Research Article
Awareness and Prevalence of Cervical Cancer among Women of Reproductive Age in Southeast, Nigeria
- S. N. Ikegwuonu 1
- E. O. Ewenyi 2
- I. A. Onuah 3
- F. C. Alumona 4
- I. O. Abali 5
- E. O. Ezirim 6
- E. M. Akwuruoha 6
- C. O. Onyemereze 6
- O. O. Adesina 7
- A. I. Airaodion 8*
1 Medical Laboratory Scientist, Nosmaris Medical Diagnostics Ltd, Aguda, Surulere, Lagos, Nigeria.
2 School of Public Health, University of Port Harcourt, Rivers, Nigeria.
3Department of Surgery, University of Port Harcourt Teaching Hospital, Rivers, Nigeria.
4 Department of Obstetrics and Gynaecology, University of Port Harcourt Teaching Hospital, Rivers State, Nigeria.
5Department of Surgery, Abia State University, Uturu, Nigeria.
6Department of Obstetrics and Gynaecology, Abia State University, Uturu, Nigeria.
7Department of Medical Laboratory Science, Babcock University, Ilishan. Ogun State, Nigeria.
8 Department of Biochemistry, Lead City University, Ibadan, Oyo, Nigeria.
*Corresponding Author: A. I. Airaodion, Department of Biochemistry, Lead City University, Ibadan, Oyo, Nigeria.
Citation: Ikegwuonu S. N, Ewenyi E. O, Onuah I. A, Alumona F. C, Airaodion A. I, et al. (2024). Awareness and Prevalence of Cervical Cancer among Women of Reproductive Age in Southeast, Nigeria. Journal of Cancer Management and Research, BioRes Scientia Publishers. 2(2):1-12. DOI: 10.59657/2996-4563.brs.24.016
Copyright: © 2024 A. I. Airaodion, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 15, 2024 | Accepted: August 27, 2024 | Published: August 31, 2024
Abstract
Background: Cervical cancer is a significant public health concern in Nigeria, with a high burden of morbidity and mortality. The awareness of cervical cancer and its preventive measures, including screening, is essential for reducing the disease's prevalence. This study aimed to assess the level of awareness and prevalence of cervical cancer among women of reproductive age in Southeast Nigeria.
Methods: A cross-sectional descriptive study was conducted among 235 women aged 15-49 years in Southeast Nigeria, using a multistage sampling technique. Data were collected using a structured questionnaire and analyzed using SPSS version 26. Descriptive statistics were used to summarize the data, and chi-square tests were applied to assess associations between demographic variables and cervical cancer prevalence.
Results: The study found that 41.7% of the participants had heard of cervical cancer, while only 30.21% were aware of the Pap smear test. The prevalence of cervical cancer in the study population was 13.19%. Factors such as age, education level, marital status, and residence significantly influenced the prevalence of cervical cancer (p < 0.05).
Conclusion: Awareness of cervical cancer and its prevention is relatively low among women in Southeast Nigeria, contributing to the observed prevalence. Efforts to increase awareness through education and improve access to screening services are crucial in reducing the burden of cervical cancer in the region.
Keywords: cervical cancer; awareness; prevalence; women of reproductive age
Introduction
Cervical cancer remains one of the most significant public health challenges affecting women globally, particularly in low- and middle-income countries (LMICs). Despite advancements in screening and vaccination, the incidence and mortality rates of cervical cancer remain disproportionately high in sub-Saharan Africa, including Nigeria. This disparity is largely attributed to limited awareness, inadequate access to preventive measures, and socio-cultural factors that hinder early detection and treatment. Globally, cervical cancer is the fourth most common cancer among women, with an estimated 604,000 new cases and 342,000 deaths in 2020 [1]. The majority of these cases occur in LMICs, where health systems often struggle with limited resources, weak infrastructure, and competing health priorities. Sub-Saharan Africa accounts for a significant burden of this disease, with cervical cancer being the leading cause of cancer-related deaths among women in this region [2]. In Nigeria, cervical cancer is the second most common cancer among women, following breast cancer. Nigeria recorded an estimated 12,075 new cases and 7,968 deaths due to cervical cancer in 2020 [3]. These figures highlight the urgent need for effective public health interventions to address the growing burden of cervical cancer in the country.
The high prevalence of cervical cancer in Nigeria can be attributed to a combination of epidemiological and socio-cultural factors. The primary etiological factor for cervical cancer is persistent infection with high-risk types of human papillomavirus (HPV), particularly HPV-16 and HPV-18, which are responsible for approximately 70% of cervical cancer cases worldwide [4]. In Nigeria, the prevalence of HPV among women is estimated to be high, with significant variations across different regions [5]. Other risk factors for cervical cancer include early onset of sexual activity, multiple sexual partners, high parity, smoking, and long-term use of oral contraceptives. Socioeconomic factors, such as poverty, low educational attainment, and limited access to healthcare services, further exacerbate the risk of cervical cancer among Nigerian women [6]. Awareness and knowledge of cervical cancer play a crucial role in the prevention and early detection of the disease. Studies have shown that women with adequate knowledge of cervical cancer and its risk factors are more likely to participate in screening programs and adopt preventive measures, such as HPV vaccination [7]. However, in Nigeria, awareness of cervical cancer remains suboptimal, particularly among women of reproductive age.
