drug coated covered stents was shown to be superior. Our patient was treated eventually with PCI covered drug coated stent but after anti thrombotic so that revascularization remain uncomplicated. Surgery and coiling are another option for CAE It may also be a better option for large aneurysms with an increased chance of rupturing [4]. CAE is a kind of atherosclerosis that occurs in 3% to 8% of coronary angiography operations for diagnostic purposes. When it comes to CAE, there is currently no agreed-upon treatment plan [10].
Differential diagnosis is Atherosclerosis, Bacterial syphilis, Behcet’s disease, Ehler-Danlos syndrome, Fibromuscular dysplasia, Giant cell arteritis, Kawasaki disease, Marfan’s syndrome, Mycotic aneurysm.
Conclusion
CAE is an uncommon finding during coronary angiography. It is highly associated with many CAD risk factors and etiologies as well as pathologic progression. Patients with CAE are usually asymptomatic and present only when having occlusive symptoms or detected during angiography. However, management in CAE with CAD is guided by the extent of CAD and its guidelines. Lack of standard operating protocols specific for CAE need to be studied and explained.
Abbreviation
CAE- Coronary artery ectasia
CAD- coronary artery disease
STEMI- ST elevation myocardial infarction
LCX- Left circumflex coronary artery
LAD- left anterior descending artery
RCA- right coronary artery
DM- Diabetes mellitus
ACS- acute coronary syndrome
MI- myocardial infarction
NOAC- Novel oral anti coagulants
PCI- percutaneous coronary intervention
MACE- major acute cardiac event
Declarations
Conflict of Interests
No Competing Interests.
Funding
This is not funded by any agency or institution.
References
- Swaye PS, Fisher LD, Litwin P, Vignola PA, Judkins MP, et al. (1983). Aneurysmal Coronary Artery Disease. Circulation. 67(1):134-138.
Publisher | Google Scholor - Hartnell GG, Parnell BM, Pridie RB. (1985). Coronary Artery Ectasia. Its Prevalence and Clinical Significance In 4993 Patients. Heart. 54(4):392-395.
Publisher | Google Scholor - Gunes Y, Boztosun B, Yildiz A, Esen AM, Saglam M, et al. (2006). Clinical Profile and Outcome of Coronary Artery Ectasia. Heart. 92(8):1159-1160.
Publisher | Google Scholor - Devabhaktuni S, Mercedes A, Diep J, Ahsan C. (2016). Coronary Artery Ectasia- A Review of Current Literature. Current Cardiology Reviews. 12(4):318-323.
Publisher | Google Scholor - Ozcan OU, Gulec S. (2013). Coronary Artery Ectasia. Cor et Vasa. 55(3):e242-e247.
Publisher | Google Scholor - Demopoulos VP, Olympios CD, Fakiolas CN, Pissimissis EG, Economides NM, et al. (1997). The Natural History of Aneurysmal Coronary Artery Disease. Heart. 78(2):136-141.
Publisher | Google Scholor - Markis JE, Joffe CD, Cohn PF, Feen DJ, Herman MV, Gorlin Ret al. (1976). Clinical Significance of Coronary Arterial Ectasia. American Journal of Cardiology. 37(2):217-222.
Publisher | Google Scholor - Akram Kawsara, Iván J. Núñez Gil, Fahad Alqahtani, Jason Moreland, Charanjit S. Rihal et al. (2018). Coronary Artery Aneurysms. J Am Coll Cardiol Intv. 11(13):1211-1223.
Publisher | Google Scholor - Luca Esposito, Marco Di Maio, Angelo Silverio, et al. (2022). Treatment and Outcome of Patients with Coronary Artery Ectasia: Current Evidence and Novel Opportunities for an Old Dilemma. Front Cardiovasc Med. 8:805727.
Publisher | Google Scholor - Patel P, Shrivastava R, Patel R, Warghane P. (2023). Coronary Artery Ectasia. Indian Journal of Clinical Cardiology. 4(1):30-38.
Publisher | Google Scholor