Case Report
Beyond Borders: Exploring the Uncharted Territory of Breast Metastasis in Meningioma
1Senior Resident, Dept. of Histopathology, Sir Gangaram Hospital, New Delhi, India.
2Senior Consultant, Neurosurgery, Sir Gangaram Hospital, New Delhi, India.
3Senior Consultant and Chairperson, Dept. of Histopathology, Sir Gangaram Hospital, New Delhi, India.
4Senior Consultant, Dept. of Histopathology, Sir Gangaram Hospital, New Delhi, India.
*Corresponding Author: Seema Rao, Senior Consultant, Dept. of Histopathology, Sir Gangaram Hospital, New Delhi, India.
Citation: Kapoor R, Goyal A, Badwal S, Rao S. (2024). Beyond Borders: Exploring the Uncharted Territory of Breast Metastasis in Meningioma, International Journal of Clinical and Surgical Pathology, BioRes Scientia Publishers. 1(2):1-3. DOI: 10.59657/ijcsp.brs.24.008
Copyright: © 2024 Seema Rao, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 19, 2024 | Accepted: August 23, 2024 | Published: August 30, 2024
Abstract
Keywords:
Introduction
A donor neoplasm's hematogenous spread within a primary host tumor is known as tumor-to-tumor metastasis (TTM) [1]. Though its exact pathophysiology is still unknown, TTM has been documented in the literature for nearly a century, since the first description by Fried in 1930 [2]. According to the literature, lung cancer and breast cancer are the most common donor tumors in TTM [3,4]. Here, we present our experience with a case of TTM of breast cancer to meningioma.
Case Presentation
A 77-year-old female patient, known hypertensive, presented with insidious onset and gradually progressive diminished vision in left eye resulting complete loss of vision over a span of 10 days. Patient also had history of appetite loss and weight loss for 1 month with no history of seizures/vomiting/loss of consciousness.
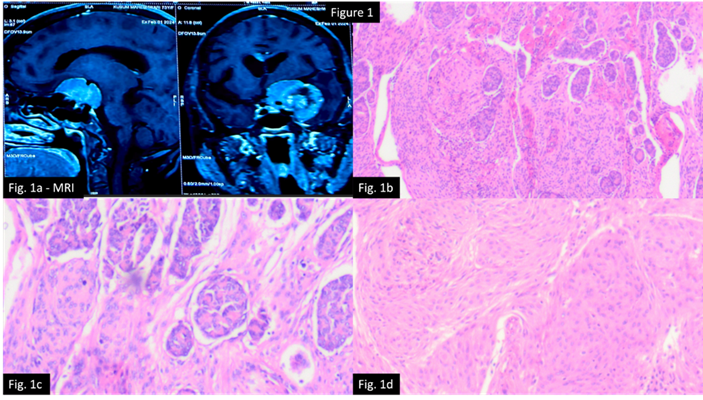
On MRI brain, a left Spheno-cavernous extra-axial space occupying lesion was seen with edema and mass effect suggestive of meningioma (Figure 1a). Excision of the tumor mass was done and sent for histopathological examination which revealed a relatively circumscribed nodular meningeal tumor which was extensively infiltrated and effaced by an adenocarcinoma in tubules and nests (Figure 1b and 1c). Periphery showed nests/lobules of appreciable meningothelial tumor component with syncytial arrangement and occasional psammoma bodies (Figure 1d).
Figure 1: 1(a): MRI image showing left Spheno-cavernous extra-axial space occupying enhancing lesion.1(b): H&E (low power): nodular meningeal tumor infiltrated by an adenocarcinoma arranged in cords, trabeculae, nests, tubules, and clusters. 1(c): H&E (medium power) Adenocarcinoma cells are round to ovoid with vesicular nuclei, inconspicuous nucleoli, and moderate eosinophilic cytoplasm along with scattered mitosis. 1(d): H&E (medium power) Meningeal tumor cells are monomorphic, round cells with vesicular nuclei and indistinct cytoplasmic boundaries; mitotic activity is scant in this component.