Cervical cancer is a preventable disease, primarily through early detection and treatment of precancerous lesions. The two main strategies for cervical cancer prevention are HPV vaccination and regular screening through Pap smears or HPV testing. Despite the availability of these preventive measures, cervical cancer screening rates in Nigeria remain low, with significant disparities across different regions and socio-economic groups [8]. In Southeast Nigeria, cultural beliefs, fear of stigma, and misconceptions about cervical cancer screening are significant barriers to the uptake of screening services. Additionally, the lack of infrastructure and trained healthcare providers further limits access to screening, particularly in rural areas. As a result, many women present with advanced stages of cervical cancer, leading to poor prognosis and high mortality rates [9]. Given the high burden of cervical cancer and the low levels of awareness and screening in Nigeria, there is a critical need for research to understand the factors influencing awareness and the prevalence of cervical cancer among women of reproductive age in Southeast Nigeria. This region, with its unique socio-cultural and economic characteristics, presents a valuable context for examining the challenges and opportunities for improving cervical cancer prevention and control. The findings from this study will contribute to the existing body of knowledge on cervical cancer in Nigeria and inform the development of targeted interventions to increase awareness, improve screening rates, and ultimately reduce the burden of cervical cancer among women in Southeast Nigeria.
Research Methodology
Study Design
This research employed a cross-sectional descriptive study design to assess the awareness and prevalence of cervical cancer among women of reproductive age in Southeast Nigeria. The study focused on understanding the level of awareness and the prevalence of cervical cancer in this population. The cross-sectional design is appropriate for determining the prevalence of particular attributes and allows for the collection of data from a large population in a relatively short period [10].
Study Area
Southeast Nigeria, comprising Abia, Anambra, Ebonyi, Enugu, and Imo states, is an important region for studying the awareness and prevalence of cervical cancer among women of reproductive age. This region is predominantly inhabited by the Igbo ethnic group and is characterized by a mix of urban and rural communities, with varying levels of access to healthcare services. Cultural beliefs, educational attainment, and economic status differ across these states, potentially influencing health-seeking behaviours and awareness of cervical cancer. The region's healthcare infrastructure and the availability of screening services, such as Pap smears, also vary, making it a critical area for understanding the disparities in cervical cancer awareness and prevalence. By focusing on Southeast Nigeria, the study can provide insights into regional differences in cervical cancer knowledge, attitudes, and practices, which are essential for targeted interventions and policy-making.
Study Population
The target population was women of reproductive age, defined as women aged 15-49 years, residing in Southeast Nigeria. This demographic is particularly relevant due to their susceptibility to cervical cancer and the need for regular screening.
Sample Size Determination
The sample size was determined using the Cochran formula for estimating proportions in a population outlined by Airaodion et al. [11]:

where n = minimum sample size
Z = 1.96 at 95% confidence level,
P = known prevalence of cervical cancer in Nigeria
e = error margin tolerated at 5% = 0.05
q = 1 - p
According to Omosun et al. [12], the existing prevalence of cervical cancer in Nigeria is 16.4%.
P = 16.4% = 0.164
q = 1 – p
= 1 – 0.164
= 0.836


 = 210.68
= 210.68
The minimum sample size was 211 and was adjusted to 235 to account for a non-response rate of 10 %.
Sampling Technique
A multistage sampling technique was employed to select participants. This includes:
- Selection of States: All five (Abia, Anambra, Ebonyi, Enugu, and Imo) states in Southeast Nigeria were included in the study to ensure a comprehensive regional representation.
- Selection of Local Government Areas (LGAs): From each state, three LGAs were randomly selected.
- Selection of Communities: In each selected LGA, two communities (one rural and one urban) were randomly chosen.
- Selection of Participants: From each community, women of reproductive age were selected using systematic random sampling from households. The sampling frame consisted of a list of households within each community, and every 3rd household was chosen until the desired sample size was achieved.
Inclusion and Exclusion Criteria
Inclusion Criteria:
- Women aged 15-49 years who have resided in the study area for at least one year.
- Women who give informed consent to participate in the study.
Exclusion Criteria:
- Women with a known history of cervical cancer, as they may have higher awareness than the general population.
- Women who are healthcare professionals or are working in a related field, as their awareness levels might differ significantly.
- Women who did not give informed consent to participate in the study
Data Collection Instruments
Data was collected using a structured questionnaire, which was divided into three sections:
- Demographic Information: Age, marital status, education level, occupation, and other relevant socio-demographic factors.
- Awareness of Cervical Cancer: Questions assessed the respondents' knowledge of cervical cancer, symptoms, screening methods (e.g., Pap smear, HPV test) etc.
- Prevalence of Cervical Cancer: Self-reported history of cervical cancer diagnosis and treatment were recorded.
The questionnaire was pre-tested in a pilot study to ensure its reliability and validity.
Data Collection Procedure
Trained research assistants administered the questionnaires through face-to-face interviews to ensure clarity and accuracy. The interviews were conducted in the local language (Igbo) where necessary, and translations were provided to maintain consistency.
Clinical Screening: Participants were offered cervical cancer screening through Pap smear test. This was done to assess the prevalence of cervical cancer in the study population.
Data Analysis
Quantitative data was analyzed using Statistical Package for Social Sciences (SPSS) software version 26. Descriptive statistics (frequencies, and percentages) were used to summarize the data. Chi-square tests were employed to assess associations between demographic variables and the prevalence of cervical cancer. A p-value of less than 0.05 was considered statistically significant.
Results
The study sample consisted of 235 women, with the majority (59.57%) aged between 30 and 49 years. Specifically, 24.68% were aged 30-34 years, 15.32% were 35-39 years, 16.60% were 40-44 years, and 20.00% were 45-49 years. In terms of education, a significant portion (57.45%) had secondary education, while 20.00% had tertiary education. Most of the participants were married (55.32%) and resided in urban areas (51.06%). Employment status varied, with 32.77% self-employed and 21.70% employed in the public sector. Monthly income data revealed that 44.26 percentage earned between 50,001 - 100,000 Naira, while 23.40 percentage earned between 10,001 - 50,000 Naira. The majority had 1-2 children (50.21%), with only 4.68 percentage having five or more children (Table 1). The study found that 58.30 percentage of the participants had never heard of cervical cancer, indicating a significant gap in awareness. Among those aware, healthcare providers (21.22%) and the internet/social media (36.33%) were the primary sources of information. A large proportion of respondents identified Human Papillomavirus (HPV) (24.37%) and multiple sexual partners (23.53%) as the causes of cervical cancer. However, awareness of HPV itself was low, with only 39.57 percentage having heard of it, and among those, only 46.24 percentage knew about the HPV vaccine. Similarly, only 30.21 percentage had heard of the Pap smear test, with 80.28 percentage of those knowing its purpose. Despite these gaps in knowledge, 41.70 percentage believed cervical cancer could be prevented, primarily through regular screening (30.52%) and safe sexual practices (28.51%) (Table 2).
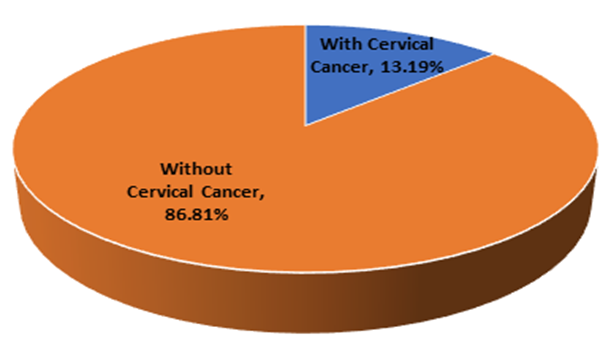
The prevalence of cervical cancer in the study population was 13.19 percentage, with 31 out of 235 women diagnosed using the Pap smear test. The remaining 86.81 percentage were not found to have cervical cancer (Figure 1). Regarding family history and personal experiences with cervical cancer, only 14.89 percentage of participants knew someone diagnosed with the disease, with 31.43 percentage of these cases being family members. Notably, none of the participants had been diagnosed with cervical cancer themselves or experienced symptoms that raised concerns about the disease. A small percentage (4.68%) reported having a family history of cervical cancer (Table 3). Several factors were found to significantly influence the prevalence of cervical cancer. Age was a critical factor, with higher prevalence observed in older age groups, particularly those aged 45-49 years (36.17%). Educational level also played a role, with no cases found among those with tertiary education (p = 0.038). Marital status was another significant factor, with a higher prevalence among divorced/widowed women (27.59%) compared to married women (6.15%). The residence was important as well, with rural dwellers experiencing a higher prevalence (16.52%) than urban dwellers (10.00%) (p = 0.049). Additionally, women who had more children (5 or more) had a significantly higher prevalence (54.55%) compared to those with fewer or no children (p = 0.019). Awareness of cervical cancer and related health practices, such as knowledge of HPV and Pap smear tests, were associated with lower prevalence rates, underscoring the importance of awareness in prevention (Table 4).
Table 1: Socio-Demographic Information of Participants
| Socio-Demographic Information | Frequency (n = 235) | Percentage (%) |
| Age (in Years) | ||
| 15-24 | 21 | 8.94 |
| 25-29 | 34 | 14.47 |
| 30-34 | 58 | 24.68 |
| 35-39 | 36 | 15.32 |
| 40-44 | 39 | 16.60 |
| 45-49 | 47 | 20.00 |
| Educational Level | ||
| No formal Education | 19 | 8.09 |
| Primary Education | 34 | 14.47 |
| Secondary Education | 135 | 57.45 |
| Tertiary Education | 47 | 20.00 |
| Marital Status | ||
| Single | 47 | 20.00 |
| Married | 130 | 55.32 |
| Divorced/Widowed | 58 | 24.68 |
| Employment Status | ||
| Unemployed | 21 | 8.94 |
| Self-employed | 77 | 32.77 |
| Private sector employee | 48 | 20.43 |
| Public sector employee | 51 | 21.70 |
| Student | 38 | 16.17 |
| Residence | ||
| Rural | 115 | 48.94 |
| Urban | 120 | 51.06 |
| Monthly Income (Naira) | ||
| Below 10,000 | 00 | 0.00 |
| 10,001 - 50,000 | 55 | 23.40 |
| 50,001 - 100,000 | 104 | 44.26 |
| 100,001 - 150,000 | 54 | 22.98 |
| Above 150,000 | 22 | 9.36 |
| Number of Children | ||
| 0 | 33 | 14.04 |
| 1-2 | 118 | 50.21 |
| 3-4 | 73 | 31.06 |
| 5 or more | 11 | 4.68 |
Table 2: Awareness of Cervical Cancer in Southeast, Nigeria.