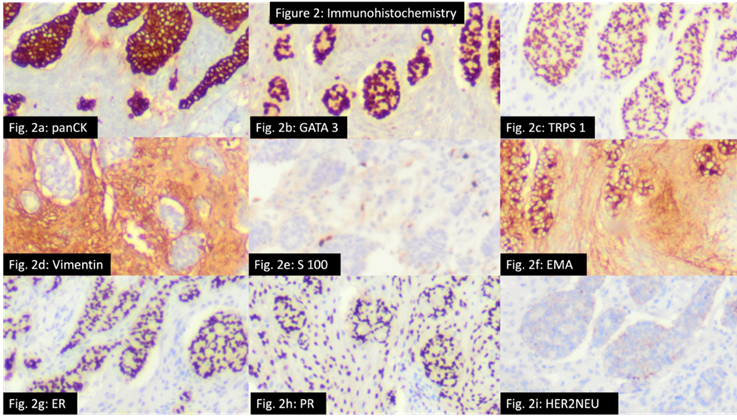
On IHC analysis (Figure 2), Adenocarcinoma component was positive for panCK, CK7, EMA, GATA3, TRPS1, ER (>90%; strong intensity) and PR (>90%; strong intensity) while being negative for TTF1, CK20, S100 and Her2neu (score 0). This immunopurified favored a breast primary tumor. On taking deep history, patient was an operated case of breast cancer (25 years back).
Figure 2: Immunohistochemistry (IHC) analysis. Figure 2a-2c: Donor tumor shows positivity for panCK, GATA 3 and TRPS 1. Figure 2d-2f: Recipient tumor shows positivity for vimentin, S-100 and EMA. Figure 2g-2i: Breast cancer panel showing ER and PR positivity while Her2neu negativity.
Meningioma component was positive for Vimentin, S100(focal), EMA and PR while negative for others.
Ki67 index is Lessthan5Percentage in Adenocarcinoma component and Lessthan1Percentage in meningioma component.
Patient was advised for follow up PET-CT and radiotherapy was planned.
TTM refers to tumor cells that metastasize via the blood to a primary host tumor (recipient tumor) from a donor tumor [4]. TTM is a known phenomenon. Over 70Percentage cases involved meningiomas, of which nearly half showed breast cancer metastasis [5]. According to Paget's "soil and seed" theory, meningiomas are susceptible to becoming recipient tumors because of their high collagen and lipid content, which creates an optimal environment for implantation [6]. Campbell et al. laid down the criteria (Box 1) for TTM which is fulfilled in our case [7].
| BOX 1 |
| Proposed diagnostic criteria by Campbell et al, [7]. |
| 1. At least two primary tumors must exist. |
| 2. The host tumor must be a true neoplasm. |
| 3. The metastatic focus must show established growth inside of the host tumor, must not be the result of contiguous growth. |
| 4. The host tumor cannot be a lymph node involved by leukemia or lymphoma. |
Conclusion
We present a rare case of TTM of breast cancer into a meningioma, which was treated using surgical resection. In the context of a meningioma, it is crucial to consider the potential for TTM in a patient with a systemic cancer. Further research is necessary to determine an appropriate course of treatment and prognosis for this uncommon occurrence, as the clinical significance of TTM is still unknown.
Declarations
Acknowledgement
None.
Conflict of Interest
None Declared.
Funding Sources
None.
Data Availability Statement
The data will be available on request from the corresponding author Informed Consent and Ethics Statement: Adequate informed consent has been taken from the patient and this manuscript has been approved by the institutional review board.
References
- Moody P, Murtagh K, Piduru S, Brem S, Murtagh R, et al. (2012). Tumor-to-Tumor Metastasis: Pathology and Neuro Imaging Considerations. Int J Clin Exp Pathol. 5:367-373.
Publisher | Google Scholor - Fried BM. (1930). Inoculation of a Meningioma by Cancer Cells from A Branchiogenic Carcinoma. Am J Pathol. 6:47-52.
Publisher | Google Scholor - Turner N, Kaye AH, Paldor I. (2021). Metastases To Meningioma-Review and Meta-Analysis. Acta Neurochir (Wien). 163:699-709.
Publisher | Google Scholor - Papadakis BK, Vorrias E, Bräutigam K, Chochlidakis N, Koutsopoulos A, et al. (2021). Intrameningioma Metastasis: A Case-Based Literature Review. J Clin Neurosci. 93:168-173.
Publisher | Google Scholor - Syed S, Karambizi DI, Baker A, et al. (2018). A Comparative Report on Intracranial Tumor to Tumor Metastasis and Collision Tumors. World Neurosurg. 116:454-463.e2.
Publisher | Google Scholor - Lanotte M, Benech F, Panciani PP, Cassoni P, Ducati A. (2009). Systemic Cancer Metastasis in A Meningioma: Report of Two Cases and Review of The Literature. Clin Neurol Neurosurg. 111:87-93.
Publisher | Google Scholor - Campbell LV Jr, Gilbert E, Chamberlain CR Jr, Watne AL. (1968). Metastases of Cancer to Cancer. Cancer. 22:635-643.
Publisher | Google Scholor