| Variable | Frequency (n = 235) | Percentage (%) |
| Have you ever heard of cervical cancer? | ||
| Yes | 98 | 41.70 |
| No | 137 | 58.30 |
| *If yes, where did you hear about cervical cancer? (You may select more than one) (n = 245) | ||
| Family/friends | 14 | 5.71 |
| Healthcare provider | 52 | 21.22 |
| Media (TV, radio, newspapers) | 22 | 8.97 |
| Internet/social media | 89 | 36.33 |
| School/educational institution | 31 | 12.65 |
| Religious gatherings | 29 | 11.84 |
| Community outreach programs | 08 | 3.27 |
| What do you think are the causes of cervical cancer? (You may select more than one) (n = 357) | ||
| Human Papillomavirus (HPV) | 87 | 24.37 |
| Multiple sexual partners | 84 | 23.53 |
| Early sexual activity | 65 | 18.21 |
| Smoking | 31 | 8.68 |
| Poor hygiene | 45 | 12.61 |
| Genetic factors | 33 | 9.24 |
| Others | 12 | 3.36 |
| Have you heard of the Human Papillomavirus (HPV)? | ||
| Yes | 93 | 39.57 |
| No | 44 | 18.72 |
| Not sure | 98 | 41.70 |
| If yes, do you know that there is a vaccine for preventing HPV infection? | ||
| Yes | 43 | 46.24 |
| No | 50 | 53.76 |
| Have you heard of the Pap smear test? | ||
| Yes | 71 | 30.21 |
| No | 75 | 31.91 |
| Not sure | 89 | 37.87 |
| If yes, do you know what the Pap smear test is used for? | ||
| Yes | 57 | 80.28 |
| No | 14 | 19.71 |
| *What are the symptoms of cervical cancer that you are aware of? (You may select more than one) (n = 470) | ||
| Abnormal vaginal bleeding | 126 | 26.81 |
| Pain during intercourse | 83 | 17.66 |
| Pelvic pain | 101 | 21.49 |
| Unusual vaginal discharge | 142 | 30.21 |
| Others | 18 | 3.83 |
| Can cervical cancer be prevented? | ||
| Yes | 98 | 41.70 |
| No | 26 | 11.06 |
| Not sure | 111 | 47.23 |
| *If yes, how can it be prevented? (You may select more than one) (n = 249) | ||
| Regular screening (Pap smear) | 76 | 30.52 |
| HPV vaccination | 55 | 22.09 |
| Safe sexual practices | 71 | 28.51 |
| Avoiding smoking | 36 | 14.46 |
| Others | 11 | 4.42 |
| *What role do you think the government should play in increasing cervical cancer awareness and screening? (Select all that apply) (n = 813) | ||
| Implement nationwide awareness campaigns | 211 | 25.95 |
| Provide free or subsidized screening services | 98 | 12.05 |
| Mandate HPV vaccination for young girls | 185 | 22.76 |
| Train more healthcare professionals in cancer screening | 200 | 24.60 |
| Partner with NGOs and community organizations | 78 | 9.59 |
| Other | 41 | 5.04 |
* Indicates multiple response
Figure 1: Prevalence of Cervical Cancer in the Study Population
Table 3: Prevalence and Family History of Participants
| Variable | Frequency (n = 235) | Percentage (%) |
| Do you know anyone who has been diagnosed with cervical cancer? | ||
| Yes | 35 | 14.89 |
| No | 200 | 85.11 |
| If yes, what is your relationship with the person? | ||
| Family member | 11 | 31.43 |
| Friend | 9 | 25.71 |
| Neighbour | 7 | 20.00 |
| Colleague | 4 | 11.43 |
| Others | 4 | 11.43 |
| Have you ever been diagnosed with cervical cancer? | ||
| Yes | 00 | 0.00 |
| No | 235 | 100.00 |
| Have you experienced any symptoms that you were concerned might be related to cervical cancer? (e.g., abnormal bleeding, pain, etc.) | ||
| Yes | 00 | 0.00 |
| No | 235 | 100.00 |
| Do you have any family history of cervical cancer? | ||
| Yes | 11 | 4.68 |
| No | 188 | 80.00 |
| Not sure | 36 | 15.32 |
Table 4: Factors influencing the Prevalence of Cervical Cancer in Southeast, Nigeria
| Variable | Prevalence of Cervical Cancer | p-value | |
| With Cervical Cancer (n = 31) | Without Cervical Cancer (n = 204) | ||
| Age (in Years) | 0.001* | ||
| 15-24 | 00 (0.00%) | 21 (100.00%) | |
| 25-29 | 00 (0.00%) | 34 (100.00%) | |
| 30-34 | 00 (0.00%) | 58 (100.00%) | |
| 35-39 | 04 (11.11%) | 32 (88.89%) | |
| 40-44 | 10 (25.64%) | 29 (74.36%) | |
| 45-49 | 17 (36.17%) | 30 (63.83%) | |
| Educational Level | 0.038* | ||
| No formal Education | 6 (31.58%) | 13 (68.42%) | |
| Primary Education | 12 (35.29%) | 22 (64.71%) | |
| Secondary Education | 13 (9.63%) | 122 (90.37%) | |
| Tertiary Education | 00 (0.00%) | 47 (100.00%) | |
| Marital Status | 0.011* | ||
| Single | 7 (14.89%) | 40 (85.11%) | |
| Married | 8 (6.15%) | 122 (93.85%) | |
| Divorced/Widowed | 16 (27.59%) | 42 (72.41%) | |
| Employment Status | 0.210 | ||
| Unemployed | 3 (14.29%) | 18 (85.71%) | |
| Self-employed | 9 (11.69%) | 68 (88.31%) | |
| Private sector employee | 7 (14.58%) | 41 (85.42%) | |
| Public sector employee | 11 (21.57%) | 40 (78.43%) | |
| Student | 1 (2.63%) | 37 (97.37%) | |
| Residence | 0.049* | ||
| Rural | 19 (16.52%) | 96 (83.48%) | |
| Urban | 12 (10.00%) | 108 (90.00%) | |
| Monthly Income (Naira) | 0.614 | ||
| Below 10,000 | 00 (0.00%) | 00 (0.00%) | |
| 10,001 - 50,000 | 8 (14.55%) | 47 (85.45%) | |
| 50,001 - 100,000 | 10 (9.62%) | 94 (90.38%) | |
| 100,001 - 150,000 | 10 (18.52%) | 44 (81.48%) | |
| Above 150,000 | 3 (13.64%) | 19 (86.36%) | |
| Number of Children | 0.019* | ||
| 0 | 00 (0.00%) | 33 (100.00%) | |
| 1-2 | 17 (14.41%) | 101 (85.59%) | |
| 3-4 | 8 (10.95%) | 65 (89.04%) | |
| 5 or more | 6 (54.55%) | 5 (45.45%) | |
| Have you ever heard of cervical cancer? | 0.000* | ||
| Yes | 5 (5.10%) | 93 (94.90%) | |
| No | 26 (18.98%) | 111 (81.02%) | |
| Have you heard of the Human Papillomavirus (HPV)? | 0.006* | ||
| Yes | 4 (4.30%) | 89 (95.70%) | |
| No | 10 (22.73%) | 34 (77.27%) | |
| Not sure | 17 (17.35%) | 81 (82.65%) | |
| Have you heard of the Pap smear test? | 0.003* | ||
| Yes | 3 (4.22%) | 68 (95.77%) | |
| No | 15 (20.00%) | 60 (80.00%) | |
| Not sure | 13 (14.61%) | 76 (85.39%) | |
| Can cervical cancer be prevented? | 0.001* | ||
| Yes | 5 (5.10%) | 93 (94.90%) | |
| No | 6 (23.08%) | 20 (76.92%) | |
| Not sure | 20 (18.02%) | 91 (81.98%) | |
| Do you know anyone who has been diagnosed with cervical cancer? | 0.035* | ||
| Yes | 5 (14.29%) | 30 (85.71%) | |
| No | 26 (13.00%) | 174 (87.00%) | |
| Do you have any family history of cervical cancer? | 0.000* | ||
| Yes | 9 (81.82%) | 2 (18.18%) | |
| No | 6 (3.19%) | 182 (96.81%) | |
| Not sure | 16 (44.44%) | 20 (55.56%) | |
Discussion
The findings from this study indicate that awareness of cervical cancer among women of reproductive age in Southeast Nigeria remains suboptimal. Only 41.7% of respondents have heard of cervical cancer, a figure that is lower than what has been reported in similar studies conducted in other regions of Nigeria. For instance, a study conducted in Southwest Nigeria reported awareness levels as high as 65% among women of reproductive age [13]. This discrepancy might be attributed to differences in educational levels, accessibility to healthcare information, and the effectiveness of public health campaigns across regions. The sources of information for those who were aware of cervical cancer were diverse. The internet and social media were the most significant sources, accounting for 36.33% of awareness. This finding underscores the growing influence of digital platforms in disseminating health information. In contrast, healthcare providers were the source for 21.22% of the respondents, which is concerning given the critical role that healthcare professionals play in educating the public about serious health conditions such as cervical cancer. Previous studies have also highlighted the importance of healthcare providers in raising awareness, suggesting that more needs to be done to utilize this channel effectively [14].
The study revealed a fragmented understanding of the causes of cervical cancer among respondents. While 24.37% correctly identified Human Papillomavirus (HPV) as a cause, significant proportions of women also incorrectly associated cervical cancer with factors like poor hygiene (12.61%) and genetic factors (9.24%). These misconceptions may contribute to inadequate preventive behaviors and highlight the need for targeted educational campaigns to correct these misunderstandings. Previous studies have similarly noted confusion among women regarding the etiology of cervical cancer, particularly in regions with low literacy levels and limited access to accurate health information [15]. Regarding prevention, 41.7% of respondents believed that cervical cancer could be prevented, but there was limited knowledge about effective preventive measures. Regular screening (Pap smear) was recognized by 30.52% of respondents, and HPV vaccination was identified by 22.09%. These findings align with other studies in Nigeria that have shown a low level of knowledge about cervical cancer prevention, despite the availability of effective interventions like HPV vaccination and Pap smear tests [16].
Awareness of HPV, the primary cause of cervical cancer, was relatively low, with only 39.57% of respondents having heard of it. Even among those who had heard of HPV, awareness of the HPV vaccine was limited, with only 46.24 percentage being aware of its existence. This is consistent with previous research in Nigeria, where HPV awareness remains low despite efforts to introduce the HPV vaccine into national immunization programs [17]. The low awareness of the Pap smear test (30.21%) further underscores the need for intensified public health efforts to promote cervical cancer screening. The study also explored awareness of cervical cancer symptoms, with abnormal vaginal bleeding (26.81%) and unusual vaginal discharge (30.21%) being the most commonly recognized symptoms. However, a significant proportion of women were unaware of other critical symptoms, such as pelvic pain and pain during intercourse. This incomplete understanding of cervical cancer symptoms is consistent with findings from other studies in Nigeria, where symptom awareness is often limited to the more obvious signs, potentially leading to delayed diagnosis and treatment [18].
The respondents expressed strong opinions regarding the role of the government in increasing cervical cancer awareness and screening. The majority (25.95%) believed that the government should implement nationwide awareness campaigns, while 24.60 percentage supported the idea of training more healthcare professionals in cancer screening. These findings are in line with previous research that emphasizes the importance of government-led initiatives in improving cervical cancer outcomes [19]. Additionally, 22.76% of respondents advocated for mandatory HPV vaccination for young girls, reflecting a growing recognition of vaccination as a key preventive measure. The awareness level reported in this study is lower than what has been observed in other regions of Nigeria, such as Lagos, where awareness levels were reported to be over 60% [14]. The reliance on the internet and social media as primary sources of information is consistent with global trends, where digital platforms are increasingly becoming critical sources of health information, especially among younger populations [20]. However, the low awareness of HPV and the Pap smear test is a recurrent issue in many parts of Nigeria, as highlighted by Adebamowo et al. [17]. This suggests that despite ongoing efforts, significant barriers to effective cervical cancer education and screening remain. Misconceptions about the causes of cervical cancer, such as the belief in poor hygiene as a causative factor, also mirror findings from other low-resource settings, where myths and misinformation often prevail due to a lack of accurate health education [15].
The prevalence of cervical cancer in the study population was determined using Pap smear results, revealing that 13.19 percentage of the participants (31 out of 235) were diagnosed with cervical cancer, while the remaining 86.81% (204 out of 235) were not (Figure 1). This prevalence rate is noteworthy, especially when considering that cervical cancer is one of the most preventable and treatable forms of cancer if detected early through regular screening programs.
Compared to previous studies, the prevalence rate observed in this study is relatively higher. For instance, a study earlier conducted in Enugu, a state in Southeast Nigeria, reported a prevalence rate of 9.5 percentage among women attending gynecological clinics [21]. Another study in Lagos, Southwest Nigeria, found a lower prevalence rate of 7.1 percentage among women who had never undergone screening [22]. Additionally, the higher awareness of cervical cancer reported in this study compared to the findings of Owoeye and Ibrahim [23], who found that only 10% of women in Ilorin, Northcentral Nigeria, were aware of cervical cancer, indicates that awareness campaigns in Southeast Nigeria may have been more effective. The higher prevalence observed in this study may be attributed to the specific demographic characteristics of the study population, which consisted of women of reproductive age, a group potentially at higher risk for cervical cancer.
The awareness of cervical cancer within the study population was also assessed. A significant portion of the participants (14.89%) knew someone who had been diagnosed with cervical cancer, which highlights a moderate level of awareness within the community. Among those who knew someone with cervical cancer, 31.43 percentage identified the individual as a family member, which is an important finding, considering the hereditary nature of certain cancers, including cervical cancer [24]. However, despite this awareness, none of the participants reported having been diagnosed with cervical cancer themselves, nor did any report experiencing symptoms that might be related to the disease. This may suggest a gap between awareness and personal concern or recognition of symptoms, which could be a barrier to seeking preventive care. The low percentage of participants with a family history of cervical cancer (4.68%) is consistent with findings from previous research. A study conducted in Ibadan, Nigeria, reported a similar percentage of participants with a family history of the disease (4.2%) [32]. This suggests that while family history is an important risk factor, it may not be prevalent in the general population, and therefore, public health interventions should focus more on general awareness and screening rather than just targeting those with a family history.
Furthermore, the absence of participants reporting personal diagnoses of cervical cancer or related symptoms could be contrasted with findings from studies in other regions, where women often reported symptoms but did not seek medical help due to various barriers, including fear, stigma, and lack of access to healthcare services [25]. This suggests that while awareness might be increasing, there is still a need for education on the importance of recognizing symptoms and seeking timely medical intervention.
The study reveals a notable prevalence of cervical cancer among women of reproductive age in Southeast Nigeria, particularly concentrated in older age groups. The prevalence was highest among women aged 45-49 years, where 36.17 percentage were diagnosed with cervical cancer, followed by those aged 40-44 years with a prevalence of 25.64%. This aligns with global trends indicating that cervical cancer risk increases with age, particularly after 35 years, reflecting cumulative exposure to risk factors over time [26]. The prevalence of cervical cancer was also significantly associated with educational level, marital status, residence, and several awareness-related variables. Women with lower educational attainment, especially those without formal education (31.58%) and those with only primary education (35.29%), showed higher prevalence rates compared to those with secondary (9.63%) and tertiary education (0.00%). This underscores the critical role of education in health awareness and access to preventive measures. Women with higher education are more likely to be informed about cervical cancer screening and preventive practices, reducing their risk of developing the disease [27]. Marital status was another significant factor, with divorced or widowed women showing a higher prevalence (27.59%) compared to married (6.15%) and single women (14.89%). The increased risk among divorced or widowed women could be due to factors such as lower socioeconomic status, reduced access to healthcare, and potentially higher exposure to multiple sexual partners, which is a known risk factor for human papillomavirus (HPV) infection, the primary cause of cervical cancer [28].
The residence also influenced the prevalence, with rural women (16.52%) more affected than their urban counterparts (10.00%). This is consistent with studies showing that rural populations often have less access to healthcare services, including cancer screening programs, and may have lower health literacy levels [29]. The disparity in healthcare access between urban and rural areas remains a significant barrier to reducing cervical cancer incidence in developing regions.
The awareness of cervical cancer and its prevention was critically low among the participants, particularly among those diagnosed with the disease. Only 5.10 percentage of those who had heard of cervical cancer were diagnosed with it, compared to 18.98 percentage who had never heard of it. Similarly, a significant proportion of women who had never heard of HPV (22.73%) and were not aware of the Pap smear test (20.00%) were more likely to have cervical cancer. These findings highlight a critical gap in public health education, particularly concerning the role of HPV in cervical cancer development and the importance of regular screening through Pap smears [30]. Furthermore, the perception of cervical cancer preventability was a significant factor. Only 5.10 percentage of women who believed cervical cancer could be prevented had the disease, whereas 23.08 percentage of those who did not believe in its preventability were diagnosed. This underscores the need for comprehensive educational campaigns to improve understanding of cervical cancer prevention, including vaccination against HPV and the benefits of regular screening. Family history emerged as a profound risk factor, with a striking 81.82 percentage of women with a family history of cervical cancer being diagnosed with the disease. This suggests a strong genetic predisposition and highlights the importance of targeted interventions for high-risk groups, including genetic counseling and more frequent screening [21]. The findings of this study are consistent with previous research conducted in other parts of Nigeria and sub-Saharan Africa. For instance, a study by Okunowo et al. [14] in Lagos, Nigeria, found that cervical cancer prevalence was higher among older women, particularly those with lower educational levels and those residing in rural areas. Similarly, Akinyemiju et al. [29] reported that women with low awareness and knowledge of cervical cancer were more likely to be diagnosed with the disease.
However, this study diverges from some reports regarding the role of marital status. While previous studies have indicated that married women are at a higher risk due to prolonged sexual activity and potential exposure to HPV [28], this study found a higher prevalence among divorced or widowed women. This could be attributed to the socioeconomic challenges and healthcare access issues faced by these groups in Southeast Nigeria, suggesting the need for targeted interventions. Additionally, the role of family history as a risk factor is more pronounced in this study compared to others, which have often focused more on behavioral and environmental factors. The strong association between family history and cervical cancer in this study calls for further investigation into genetic factors contributing to cervical cancer in this population.
Conclusion
Awareness of cervical cancer is relatively low among women in Southeast Nigeria, with significant gaps in knowledge regarding preventive measures. The prevalence of cervical cancer in this population highlights the need for enhanced awareness campaigns and access to screening services. Targeted interventions are essential to reduce the burden of cervical cancer in this region.
Implications for Public Health and Recommendations
The findings of this study underscore the urgent need for improved public health strategies targeting cervical cancer prevention in Southeast Nigeria. Educational interventions are crucial to increase awareness of cervical cancer, HPV, and the importance of regular screening. Efforts should be particularly focused on older women, those with lower educational attainment, and those residing in rural areas. Moreover, the healthcare system should be strengthened to ensure better access to cervical cancer screening and treatment services, especially in rural communities. Mobile health units and community-based interventions could play a significant role in reaching underserved populations. Finally, the high prevalence of cervical cancer among women with a family history of the disease suggests that genetic counselling and targeted screening programs could be beneficial. Policymakers should consider integrating genetic risk assessments into cervical cancer prevention strategies to identify and support high-risk individuals.
References
- World Health Organization (WHO). (2021). Cervical cancer. World Health Organization.
Publisher | Google Scholor - Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. (2019). Global cancer observatory: Cancer today. International Agency for Research on Cancer.
Publisher | Google Scholor - International Agency for Research on Cancer (IARC). (2021). Cervical cancer estimated incidence, mortality and prevalence worldwide in 2020. Global Cancer Observatory.
Publisher | Google Scholor - Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. (2021). Human papillomavirus and related diseases in the world.
Publisher | Google Scholor - Eze JN, Obiechina HN, Ejikeme BN, Ikeme AC, Onyebuchi AK. (2022). Epidemiology of human papillomavirus infection in Nigerian women: A meta-analysis. BMC Public Health, 22(1):839.
Publisher | Google Scholor - Akinlotan M, Bolin JN, Helduser JW, Ojinnaka C, Lichorad A, McClellan DA. (2020). Cervical cancer screening barriers and risk factor knowledge among uninsured women. Journal of Community Health, 45(4):715-726.
Publisher | Google Scholor - Odetunde OA, Osadebe OC, Anyichie AM, Onwuameze OE, Uchenna IJ. (2021). Knowledge, attitude, and uptake of human papillomavirus vaccination among women in South-Eastern Nigeria. BMC Public Health, 21(1):1823.
Publisher | Google Scholor - Okeke TC, Onyekwelu PI, Ikeako LC, Ezenyeaku CC. (2020). Prevalence and pattern of cervical cancer among women in Enugu, Southeast Nigeria. Nigerian Journal of Clinical Practice, 23(4):523-529.
Publisher | Google Scholor - Umeh CC, Ogwueleka OR, Mbakwem OP. (2021). Determinants of cervical cancer screening uptake among Nigerian women: A systematic review. Nigerian Medical Journal, 62(2):68-75.
Publisher | Google Scholor - Ezirim, E. O., Anele, D. O., Okite, U. P., Abali, I. O., Akwuruoha, E. M., Onyemereze, C. O., Omole, O. R., & Airaodion, A. I. (2024). Awareness, Prevalence and Severity of Anaemia and Related Contributing Factors, among Pregnant Women Attending Antenatal Clinic in a Teaching Hospital in Southern Nigeria. Asian Journal of Pregnancy and Childbirth, 7(1):38-52.
Publisher | Google Scholor - Airaodion AI, Ijioma CE, Ejikem PI, Abali IO, Aminu-Ayinde OE, Ogwu CI, Kalesanwo EA, Amuta AC, Areh JE, Odarah JE, Onyeukwu N, Nwokocha VC, Ogbonna UJ, Ogor VE. (2023). Prevalence of Erectile Dysfunction in Men with Type 2 Diabetes Mellitus in Osun State, Nigeria. Direct Res. J. Agric. Food Sci, 10(6): 45-52.
Publisher | Google Scholor - Omosun, A., Abayomi, A., Ogboye, O., Lajide, D., Oladele, D., Popoola, A., Banjo, A. A., Chugani, B., Mabadeje, B., Abdur-Razaak, H., Wellington, O., Andu, L., Adepase, A., Adesina, F., Olonire, O., Fetuga, A., Onasanya, O., Awosika, F., Folarin-Williams, O., & Anya, S. E. (2022). Distribution of cancer and cancer screening and treatment services in Lagos: A 10-year review of hospital records. JCO Global Oncology, 8.
Publisher | Google Scholor - Ezechi OC, Petters IT, Okeke PN. (2022). Cervical cancer awareness and prevention practices among women attending a tertiary healthcare facility in Southwest Nigeria. Afr J Reprod Health, 26(1):118-126.
Publisher | Google Scholor - Okunowo AA, Daramola ES, Okunade KS. (2021). Cervical cancer screening uptake among women in Lagos, Nigeria: Implications for public health intervention. J Public Health Afr, 12(1):1361.
Publisher | Google Scholor - Oche MO, Kaoje AU, Gana GJ. (2019). Misconceptions and attitudes towards cervical cancer screening among women in Sokoto, Nigeria. Niger J Med, 28(3):230-236.
Publisher | Google Scholor - Ifeanyi E, Anunobi C, Osondu C. (2020). Knowledge, attitude, and practice of cervical cancer screening among women in Onitsha, Southeast Nigeria. Trop Med Int Health, 25(7):801-810.
Publisher | Google Scholor - Adebamowo CA, Adekunle F, Ajayi O. (2021). Awareness of HPV infection and vaccine and willingness to vaccinate among female students at a Nigerian university. J Cancer Educ, 36(2):300-307.
Publisher | Google Scholor - Akanbi O, Oche M, Lawal I. (2022). Symptom awareness and cervical cancer screening uptake among women in rural Nigeria. BMC Public Health, 22(1):654-667.
Publisher | Google Scholor - Idowu A, Olajide SF, Ibrahim RA. (2020). Governmental and non-governmental efforts towards reducing cervical cancer in Nigeria. Afr J Med Med Sci, 49(2):115-121.
Publisher | Google Scholor - Eze JN, Umeora OU, Obuna JA, Egwuatu VE, Ejikeme BN. (2017). Cervical cancer awareness and cervical screening uptake at the Mater Misericordiae Hospital, Afikpo, Southeast Nigeria. Ann Afr Med, 16(4):167-173.
Publisher | Google Scholor - Adebamowo CA, Adewole IF, Ajayi OI, Obajimi MO, Lawal A. (2018). Knowledge, attitudes, and practices related to cervical cancer among adult women in Lagos, Nigeria. J Cancer Epidemiol, 1-7.
Publisher | Google Scholor - Owoeye IO, Ibrahim IA. (2013). Knowledge and attitude towards cervical cancer screening among female students and staff in a tertiary institution in Ilorin, Nigeria. J Prev Med Hyg, 54(3):160-163.
Publisher | Google Scholor - Bae JM, Kim EH. (2016). Family history of cervical cancer and risk of cervical cancer: A meta-analysis of observational studies. Asian Pac J Cancer Prev, 17(4):2101-2106.
Publisher | Google Scholor - Anorlu RI. (2008). Cervical cancer: The sub-Saharan African perspective. Reprod Health Matters, 16(32):41-49.
Publisher | Google Scholor - Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin, 68(6):394-424.
Publisher | Google Scholor - Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. (2013). The causal relation between human papillomavirus and cervical cancer. J Clin Pathol, 55(4):244-265.
Publisher | Google Scholor - Castellsagué X, Díaz M, de Sanjosé S, Muñoz N, Herrero R, Franceschi S, et al. (2006). Worldwide human papillomavirus etiology of cervical adenocarcinoma and its cofactors: Implications for screening and prevention. J Natl Cancer Inst, 98(5):303-315.
Publisher | Google Scholor - Akinyemiju T. (2012). Socio-economic and health access determinants of breast and cervical cancer screening in low-income countries: Analysis of the World Health Survey. PLoS One, 7(11).
Publisher | Google Scholor - Ngugi CW, Sayed AR, Mwachiro MM, Mbakaya C, Bukusi EA, Ngugi PM. (2012). Awareness and uptake of HIV testing among young people in Kenya. J Hum Virol Retrovirol, 1(2):14-21.
Publisher | Google Scholor - World Health Organization (WHO). (2023). Digital health: A strategy for enhancing public health. World Health Organization Report, 1-45.
Publisher | Google Scholor